J Breast Cancer.
2012 Sep;15(3):350-355. 10.4048/jbc.2012.15.3.350.
Oncoplastic Reconstruction with Superior Based Lateral Breast Rotation Flap after Lower Quadrant Tumor Resection
- Affiliations
-
- 1Department of Surgery, Research Institute for Medical Science, Chungnam National University College of Medicine, Daejeon, Korea. kimjr@cnu.ac.kr
- 2Department of Pathology, Research Institute for Medical Science, Chungnam National University College of Medicine, Daejeon, Korea.
- KMID: 2286462
- DOI: http://doi.org/10.4048/jbc.2012.15.3.350
Abstract
- PURPOSE
Poor cosmetic outcome have been reported as a result of breast cancer operation due to lower quadrant breast tumors; this is particularly true for women with small, firm breasts. Herein, we report here on the use of superior based lateral breast rotation flap reconstruction to improve cosmetic outcome in patients with lower quadrant breast cancer.
METHODS
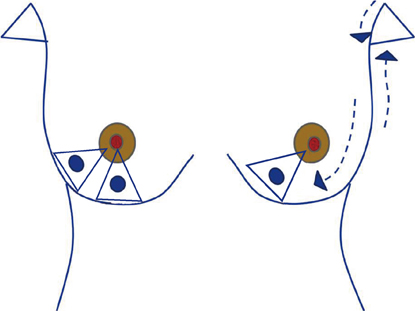
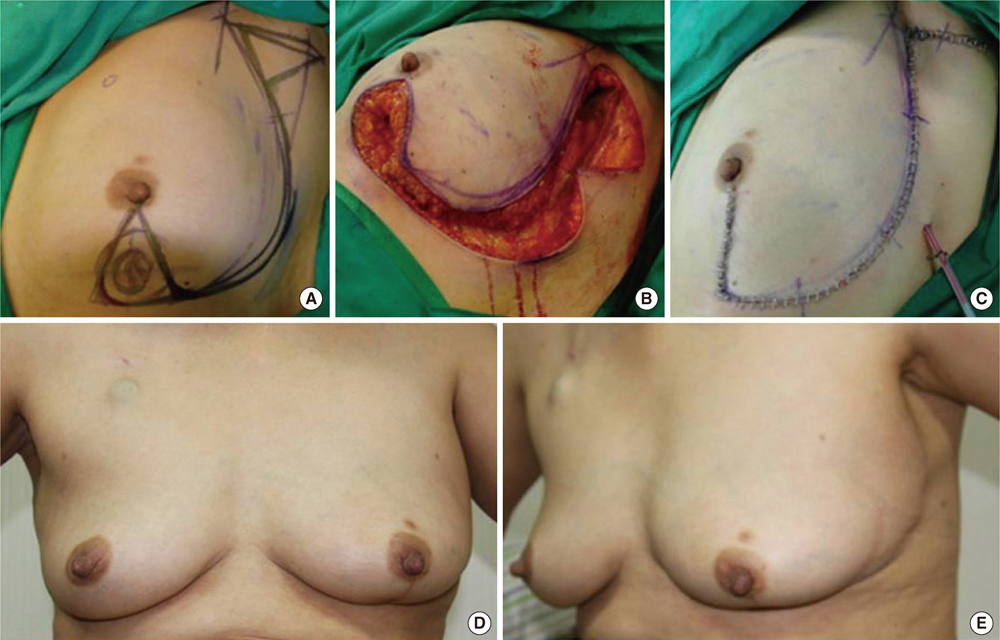
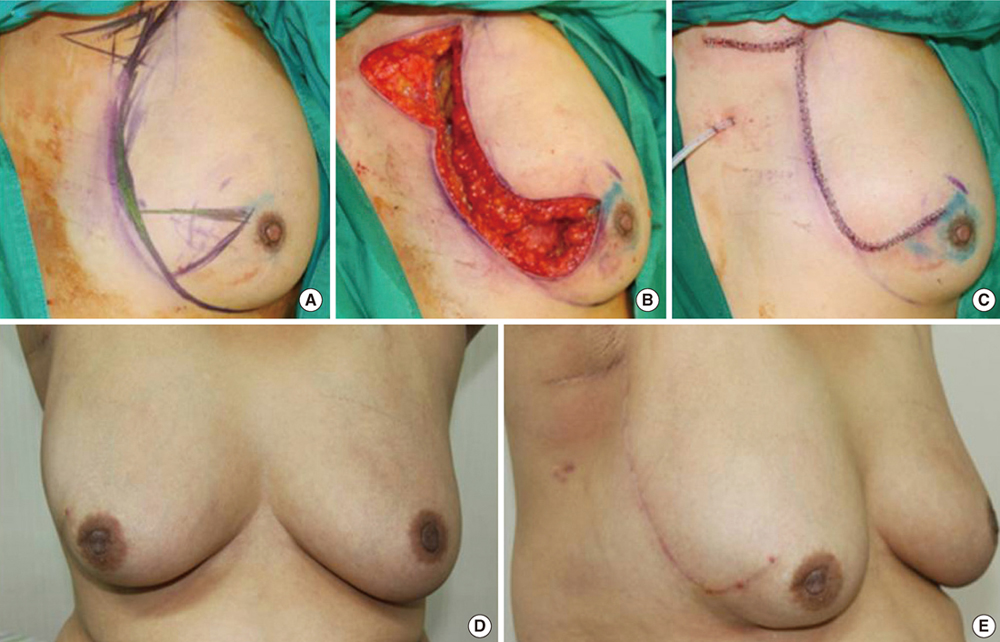
We enrolled 33 patients with invasive breast cancer located in the lower quadrant of the breast, which were located more than 2 cm apart from the nipple. After completing a quadrantectomy, a single S-shaped or reverse S-shaped incision was made from axilla to tumor site. Two triangular skin islands, one on the axilla and one overlying the tumor were marked for excision. Once the fibroglandular tissues and the additional fatty tissue of the lateral chest wall were appropriately mobilized, the breast defect was closed at the mid-point of the parenchymal thickness in order to keep the natural position of the infra mammary fold.
RESULTS
