Cancer Res Treat.
2005 Jun;37(3):177-182.
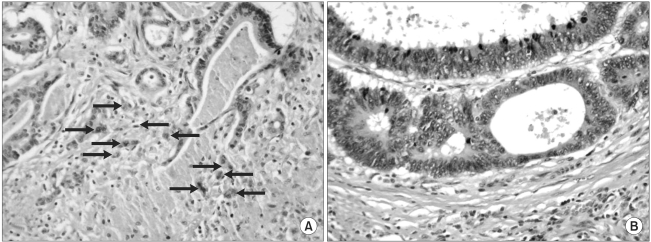
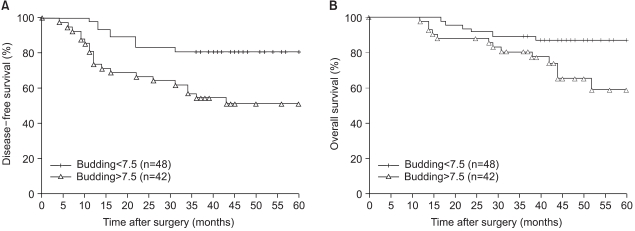
Intensity of Tumor Budding as an Index for the Malignant Potential in Invasive Rectal Carcinoma
- Affiliations
-
- 1Department of Surgery, Dong-A University College of Medicine, Busan, South Korea. colonch@donga.ac.kr
- 2Department of Internal Medicine, Dong-A University College of Medicine, Busan, South Korea.
- 3Department of Pathology, Dong-A University College of Medicine, Busan, South Korea.
Abstract
- PURPOSE
The aim of this study was to quantitatively assess the intensity of tumor budding in rectal carcinoma and to determine how it correlates with the malignant potential. MATERIALS AND METHODS: Intensities of the tumor budding at the invasive front of the surgical specimens from 90 patients (male, 51) with well- or moderately- differentiated rectal carcinoma were investigated. Differences in the budding intensity among pathologic variables were compared, and recurrences and survivals were analyzed in accordance with degree of the budding intensity. The patients ranged in age from 33 to 75 years (mean, 55.4) with the median follow-up being 43 months (range, 12~108). RESULTS: Tumor budding was identified in 89 patients (98.9%) with a mean intensity of 7.5+/-5.3. The budding intensity was significantly higher in tumors with lymphatic invasion (p=0.0081), blood vessel invasion (p<0.0001), and perineural invasion (p=0.0013) than in those tumor without these findings. It became significantly higher with the increase in nodal stage (p<0.0001). The intensity of tumor budding in patients with relapse (29 patients) was significantly higher than that in patients without relapse (6.2+/-5.0 vs. 10.2+/-4.9; p=0.0005), but this difference in the intensity was observed only for the node-positive patients (8.0+/-3.4 vs. 11.9+/-5.1; p=0.0064). When the patients were stratified into two groups on either side of the mean of the intensity, the higher intensity group showed a significantly less favorable disease- free (DFS) and overall survival (OS) (p=0.0026 and 0.0205, respectively). Based on the multivariate analysis, the nodal stage and the intensity of budding proved to be the independent variables associated with DFS (p=0.023 and 0.03, respectively). CONCLUSION: Tumor budding at the invasive margin is a reliable pathologic index that indicates a higher malignant potential and a less favorable prognosis for patients with advanced rectal carcinoma.
Keyword
Figure
Reference
-
1. Morodomi T, Isomoto H, Shirouzu K, Kakegawa K, Irie K, Morimatsu M. An index for estimating the probability of lymph node metastasis in rectal cancers. Lymph node metastasis and the histopathology of actively invasive regions of cancer. Cancer. 1989; 63:539–543. PMID: 2912530.
Article2. Hase K, Shatney C, Johnson D, Trollope M, Vierra M. Prognostic value of tumor "budding" in patients with colorectal cancer. Dis Colon Rectum. 1993; 36:627–635. PMID: 8348847.
Article3. Okuyama T, Oya M, Ishikawa H. Budding as a useful prognostic marker in pT3 well- or moderately-differentiated rectal adenocarcinoma. J Surg Oncol. 2003; 83:42–47. PMID: 12722096.
Article4. Ueno H, Murphy J, Jass JR, Mochizuki H, Talbot IC. Tumour 'budding' as an index to estimate the potential of aggressiveness in rectal cancer. Histopathology. 2002; 40:127–132. PMID: 11952856.
Article5. Tanaka M, Hashiguchi Y, Ueno H, Hase K, Mochizuki H. Tumor budding at the invasive margin can predict patients at high risk of recurrence after curative surgery for stage II, T3 colon cancer. Dis Colon Rectum. 2003; 46:1054–1059. PMID: 12907899.
Article6. Okuyama T, Oya M, Ishikawa H. Budding as a risk factor for lymph node metastasis in pT1 or pT2 well-differentiated colorectal adenocarcinoma. Dis Colon Rectum. 2002; 45:628–634. PMID: 12004212.
