Ann Rehabil Med.
2014 Dec;38(6):791-798. 10.5535/arm.2014.38.6.791.
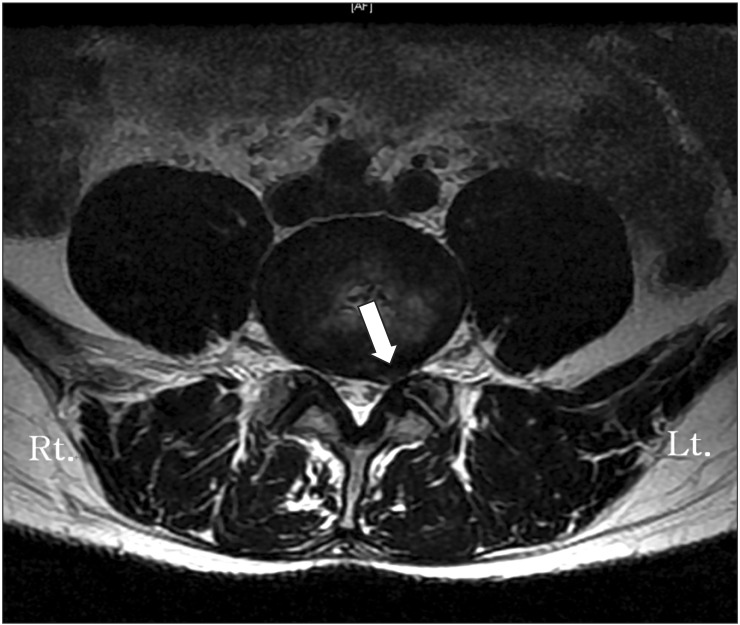
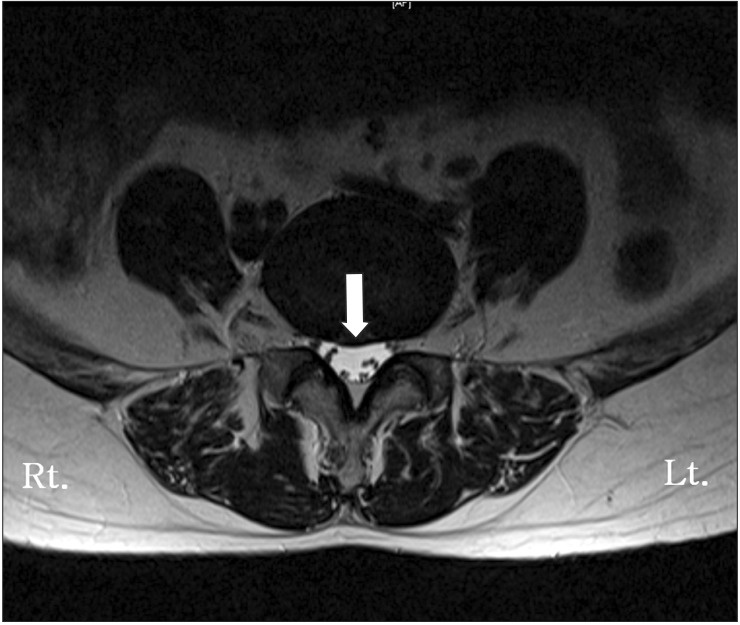
Use of Magnetic Resonance Imaging to Identify Outcome Predictors of Caudal Epidural Steroid Injections for Lower Lumbar Radicular Pain Caused by a Herniated Disc
- Affiliations
-
- 1Department of Rehabilitation Medicine, Gangnam Severance Hospital, Seoul, Korea. RMPJH@yuhs.ac
- 2Rehabilitation Institute of Neuromuscular Disease, Yonsei University College of Medicine, Seoul, Korea.
