Ann Rehabil Med.
2013 Oct;37(5):649-657. 10.5535/arm.2013.37.5.649.
Contributing Factors Analysis for the Changes of the Gross Motor Function in Children With Spastic Cerebral Palsy After Physical Therapy
- Affiliations
-
- 1Department of Rehabilitation Medicine, Bundang Jesaeng General Hospital, Seongnam, Korea. viaduct83@naver.com
- 2Department of Statistics, Seoul National University, Seoul, Korea.
- KMID: 2266582
- DOI: http://doi.org/10.5535/arm.2013.37.5.649
Abstract
OBJECTIVE
To investigate the factors which contribute to the improvements of the gross motor function in children with spastic cerebral palsy after physical therapy.
METHODS
The subjects were 45 children with spastic cerebral palsy with no previous botulinum toxin injection or operation history within 6 months. They consisted of 24 males (53.3%) and 21 females (46.7%), and the age of the subjects ranged from 2 to 6 years, with the mean age being 41+/-18 months. The gross motor function was evaluated by Gross Motor Function Measure (GMFM)-88 at the time of admission and discharge, and then, the subtractions were correlated with associated factors.
RESULTS
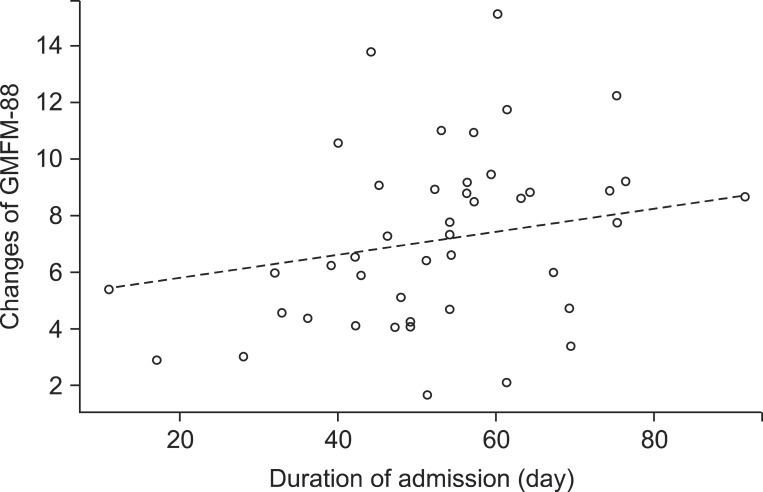
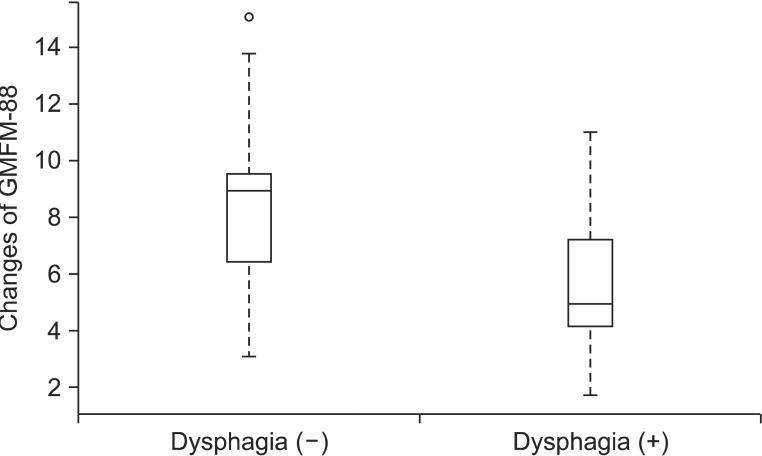
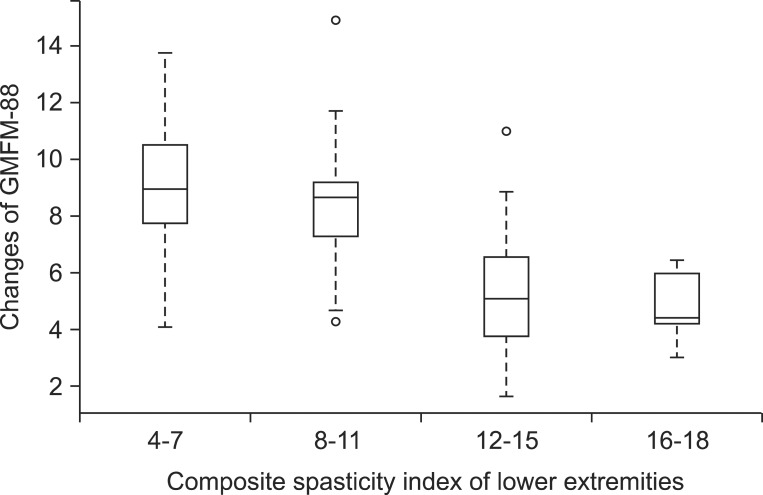
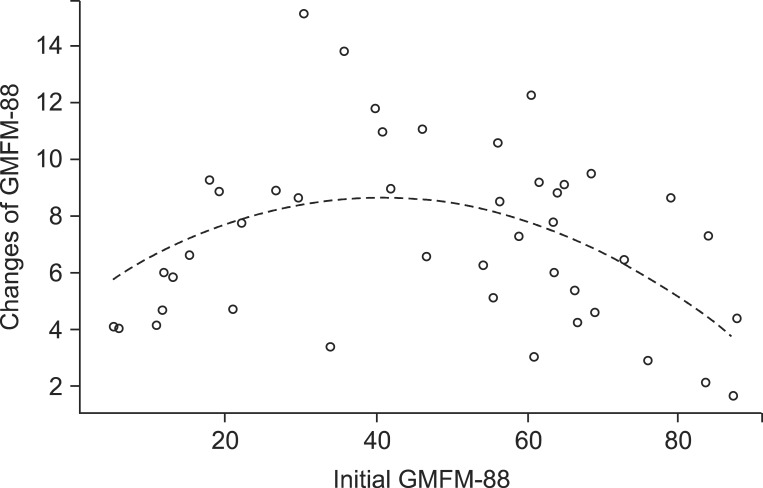
The GMFM-88 was increased by 7.17+/-3.10 through 52+/-16 days of physical therapy. The more days of admission, the more improvements of GMFM-88 were attained. The children with initial GMFM-88 values in the middle range showed more improvements in GMFM-88 (p<0.05). The children without dysphagia and children with less spasticity of lower extremities also showed more improvements in GMFM-88 (p<0.05).