Median tumor size was 2.3 cm (range, 0.7-3.5 cm) and median resected volume was 35.5 g (range, 27.0-51.0 g). With a mean follow-up of 24.5 months (range, 9.0-33.5 months), cosmetic outcomes were good (94.0%) to fair (6.0%) at 6 months after the procedure, and there was no local or systemic recurrence during the short term follow-up period.
CONCLUSION
Clearly, this type of rotation flap reconstruction is an oncologically safe and a cosmetically sound procedure. Hopefully this rotation flap reconstruction technique will become more widely available and perhaps a standard procedure for lower quadrant breast tumors, especially for cosmetic treatment of small to medium-sized breasts.
Keyword
MeSH Terms
Figure
Reference
-
1. Amano G, Ohuchi N, Ishibashi T, Ishida T, Amari M, Satomi S. Correlation of three-dimensional magnetic resonance imaging with precise histopathological map concerning carcinoma extension in the breast. Breast Cancer Res Treat. 2000. 60:43–55.
Article2. Holland R, Hendriks JH, Vebeek AL, Mravunac M, Schuurmans Stekhoven JH. Extent, distribution, and mammographic/histological correlations of breast ductal carcinoma in situ. Lancet. 1990. 335:519–522.
Article3. de Andrade Urban C. New classification for oncoplastic procedures in surgical practice. Breast. 2008. 17:321–322.
Article4. Anderson BO, Masetti R, Silverstein MJ. Oncoplastic approaches to partial mastectomy: an overview of volume-displacement techniques. Lancet Oncol. 2005. 6:145–157.
Article5. Kronowitz SJ, Kuerer HM, Buchholz TA, Valero V, Hunt KK. A management algorithm and practical oncoplastic surgical techniques for repairing partial mastectomy defects. Plast Reconstr Surg. 2008. 122:1631–1647.
Article6. Tan M. Additional considerations in the application of oncoplastic approaches. Lancet Oncol. 2005. 6:355–356.