- KMID: 2267089
- DOI: http://doi.org/10.5535/arm.2014.38.6.791
Abstract
OBJECTIVE
We used lumbar magnetic resonance image (MRI) findings to determine possible outcome predictors of a caudal epidural steroid injection (CESI) for radicular pain caused by a herniated lumbar disc (HLD).
METHODS
Ninety-one patients with radicular pain whose MRI indicated a HLD were enrolled between September 2010 and July 2013. The CESIs were performed using ultrasound (US). A responder was defined as having complete relief or at least a 50% reduction of pain as assessed by the visual analog scale (VAS) and functional status on the Roland Morris Disability Questionnaire (RMDQ); responder (VAS n=61, RMDQ n=51), and non-responder (VAS n=30, RMDQ n=40). MRI findings were analyzed and compared between the two groups with regard to HLD level, HLD type (protrusion or exclusion), HLD zone (central, subarticular, foraminal, and extraforaminal), HLD volume (mild, moderate, or severe), relationship between HLD and nerve root (no contact, contact, displaced, or compressed), disc height loss (none, less than half, or more than half ), and disc degeneration grade (homogeneous disc structure or inhomogeneous disc structure-clear nucleus and height of intervertebral disc).
RESULTS
A centrally located herniated disc was more common in the responder group than that in the non-responder group. Treatment of centrally located herniated discs showed satisfactory results. (VAS p=0.025, RMDQ p=0.040). Other factors, such as HLD level, HLD type, HLD volume, relationship to nerve root, disc height loss, and disc degeneration grade, were not critical.
CONCLUSION
The HLD zone was significant for pain reduction after CESI. A centrally located herniated disc was a predictor of a good clinical outcome.
MeSH Terms
Figure
Reference
-
1. Nygaard OP, Mellgren SI, Osterud B. The inflammatory properties of contained and noncontained lumbar disc herniation. Spine (Phila Pa 1976). 1997; 22:2484–2488. PMID: 9383853.
Article2. Franson RC, Saal JS, Saal JA. Human disc phospholipase A2 is inflammatory. Spine (Phila Pa 1976). 1992; 17(6 Suppl):S129–S132. PMID: 1631712.
Article3. Olmarker K, Blomquist J, Stromberg J, Nannmark U, Thomsen P, Rydevik B. Inflammatogenic properties of nucleus pulposus. Spine (Phila Pa 1976). 1995; 20:665–669. PMID: 7604342.
Article4. Park Y, Lee JH, Park KD, Ahn JK, Park J, Jee H. Ultrasound-guided vs. fluoroscopy-guided caudal epidural steroid injection for the treatment of unilateral lower lumbar radicular pain: a prospective, randomized, single-blind clinical study. Am J Phys Med Rehabil. 2013; 92:575–586. PMID: 23636087.5. Hopwood MB, Abram SE. Factors associated with failure of lumbar epidural steroids. Reg Anesth. 1993; 18:238–243. PMID: 8398958.6. Sayegh FE, Kenanidis EI, Papavasiliou KA, Potoupnis ME, Kirkos JM, Kapetanos GA. Efficacy of steroid and nonsteroid caudal epidural injections for low back pain and sciatica: a prospective, randomized, double-blind clinical trial. Spine (Phila Pa 1976). 2009; 34:1441–1447. PMID: 19525834.7. Wewers ME, Lowe NK. A critical review of visual analogue scales in the measurement of clinical phenomena. Res Nurs Health. 1990; 13:227–236. PMID: 2197679.
Article8. Roland M, Morris R. A study of the natural history of back pain. Part I: development of a reliable and sensitive measure of disability in low-back pain. Spine (Phila Pa 1976). 1983; 8:141–144. PMID: 6222486.9. Roland M, Morris R. A study of the natural history of low-back pain. Part II: development of guidelines for trials of treatment in primary care. Spine (Phila Pa 1976). 1983; 8:145–150. PMID: 6222487.10. Fardon DF. Nomenclature and classification of lumbar disc pathology. Spine (Phila Pa 1976). 2001; 26:461–462. PMID: 11242371.
