Healthc Inform Res.
2010 Dec;16(4):305-311. 10.4258/hir.2010.16.4.305.
Implementation of Chest X-ray Observation Report Entry System
- Affiliations
-
- 1Biomedical Information Technology Center, Keimyung University, Daegu, Korea.
- 2Department of Biomedical Engineering, Keimyung University School of Medicine, Daegu, Korea.
- 3Department of Medical Informatics, Keimyung University School of Medicine, Daegu, Korea.
- 4Department of Internal Medicine, Keimyung University School of Medicine, Daegu, Korea. ynkim@dsmc.or.kr
- 5Institute of Medical Information, MDware Co. Ltd., Daegu, Korea.
- KMID: 2284544
- DOI: http://doi.org/10.4258/hir.2010.16.4.305
Abstract
OBJECTIVES
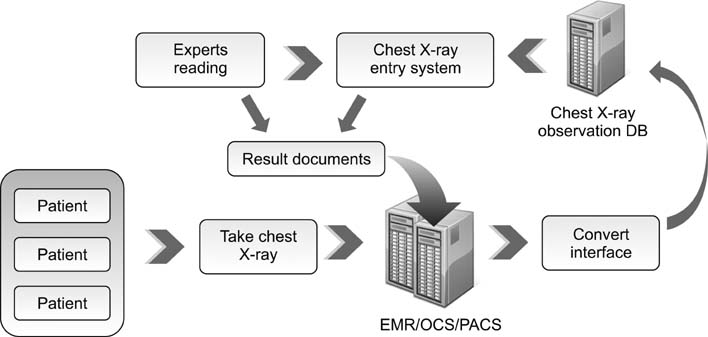
X-rays are widely used in medical examinations. In particular, chest X-rays are the most frequent imaging test. However, observations are usually recorded in a free-text format. Therefore, it is difficult to standardize the information provided to construct a database for the sharing of clinical data. Here, we describe a simple X-ray observation entry system that can interlock with an electronic medical record system.
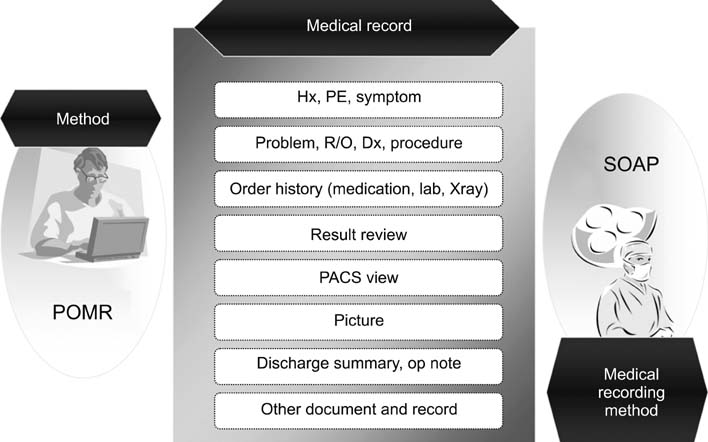
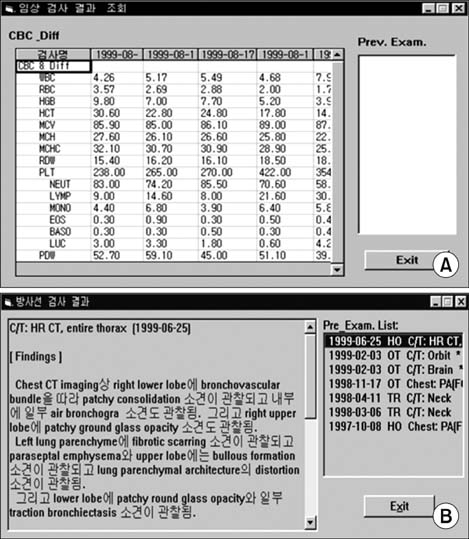
METHODS
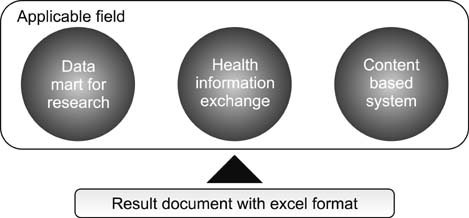
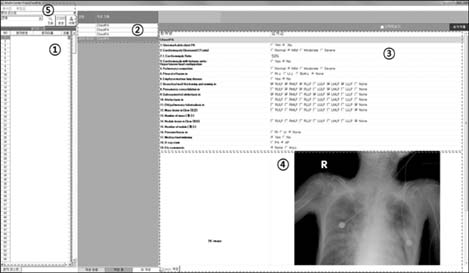
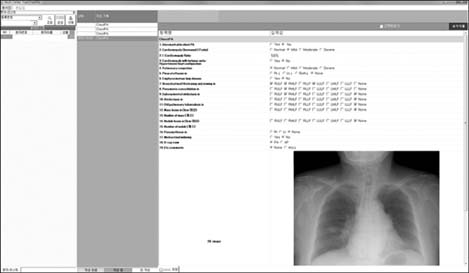
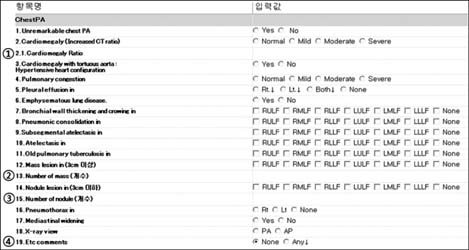
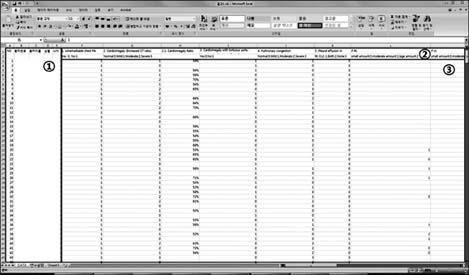
We investigated common diagnosis indices. Based on the indices, we have designed an entry system which consists of 5 parts: 1) patient lists, 2) image selection, 3) diagnosis result entry, 4) image view, and 5) main menu. The X-ray observation results can be extracted in an Excel format.
