Korean J Pain.
2015 Jan;28(1):22-31. 10.3344/kjp.2015.28.1.22.
Comparative Study of the Effects of the Retrocrural Celiac Plexus Block Versus Splanchnic Nerve Block, C-arm Guided, for Upper Gastrointestinal Tract Tumors on Pain Relief and the Quality of Life at a Six-month Follow Up
- Affiliations
-
- 1Department of Anesthesia and Pain Relief, Tanta Cancer Institute, Tanta, Egypt.
- 2Department of Anesthesia and Surgical Intensive Care, Faculty of Medicine, Tanta University, Tanta, Egypt. yasser.amr@gmail.com
- KMID: 2278249
- DOI: http://doi.org/10.3344/kjp.2015.28.1.22
Abstract
- BACKGROUND
The celiac plexus and splanchnic nerves are targets for neurolytic blocks for pain relief from pain caused by upper gastrointestinal tumors. Therefore, we investigated the analgesic effect of a celiac plexus block versus a splanchnic nerve block and the effects of these blocks on the quality of life six months post-intervention for patients with upper GIT tumors.
METHODS
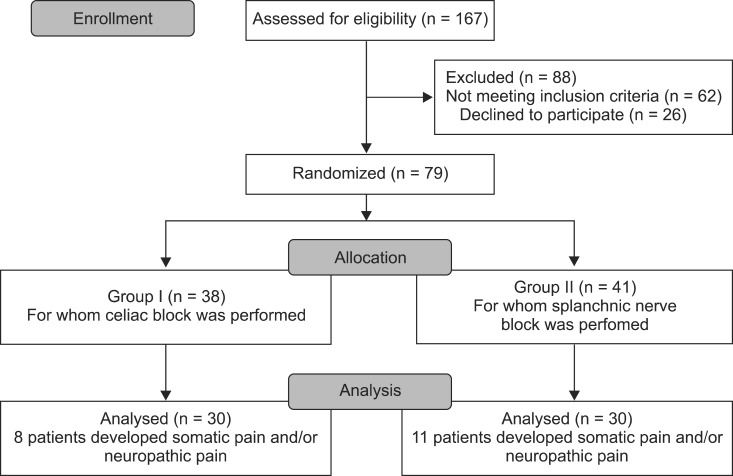