Article11. Pfirrmann CW, Dora C, Schmid MR, Zanetti M, Hodler J, Boos N. MR image-based grading of lumbar nerve root compromise due to disk herniation: reliability study with surgical correlation. Radiology. 2004; 230:583–588. PMID: 14699183.
Article12. Pfirrmann CW, Metzdorf A, Zanetti M, Hodler J, Boos N. Magnetic resonance classification of lumbar intervertebral disc degeneration. Spine (Phila Pa 1976). 2001; 26:1873–1878. PMID: 11568697.
Article13. Daghighi MH, Pouriesa M, Maleki M, Fouladi DF, Pezeshki MZ, Mazaheri Khameneh R, et al. Migration patterns of herniated disc fragments: a study on 1,020 patients with extruded lumbar disc herniation. Spine J. 2014; 14:1970–1977. PMID: 24361346.
Article14. Cyriax JH. Textbook of orthopaedic medicine. London: Bailliere Tindall;1882.15. Kelman H. Epidural injection therapy for sciatic pain. Am J Surg. 1944; 64:183–190.
Article16. Kantrowitz F, Robinson DR, Mcguire MB, Levine L. Corticosteroids inhibit prostaglandin production by rheumatoid synovia. Nature. 1975; 258:737–739. PMID: 1207758.
Article17. Nishimura N, Fujimaki T, Oshibuchi M, Yoshikawa I, Aida M. The distribution of solutions in the epidural space. Masui. 1991; 40:350–360. PMID: 2072487.18. Makki D, Nawabi DH, Francis R, Hamed AR, Hussein AA. Is the outcome of caudal epidural injections affected by patient positioning? Spine (Phila Pa 1976). 2010; 35:E687–E690. PMID: 20535042.
Article19. Komori H, Shinomiya K, Nakai O, Yamaura I, Takeda S, Furuya K. The natural history of herniated nucleus pulposus with radiculopathy. Spine (Phila Pa 1976). 1996; 21:225–229. PMID: 8720408.
Article20. McCarron RF, Wimpee MW, Hudkins PG, Laros GS. The inflammatory effect of nucleus pulposus. A possible element in the pathogenesis of low-back pain. Spine (Phila Pa 1976). 1987; 12:760–764. PMID: 2961088.21. Price DD, McGrath PA, Rafii A, Buckingham B. The validation of visual analogue scales as ratio scale measures for chronic and experimental pain. Pain. 1983; 17:45–56. PMID: 6226917.
Article22. Grotle M, Brox JI, Vollestad NK. Concurrent comparison of responsiveness in pain and functional status measurements used for patients with low back pain. Spine (Phila Pa 1976). 2004; 29:E492–E501. PMID: 15507789.
Article23. Ostelo RW, Deyo RA, Stratford P, Waddell G, Croft P, Von Korff M, et al. Interpreting change scores for pain and functional status in low back pain: towards international consensus regarding minimal important change. Spine (Phila Pa 1976). 2008; 33:90–94. PMID: 18165753.24. Abdi S, Datta S, Trescot AM, Schultz DM, Adlaka R, Atluri SL, et al. Epidural steroids in the management of chronic spinal pain: a systematic review. Pain Physician. 2007; 10:185–212. PMID: 17256030.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Arachnoiditis Following Caudal Epidural Injections for the Lumbo-Sacral Radicular Pain
- Cauda Equina Syndrome Following Volumetric Caudal Epidural Steroid Injection in a Herniated Interverterbral Disc Patient: A case report
- Persistent Hiccup after Epidural Steroid Injection: Case reports
- The Effective Steroid Dose of Caudal Epidural Injection with Unilateral Epidural Catheter Position in Patients with Symptomatic Herniated Nucleus Purposus
- Air Bubbles Mimic Disc Herniation in MRI after Cervical Epidural Block