Ann Rehabil Med.
2013 Aug;37(4):471-478. 10.5535/arm.2013.37.4.471.
Prevalence of the Rotator Cuff Tear Increases With Weakness in Hemiplegic Shoulder
- Affiliations
-
- 1Department of Rehabilitation Medicine, Seoul National University College of Medicine, Seoul, Korea. tairyoon@snu.ac.kr
- 2Department of Rehabilitation Medicine, Kangwon National University School of Medicine, Chuncheon, Korea.
- 3Department of Rehabilitation Medicine, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
- KMID: 2266602
- DOI: http://doi.org/10.5535/arm.2013.37.4.471
Abstract
OBJECTIVE
To investigate the relationship between the rotator cuff tear (RCT) and the muscle strength in hemiplegic side, and the effects of paralysis on the affected shoulders in hemiplegic patients.
METHODS
A cross-sectional observational study performed in a university hospital was presented. The study enrolled 55 participants with hemiplegia of diverse degree of motor paresis, excluding those with bilateral lesions, history of major trauma or other co-existing musculoskeletal disorders of the shoulder. The main outcome measurements were muscle strength of the affected upper extremity (based on Medical Research Council scale), RCTs of the bilateral shoulders (by ultrasonography), and presence of shoulder pain, subluxation of the glenohumeral joint, passive range of motions, and subacromial spurs.
RESULTS
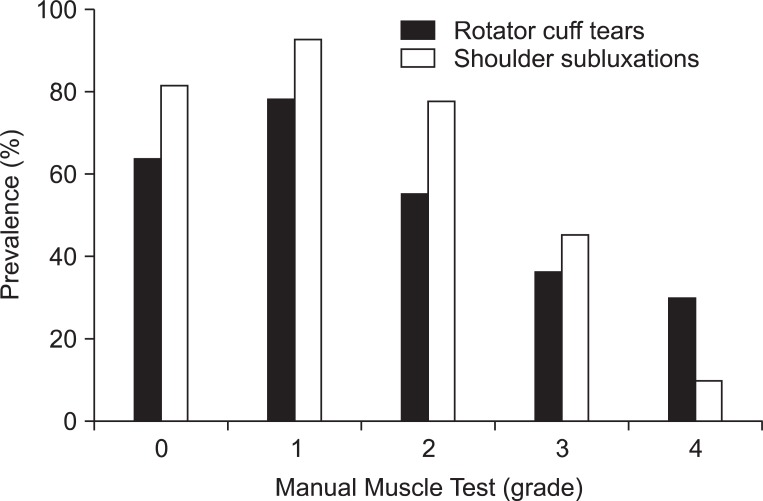
Comparing each side of the shoulders, the prevalence of shoulder pain and supraspinatus muscle tear was higher (p<0.0001, p=0.007), and the range of motion was restricted (p<0.0001, p<0.0001, p<0.0001, p<0.0001) in the affected side. There was a significant trend toward higher prevalence of RCT and shoulder subluxation in the weaker shoulder (p=0.019, p<0.0001). In a multivariate analysis, Manual Muscle Test grade of less than three was an independent risk factor for RCT (p=0.025).
CONCLUSION
RCT in hemiplegia had a linear trend with muscle weakness in the affected side and the degree of weakness was an independent risk factor for the occurrence of RCT. In addition, shoulder pain, limitation of range of motions, and RCT were more frequent on the hemiplegic side of the shoulders. It is the first study to reveal a linear trend between RCT and upper extremity weakness and will provide physicians an insight to the management of RCTs in hemiplegic patients.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Hemiplegic Shoulder Pain in Shoulder Subluxation after Stroke: Associated with Range of Motion Limitation
Sang Chul Lee, Ae Ryoung Kim, Won Hyuk Chang, Ju-sun Kim, Deog Young Kim
Brain Neurorehabil. 2018;11(1):. doi: 10.12786/bn.2018.11.e6.
Reference
-
1. Reilly P, Macleod I, Macfarlane R, Windley J, Emery RJ. Dead men and radiologists don't lie: a review of cadaveric and radiological studies of rotator cuff tear prevalence. Ann R Coll Surg Engl. 2006; 88:116–121. PMID: 16551396.
Article2. Sano H, Ishii H, Trudel G, Uhthoff HK. Histologic evidence of degeneration at the insertion of 3 rotator cuff tendons: a comparative study with human cadaveric shoulders. J Shoulder Elbow Surg. 1999; 8:574–579. PMID: 10633891.