Seventy-nine patients with inoperable upper GIT tumors and with severe uncontrolled visceral pain were randomized into two groups. These were Group I, for whom a celiac plexus block was used with a bilateral needle retrocrural technique, and Group II, for whom a splanchnic nerve block with a bilateral needle technique was used. The visual analogue scale for pain (0 to 100), the quality of life via the QLQ-C30 questionnaire, and survival rates were assessed.
RESULTS
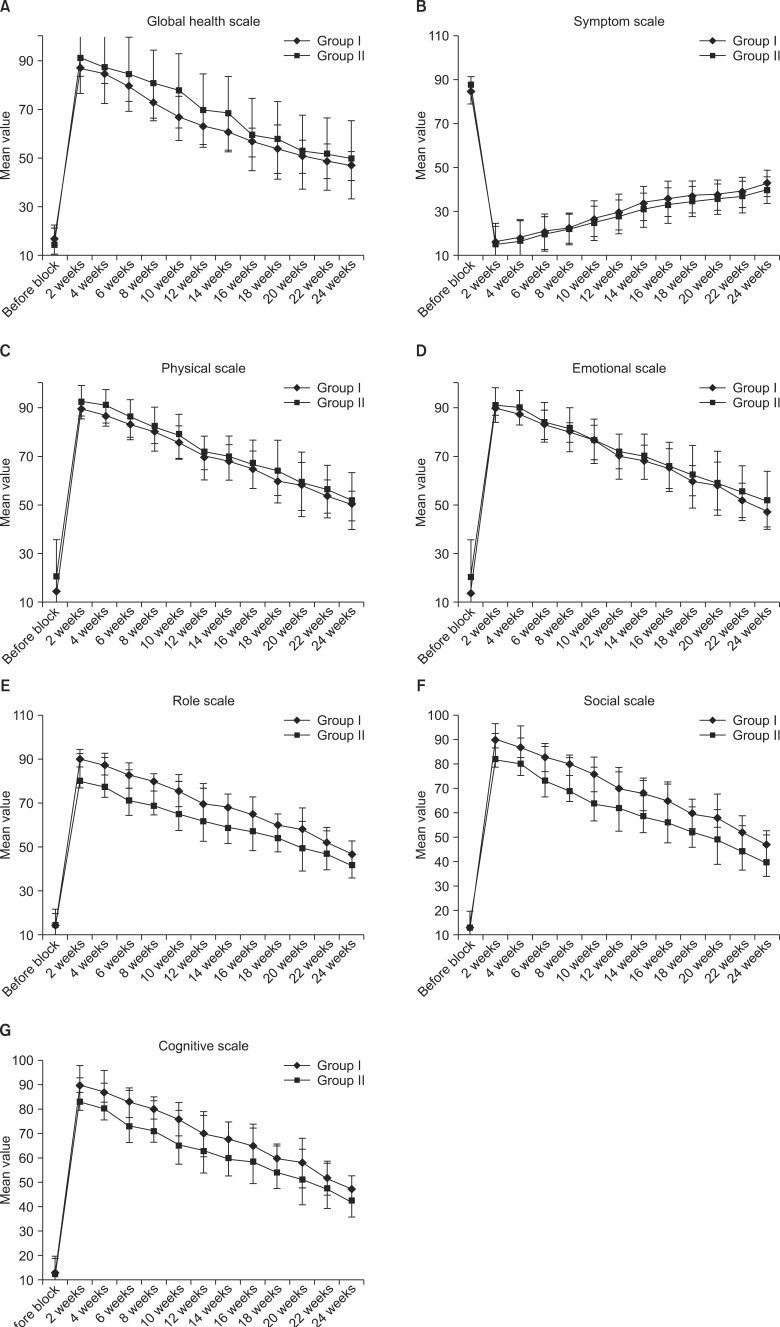
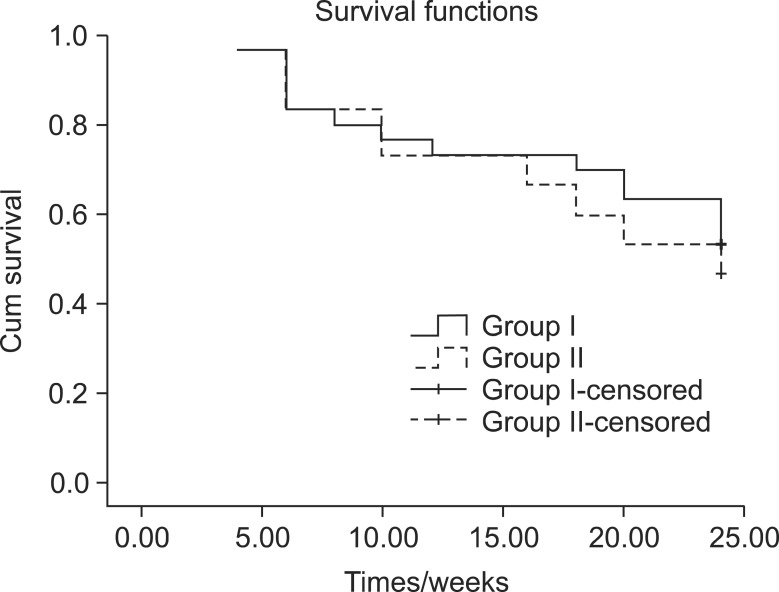
Pain scores were comparable in both groups in the first week after the block. Significantly more patients retained good analgesia with tramadol in the splanchnic group from 16 weeks onwards (P = 0.005, 0.001, 0.005, 0.001, 0.01). Social and cognitive scales improved significantly from the second week onwards in the splanchnic group. Survival of both groups was comparable.
CONCLUSIONS
The results of this study demonstrate that the efficacy of the splanchnic nerve block technique appears to be clinically comparable to a celiac block. All statistically significant differences are of little clinical value.
