Clin Nutr Res.
2014 Jan;3(1):33-38. 10.7762/cnr.2014.3.1.33.
Relationship of Delayed Parenteral Nutrition Protocol with the Clinical Outcomes in a Medical Intensive Care Unit
- Affiliations
-
- 1Department of Nutrition and Dietetics, Severance Hospital, Yonsei University Health System, Seoul 120-752, Korea.
- 2Department of Internal Medicine, Yonsei University College of Medicine, Seoul 120-752, Korea. YSAMKIM@yuhs.ac
- 3Department of Pain and Anesthesiology, Yonsei University College of Medicine, Seoul 120-752, Korea.
- KMID: 2279619
- DOI: http://doi.org/10.7762/cnr.2014.3.1.33
Abstract
- Although parenteral nutrition (PN) is an important treatment for patients who are unable to tolerate enteral nutrition (EN), recent international guidelines recommended that PN should be reserved and initiated only after 7 days in well-nourished patients. This retrospective study was conducted to analyze the effect on clinical outcomes of a PN protocol with PN starting 4 days after admission to the intensive care unit (ICU). Eighty-one patients who were admitted from January to March of 2012 were included in the pre-protocol group, and 74 patients who were admitted from April to June of 2012 were included in the post-protocol group. There were no significant differences between the two groups when the age, gender, and admission Acute Physiology and Chronic Health Evaluation (APACHE) II scores were compared. Significantly fewer patients in the post-protocol group were provided PN (58.1% vs. 81.3%, p = 0.002), which was initiated significantly later than in the pre-protocol group (2.7 +/- 2.2 days vs. 1.9 +/- 2.0 days, p = 0.046). Five patients (6.2%) in the pre-protocol group acquired central line-associated bloodstream infection (CLA-BSI) in the ICU, yet none of the patients in the post-protocol group developed CLA-BSI (p = 0.03). The duration of antibiotic therapy and ICU stay were significantly shorter in the post-protocol group than in the pre-protocol group. By delaying initiation of PN, short-term clinical outcomes including incidence of CLA-BSI, antibiotic use, and ICU stay might be improved. Further research should be conducted to investigate the long-term effects of the decreased nutrient intake resulting from delayed PN.
MeSH Terms
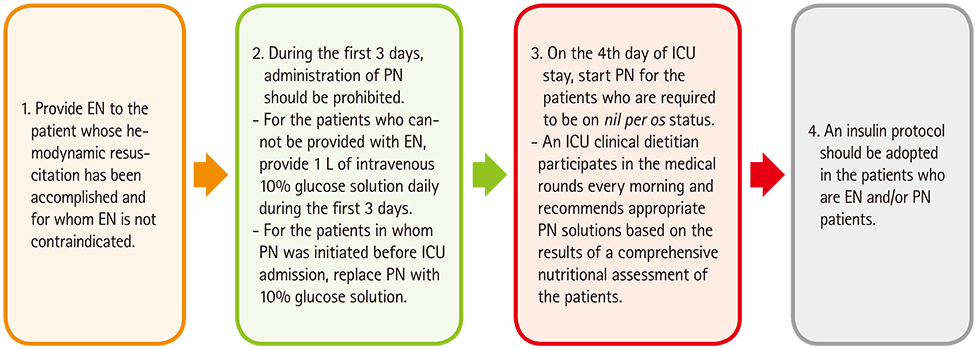
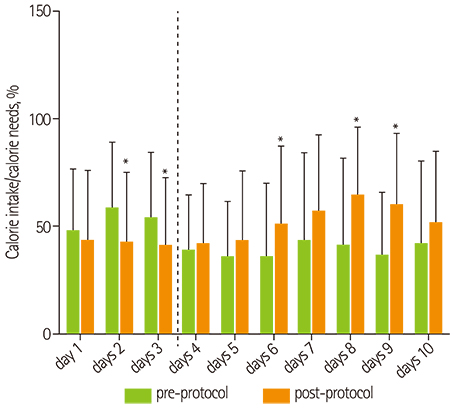
Figure
Reference
-
1. Btaiche IF, Khalidi N. Metabolic complications of parenteral nutrition in adults, Part 2. Am J Health Syst Pharm. 2004; 61:2050–2057.
Article2. Btaiche IF, Khalidi N. Metabolic complications of parenteral nutrition in adults, part 1. Am J Health Syst Pharm. 2004; 61:1938–1949.
Article3. Singer P, Berger MM, Van den Berghe G, Biolo G, Calder P, Forbes A, Griffiths R, Kreyman G, Leverve X, Pichard C. ESPEN Guidelines on parenteral nutrition: intensive care. Clin Nutr. 2009; 28:387–400.