Article3. Lindgren I, Jonsson AC, Norrving B, Lindgren A. Shoulder pain after stroke: a prospective population-based study. Stroke. 2007; 38:343–348. PMID: 17185637.4. Yu D. Shoulder pain in hemiplegia. Phys Med Rehabil Clin N Am. 2004; 15:vi–vii. 683–697. PMID: 15219895.5. Bender L, McKenna K. Hemiplegic shoulder pain: defining the problem and its management. Disabil Rehabil. 2001; 23:698–705. PMID: 11732559.6. Gilmore PE, Spaulding SJ, Vandervoort AA. Hemiplegic shoulder pain: implications for occupational therapy treatment. Can J Occup Ther. 2004; 71:36–46. PMID: 15015899.
Article7. Van Ouwenaller C, Laplace PM, Chantraine A. Painful shoulder in hemiplegia. Arch Phys Med Rehabil. 1986; 67:23–26. PMID: 3942479.8. Joynt RL. The source of shoulder pain in hemiplegia. Arch Phys Med Rehabil. 1992; 73:409–413. PMID: 1580765.9. Hakuno A, Sashika H, Ohkawa T, Itoh R. Arthrographic findings in hemiplegic shoulders. Arch Phys Med Rehabil. 1984; 65:706–711. PMID: 6497618.10. Rizk TE, Christopher RP, Pinals RS, Salazar JE, Higgins C. Arthrographic studies in painful hemiplegic shoulders. Arch Phys Med Rehabil. 1984; 65:254–256. PMID: 6712451.11. Lo SF, Chen SY, Lin HC, Jim YF, Meng NH, Kao MJ. Arthrographic and clinical findings in patients with hemiplegic shoulder pain. Arch Phys Med Rehabil. 2003; 84:1786–1791. PMID: 14669184.12. Najenson T, Yacubovich E, Pikielni SS. Rotator cuff injury in shoulder joints of hemiplegic patients. Scand J Rehabil Med. 1971; 3:131–137. PMID: 5156175.13. Nepomuceno CS, Miller JM 3rd. Shoulder arthrography in hemiplegic patients. Arch Phys Med Rehabil. 1974; 55:49–51. PMID: 4810651.14. Wolff AB, Sethi P, Sutton KM, Covey AS, Magit DP, Medvecky M. Partial-thickness rotator cuff tears. J Am Acad Orthop Surg. 2006; 14:715–725. PMID: 17148619.
Article15. Neer CS 2nd. Anterior acromioplasty for the chronic impingement syndrome in the shoulder. 1972. J Bone Joint Surg Am. 2005; 87:1399. PMID: 15930554.16. MacGillivray JD, Fealy S, Potter HG, O'Brien SJ. Multiplanar analysis of acromion morphology. Am J Sports Med. 1998; 26:836–840. PMID: 9850788.
Article17. Wang JC, Horner G, Brown ED, Shapiro MS. The relationship between acromial morphology and conservative treatment of patients with impingement syndrome. Orthopedics. 2000; 23:557–559. PMID: 10875415.
Article18. Yamaguchi K, Ditsios K, Middleton WD, Hildebolt CF, Galatz LM, Teefey SA. The demographic and morphological features of rotator cuff disease: a comparison of asymptomatic and symptomatic shoulders. J Bone Joint Surg Am. 2006; 88:1699–1704. PMID: 16882890.19. Jobe CM. Superior glenoid impingement. Orthop Clin North Am. 1997; 28:137–143. PMID: 9113710.
Article20. Blevins FT. Rotator cuff pathology in athletes. Sports Med. 1997; 24:205–220. PMID: 9327536.
Article21. Soslowsky LJ, Thomopoulos S, Tun S, Flanagan CL, Keefer CC, Mastaw J, et al. Neer Award 1999. Overuse activity injures the supraspinatus tendon in an animal model: a histologic and biomechanical study. J Shoulder Elbow Surg. 2000; 9:79–84. PMID: 10810684.
Article22. Perry SM, McIlhenny SE, Hoffman MC, Soslowsky LJ. Inflammatory and angiogenic mRNA levels are altered in a supraspinatus tendon overuse animal model. J Shoulder Elbow Surg. 2005; 14(1 Suppl S):79S–83S. PMID: 15726091.