Keyword
MeSH Terms
-
Abdominal Pain
Analgesia
Autonomic Nerve Block
Celiac Plexus*
Follow-Up Studies*
Gastrointestinal Neoplasms
Humans
Needles
Nerve Block
Pain Measurement
Quality of Life*
Surveys and Questionnaires
Splanchnic Nerves*
Survival Rate
Tramadol
Treatment Outcome
Upper Gastrointestinal Tract*
Visceral Pain
Weights and Measures
Tramadol
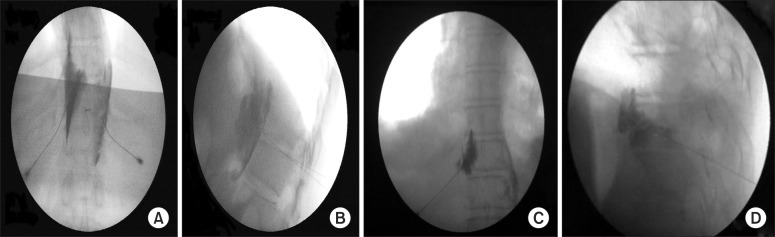
Figure
Cited by 2 articles
-
Transient paraplegia after neurolytic splanchnic block in a patient with metastatic colon carcinoma
Gonca Oguz, Gulcin Senel, Nesteren Kocak
Korean J Pain. 2018;31(1):50-53. doi: 10.3344/kjp.2018.31.1.50.Splanchnic nerve neurolysis via the transdiscal approach under fluoroscopic guidance: a retrospective study
Zhenhua Cai, Xiaolin Zhou, Mengli Wang, Jiyu Kang, Mingshuo Zhang, Huacheng Zhou
Korean J Pain. 2022;35(2):202-208. doi: 10.3344/kjp.2022.35.2.202.
Reference
-
1. Caraceni A, Portenoy RK. Pain management in patients with pancreatic carcinoma. Cancer. 1996; 78:639–653. PMID: 8681303.
Article2. Serlin RC, Mendoza TR, Nakamura Y, Edwards KR, Cleeland CS. When is cancer pain mild, moderate or severe? Grading pain severity by its interference with function. Pain. 1995; 61:277–284. PMID: 7659438.
Article3. de Oliveira R, dos Reis MP, Prado WA. The effects of early or late neurolytic sympathetic plexus block on the management of abdominal or pelvic cancer pain. Pain. 2004; 110:400–408. PMID: 15275792.
Article4. Firdousi FH, Sharma D, Raina VK. Palliation by coeliac plexus block for upper abdominal visceral cancer pain. Trop Doct. 2002; 32:224–226. PMID: 12405303.
Article5. Mercadante S, Catala E, Arcuri E, Casuccio A. Celiac plexus block for pancreatic cancer pain: factors influencing pain, symptoms and quality of life. J Pain Symptom Manage. 2003; 26:1140–1147. PMID: 14654266.
Article6. Bouhassira D, Attal N, Alchaar H, Boureau F, Brochet B, Bruxelle J, et al. Comparison of pain syndromes associated with nervous or somatic lesions and development of a new neuropathic pain diagnostic questionnaire (DN4). Pain. 2005; 114:29–36. PMID: 15733628.
Article7. Aaronson NK, Ahmedzai S, Bergman B, Bullinger M, Cull A, Duez NJ, et al. The European Organization for Research and Treatment of Cancer QLQ-C30: a quality-of-life instrument for use in international clinical trials in oncology. J Natl Cancer Inst. 1993; 85:365–376. PMID: 8433390.
Article8. Lawlor P, Turner K, Hanson J, Bruera E. Dose ratio between morphine and hydromorphone in patients with cancer pain: a retrospective study. Pain. 1997; 72:79–85. PMID: 9272790.
Article9. Breitbart W, Chandler S, Eagel B, Ellison N, Enck RE, Lefkowitz M, et al. An alternative algorithm for dosing transdermal fentanyl for cancer-related pain. Oncology (Williston Park). 2000; 14:695–705. PMID: 10853461.10. Goudas L, Carr DB, Bloch R, Balk E, Ioannidis JP, Terrin N, et al. Management of cancer pain. Evid Rep Technol Assess (Summ). 2001; 1–5. PMID: 11253288.11. Noble M, Gress FG. Techniques and results of neurolysis for chronic pancreatitis and pancreatic cancer pain. Curr Gastroenterol Rep. 2006; 8:99–103. PMID: 16533471.