Article4. McClave SA, Martindale RG, Vanek VW, McCarthy M, Roberts P, Taylor B, Ochoa JB, Napolitano L, Cresci G. A.S.P.E.N. Board of Directors. American College of Critical Care Medicine. Society of Critical Care Medicine. Guidelines for the provision and assessment of nutrition support therapy in the adult critically Ill patient: society of critical care medicine (SCCM) and american society for parenteral and enteral nutrition (A.S.P.E.N.). JPEN J Parenter Enteral Nutr. 2009; 33:277–316.
Article5. Casaer MP, Mesotten D, Hermans G, Wouters PJ, Schetz M, Meyfroidt G, Van Cromphaut S, Ingels C, Meersseman P, Muller J, Vlasselaers D, Debaveye Y, Desmet L, Dubois J, Van Assche A, Vanderheyden S, Wilmer A, Van den Berghe G. Early versus late parenteral nutrition in critically ill adults. N Engl J Med. 2011; 365:506–517.
Article6. Heidegger CP, Berger MM, Graf S, Zingg W, Darmon P, Costanza MC, Thibault R, Pichard C. Optimisation of energy provision with supplemental parenteral nutrition in critically ill patients: a randomised controlled clinical trial. Lancet. 2013; 381:385–393.
Article7. Vincent JL, Preiser JC. When should we add parenteral to enteral nutrition? Lancet. 2013; 381:354–355.
Article8. van der Kooi TI, Wille JC, van Benthem BH. Catheter application, insertion vein and length of ICU stay prior to insertion affect the risk of catheter-related bloodstream infection. J Hosp Infect. 2012; 80:238–244.
Article9. Lin LY, Lin HC, Lee PC, Ma WY, Lin HD. Hyperglycemia correlates with outcomes in patients receiving total parenteral nutrition. Am J Med Sci. 2007; 333:261–265.
Article10. Beghetto MG, Victorino J, Teixeira L, de Azevedo MJ. Parenteral nutrition as a risk factor for central venous catheter-related infection. JPEN J Parenter Enteral Nutr. 2005; 29:367–373.
Article11. Pasero D, De Rosa FG, Rana NK, Fossati L, Davi A, Rinaldi M, Di Perri G, Ranieri VM. Candidemia after cardiac surgery in the intensive care unit: an observational study. Interact Cardiovasc Thorac Surg. 2011; 12:374–378.
Article12. Stratman RC, Martin CA, Rapp RP, Berger R, Magnuson B. Candidemia incidence in recipients of parenteral nutrition. Nutr Clin Pract. 2010; 25:282–289.
Article13. Jarvis WR. Selected aspects of the socioeconomic impact of nosocomial infections: morbidity, mortality, cost, and prevention. Infect Control Hosp Epidemiol. 1996; 17:552–557.
Article14. Hu B, Tao L, Rosenthal VD, Liu K, Yun Y, Suo Y, Gao X, Li R, Su D, Wang H, Hao C, Pan W, Saunders CL. Device-associated infection rates, device use, length of stay, and mortality in intensive care units of 4 Chinese hospitals: International Nosocomial Control Consortium findings. Am J Infect Control. 2013; 41:301–306.
Article15. Kübler A, Duszynska W, Rosenthal VD, Fleischer M, Kaiser T, Szewczyk E, Barteczko-Grajek B. Device-associated infection rates and extra length of stay in an intensive care unit of a university hospital in Wroclaw, Poland: International Nosocomial Infection Control Consortium's (INICC) findings. J Crit Care. 2012; 27:105.e5–105.e10.
Article16. Villet S, Chiolero RL, Bollmann MD, Revelly JP, Cayeux R, Delarue J, Berger MM. Negative impact of hypocaloric feeding and energy balance on clinical outcome in ICU patients. Clin Nutr. 2005; 24:502–509.
Article17. Lee H, Koh SO, Park MS. Higher dextrose delivery via TPN related to the development of hyperglycemia in non-diabetic critically ill patients. Nutr Res Pract. 2011; 5:450–454.
Article18. Dissanaike S, Shelton M, Warner K, O'Keefe GE. The risk for bloodstream infections is associated with increased parenteral caloric intake in patients receiving parenteral nutrition. Crit Care. 2007; 11:R114.
Article19. Doig GS, Simpson F, Sweetman EA, Finfer SR, Cooper DJ, Heighes PT, Davies AR, O'Leary M, Solano T, Peake S. Early PN Investigators of the ANZICS Clinical Trials Group. Early parenteral nutrition in critically ill patients with short-term relative contraindications to early enteral nutrition: a randomized controlled trial. JAMA. 2013; 309:2130–2138.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Nutrition Therapy in Critically Ill Patients
- Current Guidelines on Clinical Nutrition in Intensive Care Units Based on ESPEN 2018
- Nutrition therapy in the intensive care unit
- Efficacy of Parenteral Nutrition with Intravenous L-alanyl-L-glutamine (Dipeptiven Inj) in Intensive Care Unit Patients
- Nutritional Support in Critically Ill Surgical Patients