Article23. Lohr JF, Uhthoff HK. The microvascular pattern of the supraspinatus tendon. Clin Orthop Relat Res. 1990; (254):35–38. PMID: 2323147.
Article24. Rothman RH, Parke WW. The vascular anatomy of the rotator cuff. Clin Orthop Relat Res. 1965; 41:176–186. PMID: 5832730.25. Rathbun JB, Macnab I. The microvascular pattern of the rotator cuff. J Bone Joint Surg Br. 1970; 52:540–553. PMID: 5455089.
Article26. Nakajima T, Rokuuma N, Hamada K, Tomatsu T, Fukuda H. Histologic and biomechanical characteristics of the supraspinatus tendon: reference to rotator cuff tearing. J Shoulder Elbow Surg. 1994; 3:79–87. PMID: 22959646.
Article27. Yuan J, Murrell GA, Wei AQ, Wang MX. Apoptosis in rotator cuff tendonopathy. J Orthop Res. 2002; 20:1372–1379. PMID: 12472255.
Article28. Yuan J, Murrell GA, Trickett A, Wang MX. Involvement of cytochrome c release and caspase-3 activation in the oxidative stress-induced apoptosis in human tendon fibroblasts. Biochim Biophys Acta. 2003; 1641:35–41. PMID: 12788227.
Article29. Yuan J, Murrell GA, Trickett A, Landtmeters M, Knoops B, Wang MX. Overexpression of antioxidant enzyme peroxiredoxin 5 protects human tendon cells against apoptosis and loss of cellular function during oxidative stress. Biochim Biophys Acta. 2004; 1693:37–45. PMID: 15276323.
Article30. Soslowsky LJ, Malicky DM, Blasier RB. Active and passive factors in inferior glenohumeral stabilization: a biomechanical model. J Shoulder Elbow Surg. 1997; 6:371–379. PMID: 9285877.
Article31. Ovesen J, Nielsen S. Experimental distal subluxation in the glenohumeral joint. Arch Orthop Trauma Surg. 1985; 104:78–81. PMID: 4051701.
Article32. Halder AM, Halder CG, Zhao KD, O'Driscoll SW, Morrey BF, An KN. Dynamic inferior stabilizers of the shoulder joint. Clin Biomech (Bristol, Avon). 2001; 16:138–143.
Article33. Niessen M, Janssen T, Meskers C, Koppe P, Konijnenbelt M, Veeger D. Kinematics of the contralateral and ipsilateral shoulder: a possible relationship with post-stroke shoulder pain. J Rehabil Med. 2008; 40:482–486. PMID: 18509565.
Article34. Diederichsen LP, Norregaard J, Dyhre-Poulsen P, Winther A, Tufekovic G, Bandholm T, et al. The activity pattern of shoulder muscles in subjects with and without subacromial impingement. J Electromyogr Kinesiol. 2009; 19:789–799. PMID: 19062307.
Article35. Gold GE, Pappas GP, Blemker SS, Whalen ST, Campbell G, McAdams TA, et al. Abduction and external rotation in shoulder impingement: an open MR study on healthy volunteers initial experience. Radiology. 2007; 244:815–822. PMID: 17690321.36. Pong YP, Wang LY, Wang L, Leong CP, Huang YC, Chen YK. Sonography of the shoulder in hemiplegic patients undergoing rehabilitation after a recent stroke. J Clin Ultrasound. 2009; 37:199–205. PMID: 19253350.
Article37. Kim HA, Kim SH, Seo YI. Ultrasonographic findings of painful shoulders and correlation between physical examination and ultrasonographic rotator cuff tear. Mod Rheumatol. 2007; 17:213–219. PMID: 17564776.
Article38. Yoon TS, Kim DH, Park JW, Kwon BS, Ryu KH, Lee HJ, et al. Causes of the hemiplegic shoulder pain. J Korean Acad Rehabil Med. 2010; 34:158–162.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Delaminated Rotator Cuff Tear: Concurrent Concept and Treatment
- Biological Characteristics of Rotator Cuff Tendon
- Intramuscular Cyst of the Rotator Cuff Associated with Tear of the Rotator Cuff: A Case Report
- Reverse Total Shoulder Arthroplasty in the Massive Rotator Cuff Tear
- Rotator cuff tear with joint stiffness: a review of current treatment and rehabilitation