Article12. Okuyama M, Shibata T, Morita T, Kitada M, Tukahara Y, Fukushima Y, et al. A comparison of intraoperative celiac plexus block with pharmacological therapy as a treatment for pain of unresectable pancreatic cancer. J Hepatobiliary Pancreat Surg. 2002; 9:372–375. PMID: 12353149.
Article13. Loukas M, Klaassen Z, Merbs W, Tubbs RS, Gielecki J, Zurada A. A review of the thoracic splanchnic nerves and celiac ganglia. Clin Anat. 2010; 23:512–522. PMID: 20235178.
Article14. Peterson PK, Molitor TW, Chao CC. The opioid-cytokine connection. J Neuroimmunol. 1998; 83:63–69. PMID: 9610674.
Article15. Kawamata M, Ishitani K, Ishikawa K, Sasaki H, Ota K, Omote K, et al. Comparison between celiac plexus block and morphine treatment on quality of life in patients with pancreatic cancer pain. Pain. 1996; 64:597–602. PMID: 8783327.
Article16. Stefaniak T, Basinski A, Vingerhoets A, Makarewicz W, Connor S, Kaska L, et al. A comparison of two invasive techniques in the management of intractable pain due to inoperable pancreatic cancer: neurolytic celiac plexus block and videothoracoscopic splanchnicectomy. Eur J Surg Oncol. 2005; 31:768–773. PMID: 15923103.
Article17. Lillemoe KD, Cameron JL, Kaufman HS, Yeo CJ, Pitt HA, Sauter PK. Chemical splanchnicectomy in patients with unresectable pancreatic cancer. A prospective randomized trial. Ann Surg. 1993; 217:447–455. PMID: 7683868.
Article18. Cherry DA, Lamberty J. Paraplegia following coeliac plexus block. Anaesth Intensive Care. 1984; 12:59–61. PMID: 6703318.
Article19. Stafford B. More complications of coeliac plexus blockade. Aust N Z J Med. 1991; 21:782–783. PMID: 1759933.
Article20. Davies DD. Incidence of major complications of neurolytic coeliac plexus block. J R Soc Med. 1993; 86:264–266. PMID: 8505748.
Article21. Sastre B, Carabalona B, Crespy B, Delpero JR, Sielezneff I, Michotey G. Transhiatal bilateral splanchnicotomy for pain control in pancreatic cancer: basic anatomy, surgical technique, and immediate results in fifty-one cases. Surgery. 1992; 111:640–646. PMID: 1375785.22. Raj PP, Thomas J, Heavner J, Racz G, Lou L, Day M, et al. The development of a technique for radiofrequency lesioning of splanchnic nerves. Curr Rev Pain. 1999; 3:377–387. PMID: 10998694.
Article23. Saenz A, Kuriansky J, Salvador L, Astudillo E, Cardona V, Shabtai M, et al. Thoracoscopic splanchnicectomy for pain control in patients with unresectable carcinoma of the pancreas. Surg Endosc. 2000; 14:717–720. PMID: 10954816.
Article24. Süleyman Ozyalçin N, Talu GK, Camlica H, Erdine S. Efficacy of coeliac plexus and splanchnic nerve blockades in body and tail located pancreatic cancer pain. Eur J Pain. 2004; 8:539–545. PMID: 15531222.
Article25. Marra V, Debernardi F, Frigerio A, Menna S, Musso L, Di Virgilio MR. Neurolytic block of the celiac plexus and splanchnic nerves with computed tomography. The experience in 150 cases and an optimization of the technic. Radiol Med. 1999; 98:183–188. PMID: 10575450.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Splanchnic Nerve Block at T12 Level
- Radiofrequency Thermocoagulation of Splanchnic Nerve in Patients with Upper Abdominal Pain
- CT Guided Celiac Plexus and Splanchnic Nerve Neurolysis: The Modified Anterior Approach
- CT-guided alcohol block of the celiac plexus: The abterior approach
- Follow up Observation after Splanchnic Nerve Block