Article7. Jakes RW, Duffy SW, Ng FC, Gao F, Ng EH. Mammographic parenchymal patterns and risk of breast cancer at and after a prevalence screen in Singaporean women. Int J Epidemiol. 2000. 29:11–19.
Article8. Steeves RA, Phromratanapongse P, Wolberg WH, Tormey DC. Cosmesis and local control after irradiation in women treated conservatively for breast cancer. Arch Surg. 1989. 124:1369–1373.
Article9. Bartelink H, Horiot JC, Poortmans P, Struikmans H, Van den Bogaert W, Barillot I, et al. Recurrence rates after treatment of breast cancer with standard radiotherapy with or without additional radiation. N Engl J Med. 2001. 345:1378–1387.
Article10. Petit JY, Garusi C, Greuse M, Rietiens M, Youssef O, Luini A, et al. One hundred and eleven cases of breast conservation treatment with simultaneous reconstruction at the European Institute of Oncology (Milan). Tumori. 2002. 88:41–47.11. Losken A, Styblo TM, Carlson GW, Jones GE, Amerson BJ. Management algorithm and outcome evaluation of partial mastectomy defects treated using reduction or mastopexy techniques. Ann Plast Surg. 2007. 59:235–242.
Article12. Clough KB, Lewis JS, Couturaud B, Fitoussi A, Nos C, Falcou MC. Oncoplastic techniques allow extensive resections for breast-conserving therapy of breast carcinomas. Ann Surg. 2003. 237:26–34.
Article13. Newman LA, Kuerer HM, McNeese MD, Hunt KK, Gurtner GC, Vlastos GS, et al. Reduction mammoplasty improves breast conservation therapy in patients with macromastia. Am J Surg. 2001. 181:215–220.
Article14. Spear SL, Pelletiere CV, Wolfe AJ, Tsangaris TN, Pennanen MF. Experience with reduction mammaplasty combined with breast conservation therapy in the treatment of breast cancer. Plast Reconstr Surg. 2003. 111:1102–1109.
Article15. Clough KB, Nos C, Salmon RJ, Soussaline M, Durand JC. Conservative treatment of breast cancers by mammaplasty and irradiation: a new approach to lower quadrant tumors. Plast Reconstr Surg. 1995. 96:363–370.
Article16. Asgeirsson KS, Rasheed T, McCulley SJ, Macmillan RD. Oncological and cosmetic outcomes of oncoplastic breast conserving surgery. Eur J Surg Oncol. 2005. 31:817–823.
Article17. Nos C, Fitoussi A, Bourgeois D, Fourquet A, Salmon RJ, Clough KB. Conservative treatment of lower pole breast cancers by bilateral mammoplasty and radiotherapy. Eur J Surg Oncol. 1998. 24:508–514.
Article18. Dewar JA, Benhamou S, Benhamou E, Arriagada R, Petit JY, Fontaine F, et al. Cosmetic results following lumpectomy, axillary dissection and radiotherapy for small breast cancers. Radiother Oncol. 1988. 12:273–280.
Article19. Munshi A, Kakkar S, Bhutani R, Jalali R, Budrukkar A, Dinshaw KA. Factors influencing cosmetic outcome in breast conservation. Clin Oncol (R Coll Radiol). 2009. 21:285–293.
Article20. Oden S, Thureau S, Baron M, Hanzen C. Conservative treatment for breast cancer: optimization of the tumor bed localization. Cancer Radiother. 2010. 14:96–102.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Surgical Techniques for Personalized Oncoplastic Surgery in Breast Cancer Patients with Small- to Moderate-Sized Breasts (Part 2): Volume Replacement
- Oncoplastic Breast Surgery
- Oncoplastic Surgical Techniques for Personalized Breast Conserving Surgery in Breast Cancer Patient with Small to Moderate Sized Breast
- Scar Wars: Preferences in Breast Surgery
- External Oblique Myocutaneous Flap for Reconstruction of Large Chest-Wall Defects following Resection of Advanced Breast Cancer