Ann Rehabil Med.
2012 Feb;36(1):47-54. 10.5535/arm.2012.36.1.47.
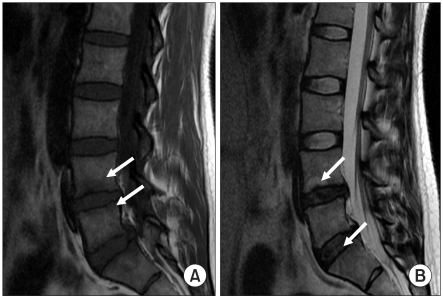
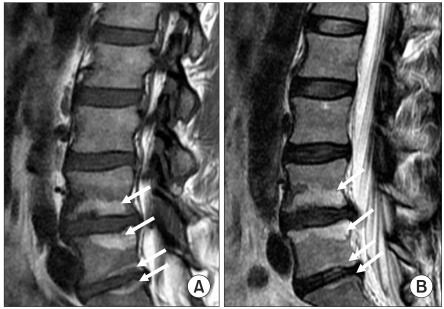
Magnetic Resonance Findings of Acute Severe Lower Back Pain
- Affiliations
-
- 1Department of Rehabilitation Medicine, Konkuk University Medical Center, Konkuk University School of Medicine, Seoul 143-729, Korea. mdlis@nate.com
- KMID: 2266780
- DOI: http://doi.org/10.5535/arm.2012.36.1.47
Abstract
OBJECTIVE
To determine abnormal MRI findings in adults hospitalized with acute severe axial LBP. METHOD: Sixty patients with back pain were divided into 3 groups consisting of 1) 23 adults with acute axial severe LBP who could not sit up or stand up for several days, but had not experienced previous back-related diseases or trauma (group A), 2) 19 adults who had been involved in a minor traffic accident, and had mild symptoms but not limited mobility (group B), and 3) 18 adults with LBP with radicular pain (group C)., Various MRI findings were assessed among the above 3 groups and compared as follows: disc herniation (protrusion, extrusion), lumbar disc degeneration (LDD), annular tear, high intensity zone (HIZ), and endplate changes.
RESULTS
The MRI findings of A group were as follows: disc herniation (87%), LDD (100%), annular tear (100%), HIZ (61%), and end plate changes (4.4%). The findings of disc herniation, annular tear, HIZ, and LDD were more prevalent in A group than in B group (p<0.01). HIZ findings were more prevalent in A group than in group B or group C (p<0.05).
CONCLUSION
Patients with acute severe axial LBP were more likely to have disc herniation, LDD, annular tear, HIZ. Among LBP groups, there was a significant association of HIZ on MRI with acute severe axial LBP.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
The Factors Associated With the Successful Outcomes of Percutaneous Disc Decompression in Patients With Lumbar Herniated Nucleus Pulposus
Sang Heon Lee, Yong Jin Jeong, Nack Hwan Kim, Hyeun Jun Park, Hyun-Joon Yoo, Soo Yung Jo
Ann Rehabil Med. 2015;39(5):735-744. doi: 10.5535/arm.2015.39.5.735.
Reference
-
1. Jarvik JG, Deyo RA. Diagnostic evaluation of low back pain with emphasis on imaging. Ann Intern Med. 2002; 137:586–597. PMID: 12353946.
Article2. Andersson GB. Epidemiological features of chronic low back pain. Lancet. 1999; 354:581–585. PMID: 10470716.3. Chou R, Qaseem A, Snow V, Casey D, Cross T Jr, Shekelle P, Owens DK. Diagnosis and treatment of low back pain: a joint clinical practice guideline from the American College of Physicians and the American Pain Society. Ann Intern Med. 2007; 147:478–491. PMID: 17909209.
Article4. Deyo RA, Rainville J, Kent DL. What can the history and physical examination tell us about low back pain? JAMA. 1992; 268:760–765. PMID: 1386391.