CONCLUSION
We can predict the improvements of the gross motor function after physical therapy according to the days of admission, initial GMFM-88, dysphagia, and spasticity of lower extremities. Further controlled studies including larger group are necessary.
MeSH Terms
Figure
Reference
-
1. Russell DJ, Rosenbaum PL, Cadman DT, Gowland C, Hardy S, Jarvis S. The gross motor function measure: a means to evaluate the effects of physical therapy. Dev Med Child Neurol. 1989; 31:341–352. PMID: 2753238.
Article2. Ibrahim AI, Hawamdeh ZM. Evaluation of physical growth in cerebral palsied children and its possible relationship with gross motor development. Int J Rehabil Res. 2007; 30:47–54. PMID: 17293720.
Article3. Venkateswaran S, Shevell MI. Comorbidities and clinical determinants of outcome in children with spastic quadriplegic cerebral palsy. Dev Med Child Neurol. 2008; 50:216–222. PMID: 18248493.
Article4. Palisano R, Rosenbaum P, Walter S, Russell D, Wood E, Galuppi B. Development and reliability of a system to classify gross motor function in children with cerebral palsy. Dev Med Child Neurol. 1997; 39:214–223. PMID: 9183258.
Article5. Palisano RJ, Hanna SE, Rosenbaum PL, Russel DJ, Walter SD, Wood EP, et al. Validation of a model of gross motor function for children with cerebral palsy. Phys Ther. 2000; 80:974–985. PMID: 11002433.