RESULTS
The usefulness of the proposed system was assessed in a study using over 500 patients' chest X-ray images. The data was readily extracted in a format that allowed convenient assessment.
CONCLUSIONS
We proposed the chest X-ray observation entry system. The proposed X-ray observation system, which can be linked with an electronic medical record system, allows easy extraction of standardized clinical information to construct a database. However, the proposed entry system is limited to chest X-rays and it is impossible to interpret the semantic information. Therefore, further research into domains using other interpretation methods is required.
Keyword
Figure
Reference
-
1. Röntgen W. Über eine neue art von strahlen. Sitzungsberichte der Physikalisch-Medicinisch Gesellschaft zu Würzburg. 1895. 132–141.2. Anderson D, Flynn K. Picture archiving and communication systems: a systematic review of published studies of diagnostic accuracy, radiology work processes, outcomes of care, and cost. Technology Assessment Program: Report no. 5. 1997. Boston, MA: Veterans Health Administration's Office of Research and Development.3. Whittick D, Gill S. Diagnostic imaging electronic health record (DI/EHR) challenges-strategy and planning perspective. In : 24th International EuroPACS Conference; 2006 June 15-17; Trondheim, Norway.4. Hripcsak G, Friedman C, Alderson PO, DuMouchel W, Johnson SB, Clayton PD. Unlocking clinical data from narrative reports: a study of natural language processing. Ann Intern Med. 1995. 122:681–688.
Article5. Koehler SB. Symtext: a natural language understanding system for encoding free text medical data [dissertation]. 1998. Salt Lake, UT: The University of Utah.6. Meystre S, Haug PJ. Automation of a problem list using natural language processing. BMC Med Inform Decis Mak. 2005. 5:30.
Article7. Leslie H, Heard S, Garde S, McNicoll I. Engaging clinicians in clinical content: herding cats or piece of cake? Stud Health Technol Inform. 2009. 150:125–129.8. Beale T, Heard S. OpenEHR release 1.0.1: archetype definitions and principles [Internet]. c2003-2007. cited at 2010 Dec 10. London: The OpenEHR Foundation;Available from: http://www.openehr.org/svn/specification/TRUNK/publishing/architecture/am/archetype_principles.pdf.9. Garde S, Knaup P, Hovenga E, Heard S. Towards semantic interoperability for electronic health records. Methods Inf Med. 2007. 46:332–343.
Article10. Bernstein K, Tvede I, Petersen J, Bredegaard K. Can openEHR archetypes be used in a national context? The Danish archetype proof-of-concept project. Stud Health Technol Inform. 2009. 150:147–151.11. Lapata M, Keller F. The Web as a baseline: evaluating the performance of unsupervised web-based models for a range of NLP tasks. Proceedings of the Human Language Technology Conference of the North American Chapter of the Association for Computational Linguistics: HLT-NAACL 2004. 2004. 2004 May 2-7; Boston, MA. Human Language Technology Conference/North American Chapter of the Association for Computational Linguistics.12. Charniak E, Knight K, Yamada K. Syntax-based language models for statistical machine translation. Proceedings of MT Summit IX. 2005. 2003 Sept 23-27; New Orleans, LA: International Association for Machine Translation.13. Clinical knowledge manager [Internet]. OpenEHR Foundation. c2010. cited at 2010 Dec 14. London, UK: OpenEHR Foundation;Available from: http://www.openehr.org/knowledge.14. Bernstein K, Andersen U. Managing care pathways combining SNOMED CT, archetypes and an electronic guideline system. Stud Health Technol Inform. 2008. 136:353–358.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Implementation of Deep Learning in ThoracicRadiology: Potential Applications and Challenges
- Automated Reporting System Using Structured Data Entry: Application to Prostate US
- Diagnostic Value of Thoracography in Pneumothorax
- Properative chest x-ray findings in peptic ulcer perforation
- Improved Reporting Rate of Notifiable Communicable Diseases through a Disease Code-Based Surveillance and In-House Electronic Reporting System