Article5. Bigos S, Bowyer O, Braen G, Brown K, Deyo R, Haldeman S, Hart J, Johnson E, Keller R, Kido D, et al. Acute low back pain problems in adults. Clinical Practice Guidline ns 14. AHCPR Publication No. 95-0642. 1994. 95. Rockville, MD: US Department of Health and Human Services;p. 1–60.6. Beattie PF, Meyers SP. Magnetic resonance imaging in low back pain: general principles and clinical issues. Phys Ther. 1998; 78:738–753. PMID: 9672546.
Article7. Tehranzadeh J, Andrews C, Wong E. Lumbar spine imaging. Normal variants, imaging pitfalls, and artifacts. Radiol Clin North Am. 2000; 38:1207–1253. PMID: 11131630.8. Anderson RE, Drayer BP, Braffman B, Davis PC, Deck MD, Hasso AN, Johnson BA, Masaryk T, Pomeranz SJ, Seidenwurm D, et al. Acute low back pain-radiculopathy. American College of Radiology. ACR Appropriateness Criteria. Radiology. 2000; 215:479–485. PMID: 11037459.9. Nachemson A, Vingard E. Nachemson A, Jonsson E, editors. Assessment of patients with neck and back pain: a best-evidence synthesis. Neck and back pain: the scientific evidence of causes, diagnosis, and treatment. 2000. 1st ed. Philadelphia: Lippincott Williams & Wilkins;p. 189–235.11. Fukuda KG. Proper use of MR imaging for evaluation of low back pain (radiologist' view). Semin Musculoskelet Radiol. 2001; 5:133–136. PMID: 11500154.12. Jarvik JG, Deyo RA. Imaging of lumbar intervertebral disk degeneration and aging, excluding disk herniations. Radiol Clin North Am. 2000; 38:1255–1266. PMID: 11131631.
Article13. Deyo RA. Magnetic resonance imaging of the lumbar spine. Terrific test or tar baby? N Engl J Med. 1994; 331:115–116. PMID: 8208253.14. Boden SD, Davis DO, Dina TS, Patronas NJ, Wiesel SW. Abnormal magnetic resonance scans of the lumbar spine in asymptomatic subjects. A prospective investigation. J Bone Joint Surg Am. 1990; 72:403–408. PMID: 2312537.15. Jensen MC, Brant-Zawadzki MN, Obuchowski N, Modic MT, Malkasian D, Ross JS. Magnetic resonance imaging of the lumbar spine in people withoutback pain. N Engl J Med. 1994; 331:69–73. PMID: 8208267.16. Stadnik TW, Lee RR, Coen HL, Neirynck EC, Buisseret TS, Osteaux MJ. Annular tears and disk herniation: prevalence and contrast enhancement on MR images in the absence of low back pain or sciatica. Radiology. 1998; 206:49–55. PMID: 9423651.
Article17. Carragee E, Alamin T, Cheng I, Franklin T, Hurwitz E. Does minor trauma cause serious low back illness? Spine. 2006; 31:2942–2949. PMID: 17139225.
Article18. Carragee E, Alamin T, Cheng I, Franklin T, van den Haak E, Hurwitz E. Are first-time episodes of serious LBP associated with new MRI findings? Spine J. 2006; 6:624–635. PMID: 17088193.
Article19. Aprill C, Bogduk N. High intensity zone: a diagnostic sign of painful lumbar disc on magnetic resonance imaging. Br J Radiol. 1992; 65:361–369. PMID: 1535257.20. Pfirrmann CW, Metzdorf A, Zanetti M, Hodler J, Boss N. Magnetic resonance classification of lumbar intervertebral disc degeneration. Spine. 2001; 26:1873–1878. PMID: 11568697.