Article6. Hidecker MJ, Ho NT, Dodge N, Hurvitz EA, Slaughter J, Workinger MS, et al. Inter-relationships of functional status in cerebral palsy: analyzing gross motor function, manual ability, and communication function classification systems in children. Dev Med Child Neurol. 2012; 54:737–742. PMID: 22715907.
Article7. Hidecker MJ, Paneth N, Rosenbaum PL, Kent RD, Lillie J, Eulenberg JB, et al. Developing and validating the Communication Function Classification System for individuals with cerebral palsy. Dev Med Child Neurol. 2011; 53:704–710. PMID: 21707596.
Article8. Ross SA, Engsberg JR. Relationships between spasticity, strength, gait, and the GMFM-66 in persons with spastic diplegia cerebral palsy. Arch Phys Med Rehabil. 2007; 88:1114–1120. PMID: 17826455.
Article9. Gorter JW, Verschuren O, van Riel L, Ketelaar M. The relationship between spasticity in young children (18 months of age) with cerebral palsy and their gross motor function development. BMC Musculoskelet Disord. 2009; 10:108. PMID: 19728891.
Article10. Park CI, Shin JS, Park ES, Lee BS, Namgung R, Park KI. Predictive value of postural reactions and neurological examinations for early diagnosis of cerebral palsy. J Korean Acad Rehabil Med. 1991; 15:22–32.11. Russell DJ, Rosenbaum PL, Avery LM, Lane M. Gross Motor Function Measure (GMFM-66 & GMFM-88) user's manual. London: Mac Keith Press;2002.12. Francis HP, Wade DT, Turner-Stokes L, Kingswell RS, Dott CS, Coxon EA. Does reducing spasticity translate into functional benefit? An exploratory meta-analysis. J Neurol Neurosurg Psychiatry. 2004; 75:1547–1551. PMID: 15489384.
Article13. Himmelmann K, Beckung E, Hagberg G, Uvebrant P. Gross and fine motor function and accompanying impairments in cerebral palsy. Dev Med Child Neurol. 2006; 48:417–423. PMID: 16700930.
Article14. Yi TI, Huh WS, Ku HK, Seo IS, Shim JW, Lee GE, et al. Nutritional status of children with cerebral palsy. J Korean Acad Rehabil Med. 2011; 35:42–47.15. Rogers B, Arvedson J, Buck G, Smart P, Msall M. Characteristics of dysphagia in children with cerebral palsy. Dysphagia. 1994; 9:69–73. PMID: 8131428.
Article16. Yuan M, Lin Y. Model selection and estimation in regression with grouped variables. J R Stat Soc Series B Stat Methodol. 2006; 68:49–67.
Article17. Tibshirani R. Regression shrinkage and selection via the Lasso. J R Stat Soc Series B Stat Methodol. 1996; 58:267–288.
Article18. Trahan J, Malouin F. Changes in the Gross Motor Function Measure in children with different types of cerebral palsy: an eight-month follow-up study. Pediatr Phys Ther. 1999; 11:12–17.19. Abel MF, Damiano DL, Blanco JS, Conaway M, Miller F, Dabney K, et al. Relationships among musculoskeletal impairments and functional health status in ambulatory cerebral palsy. J Pediatr Orthop. 2003; 23:535–541. PMID: 12826956.
Article20. Harries N, Kassirer M, Amichai T, Lahat E. Changes over years in gross motor function of 3-8 year old children with cerebral palsy: using the Gross Motor Function Measure (GMFM-88). Isr Med Assoc J. 2004; 6:408–411. PMID: 15274531.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Effectiveness of Selective Posterior Rhizotomy for the Rehabilitation in Children with Cerebral Palsy
- Relation among the Gross Motor Function, Manual Performance and Upper Limb Functional Measures in Children with Spastic Cerebral Palsy
- Gross Motor Function Outcome After Intensive Rehabilitation in Children With Bilateral Spastic Cerebral Palsy
- Comparison between the Effect of Aquatic Exercise Program and Land Exercise Program in Spastic Cerebral Palsy on Motor Function and Balance
- Effects of Hippotherapy on Gross Motor Function and Functional Performance of Children with Cerebral Palsy