Article7. Jass JR, Sobin LH. Histologic typing of intestinal tumors. WHO international histological classification of tumors. 1989. 2th ed. Berlin: Springer-Verlag.8. Dukes CE. The classification of cancer of the rectum. J Pathol Bacteriol. 1932; 35:323–332.
Article9. Mantel N. Evaluation of survival data and two new rank order statistics arising in its consideration. Cancer Chemother Rep. 1966; 50:163–170. PMID: 5910392.10. Cox DR. Regression models and life tables. J R Stat Soc. 1972; 34:187–220.11. Imai T. The growth of human carcinoma: a morphological analysis. Fukuoka Igaku Zasshi. 1954; 45:72–102.12. Hase K, Shatney CH, Mochizuki H, Johnson DL, Tamakuma S, Vierra M, Trollope M. Long-term results of curative resection of "minimally invasive" colorectal cancer. Dis Colon Rectum. 1995; 38:19–26. PMID: 7813339.
Article13. Teixeira CR, Tanaka S, Haruma K, Yoshihara M, Sumii K, Kajiyama G, et al. Carcinoembryonic antigen staining patterns at the invasive tumor margin predict the malignant potential of colorectal carcinoma. Oncology. 1994; 51:228–233. PMID: 7515172.
Article14. Frost P, Levin B. Clinical implications of metastatic process. Lancet. 1992; 339:1458–1461. PMID: 1351135.
Article15. Masaki T, Matsuoka H, Sugiyama M, Abe N, Izumisato Y, Sakamoto A, et al. Laminin-5 γ2 chain expression as a possible determinant of tumor aggressiveness in T1 colorectal carcinomas. Dig Dis Sci. 2003; 48:272–278. PMID: 12643602.16. Masaki T, Goto A, Sugiyama M, Matsuoka H, Abe N, Sakamoto A, et al. Possible contribution of CD44 variant 6 and nuclear beta-catenin expression to the formation of budding tumor cells in patients with T1 colorectal carcinoma. Cancer. 2001; 92:2539–2546. PMID: 11745187.17. Masaki T, Sugiyama M, Matsuoka H, Abe N, Izumisato Y, Sakamoto A, et al. Coexpression of matrilysin and laminin-5 gamma2 chain may contribute to tumor cell migration in colorectal carcinomas. Dig Dis Sci. 2003; 48:1262–1267. PMID: 12870781.18. Sordat I, Rousselle P, Chaubert P, Petermann O, Aberdam D, Bosman FT, et al. Tumor cell budding and laminin-5 expression in colorectal carcinoma can be modulated by the tissue micro-environment. Int J Cancer. 2000; 88:708–717. PMID: 11072238.
Article19. Simon R, Altman DG. Statistical aspects of prognostic factor studies in oncology. Br J Cancer. 1994; 69:979–985. PMID: 8198989.
Article20. Okuyama T, Oya M, Yamaguchi M. Budding (sprouting) as a useful prognostic marker in colorectal mucinous carcinoma. Jpn J Clin Oncol. 2002; 32:412–416. PMID: 12451038.
Article21. Ueno H, Price AB, Wilkinson KH, Jass JR, Mochizuki H, Talbot IC. A new prognostic staging system for rectal cancer. Ann Surg. 2004; 240:832–839. PMID: 15492565.
Article22. Wang HS, Liang WY, Lin TC, Chen WS, Jiang JK, Yang SH, et al. Curative resection of T1 colorectal carcinoma: risk of lymph node metastasis and long-term prognosis. Dis Colon Rectum. 2005; 3. 24. DOI: 10.1007/s10350-004-0935-y.
Article23. Bleday R, Breen E, Jessup JM, Burgess A, Sentovich SM, Steele G Jr. Prospective evaluation of local excision for small rectal cancers. Dis Colon Rectum. 1997; 40:388–392. PMID: 9106685.
Article24. Garcia-Aguilar J, Pollack J, Lee SH, Hernandez de Anda E, Mellgren A, Wong WD, et al. Accuracy of endorectal ultrasonography in preoperative staging of rectal tumors. Dis Colon Rectum. 2002; 45:10–15. PMID: 11786756.
Article25. Orrom WJ, Wong WD, Rothenberger DA, Jensen LL, Goldberg SM. Endorectal ultrasound in the preoperative staging of rectal tumors. A learning experience. Dis Colon Rectum. 1990; 33:654–659. PMID: 2198147.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Tumor budding in invasive breast carcinoma and its association with clinicopathological parameters: an experience from a tertiary care center in India
- Expression of E-cadherin and beta-catenin is Altered at Tumor Budding Sites, Whose Number is Associated with the Progression of Colorectal Carcinoma
- Tumor Budding and Recurrence in Submucosal Invasive Colorectal Cancers of Favorable Histology: Case Reports of Two Early Colorectal Cancers with Advanced Recurrences
- Histologically confirmed distant metastatic urothelial carcinoma from the urinary bladder: a retrospective review of one institution’s 20-year experience
- Clinicopathologic Factors for Prediction of Lymph Node Metastasis in Submucosally Invasive Colorectal Carcinoma