Article21. Takatalo J, Karppinen J, Niinimaki J, Taimela S, Nayha S, Jarvelin MR, Kyllonen E, Tervonen O. Prevalence of degenerative imaging findings in lumbar magnetic resonance imaging among young adults. Spine. 2009; 34:1716–1721. PMID: 19770614.
Article22. Modic MT, Masaryk TJ, Ross JS, Carter JR. Imaging of degenerative disk disease. Radiology. 1988; 168:177–186. PMID: 3289089.
Article23. Modic MT, Steinberg PM, Ross JS, Masaryk TJ, Carter JR. Degenerative disk disease: assessment of changes in vertebral body marrow with MR imaging. Radiology. 1988; 166:193–199. PMID: 3336678.
Article24. Trattnig S, Stelzeneder D, Goed S, Reissegger M, Mamisch TC, Paternostro-Sluga T, Weber M, Szomolanyi P, Welsch GH. Lumbar intervertebral disc abnormalities: comparison of quantitative T2 mapping with conventional MR at 3.0T. Eur Radiol. 2010; 20:2715–2722. PMID: 20559835.
Article25. Schellhas KP, Pollei SR, Gundry CR, Heithoff KB. Lumbar disc high-intensity zone. Correlation of magnetic resonance imaging and discography. Spine. 1996; 21:79–86. PMID: 9122767.26. Saifuddin A, Mitchell R, Taylor BA. Extradural inflammation associated with annular tears: demonstration with gadoliniumenhanced lumbar spine MRI. Eur Spine J. 1999; 8:34–39. PMID: 10190852.
Article27. Lam KS, Carlin D, Mulholland RC. Lumbar disc high-intensity zone: the value and significance of provocative discography in the determination of the discogenic pain source. Eur Spine J. 2000; 9:36–41. PMID: 10766075.
Article28. Peng B, Hou S, Wu W, Zhang C, Yang Y. The pathogenesis and clinical significance of a high-intensity zone (HIZ) of lumbar intervertebral disc on MR imaging in the patient with discogenic low back pain. Eur Spine J. 2006; 15:583–587. PMID: 16047210.
Article29. Ricketson R, Simmons JW, Hauser BO. The prolapsed intervertebral disc. The high-intensity zone with discography correlation. Spine. 1996; 21:2758–2762. PMID: 8979322.30. Smith BM, Hurwitz EL, Solsberg D, Rubinstein D, Corenman DS, Dwyer AP, Kleiner J. Interobserver reliability of detecting lumbar intervertebral disc high-intensity zone on magnetic resonance imaging and association of high-intensity zone with pain and anular disruption. Spine. 1998; 23:2074–2080. PMID: 9794051.
Article31. Rankine JJ, Gill KP, Hutchinson CE, Ross ER, Williamson JB. The clinical significance of the highintensity zone on lumbar spine magnetic resonance imaging. Spine. 1999; 24:1913–1919. PMID: 10515016.
Article32. Peng B, Hou S, Wu S, Zhang C, Yang Y. The pathogenesis and clinical significance of a high-intensity zone (HIZ) of lumbar intervertebral disc on MR imaging in the patient with discogenic low back pain. Eur Spine J. 2006; 15:583–587. PMID: 16047210.
Article33. Hadjipavlou AG, Tzermiadianos MN, Bogduk N, Zindrick MR. The pathophysiology of disc degeneration a critical review. J Bone Joint Surg Br. 2008; 90:1261–1270. PMID: 18827232.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Acute Schmorl Node in Dorsal Spine: An Unusual Cause of a Sudden Onset of Severe Back Pain in a Young Female
- Spinal Nerve Root Swelling Mimicking Intervertebral Disc Herniation in Magnetic Resonance Imaging: A Case Report
- Severe Low Back Pain and Radiculopathy during Epiduroscopy
- Transabdominal Ultrasonographic Findings of Lumbar Spine-Related Lesions in Patients with Back Pain: Correlation with MRI
- A Case of Intradural Epidermoid Tumor in Lumbar Region