Ann Rehabil Med.
2014 Oct;38(5):612-619. 10.5535/arm.2014.38.5.612.
Cutoff Value of Pharyngeal Residue in Prognosis Prediction After Neuromuscular Electrical Stimulation Therapy for Dysphagia in Subacute Stroke Patients
- Affiliations
-
- 1Department of Rehabilitation Medicine, Wonju Severance Christian Hospital, Yonsei University Wonju College of Medicine, Wonju, Korea. enmcse@hanmail.net
- 2Department of Preventive Medicine, Yonsei University Wonju College of Medicine, Wonju, Korea.
- 3Department of Occupational Therapy, Graduate School of Yonsei University, Wonju, Korea.
- KMID: 2266495
- DOI: http://doi.org/10.5535/arm.2014.38.5.612
Abstract
OBJECTIVE
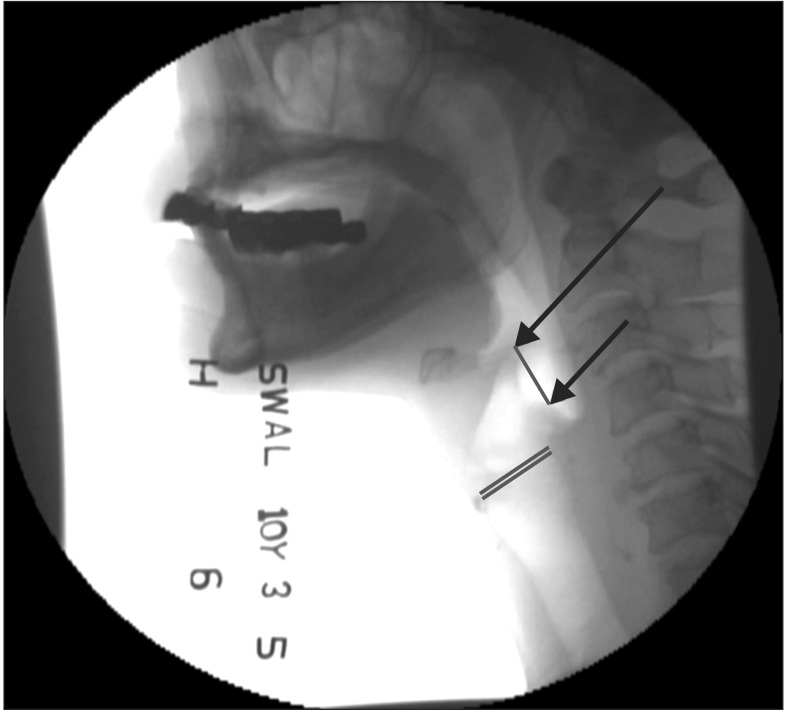
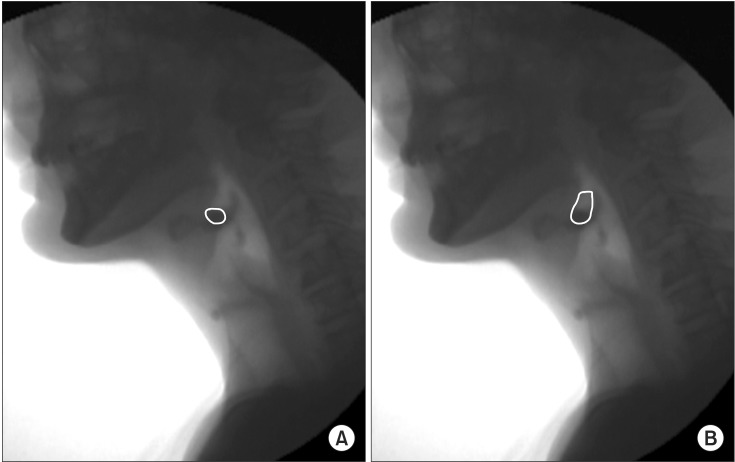
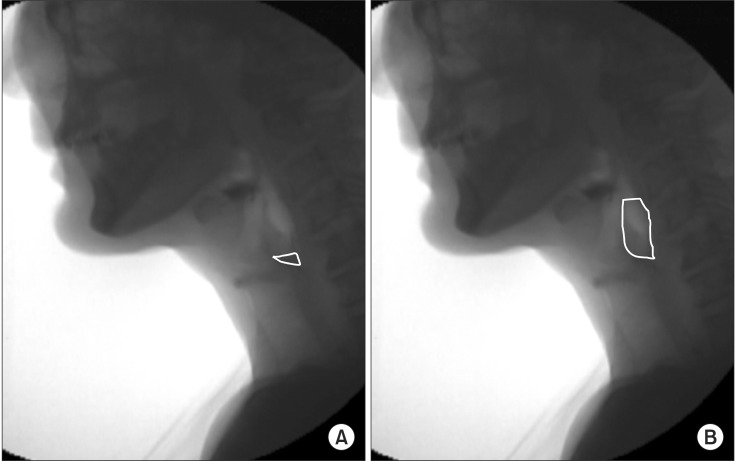
To determine the cutoff value of the pharyngeal residue for predicting reduction of aspiration, by measuring the residue of valleculae and pyriformis sinuses through videofluoroscopic swallowing studies (VFSS) after treatment with neuromuscular electrical stimulator (VitalStim) in stroke patients with dysphagia.
METHODS
VFSS was conducted on first-time stroke patients before and after the VitalStim therapy. The results were analyzed for comparison of the pharyngeal residue in the improved group and the non-improved group.
RESULTS
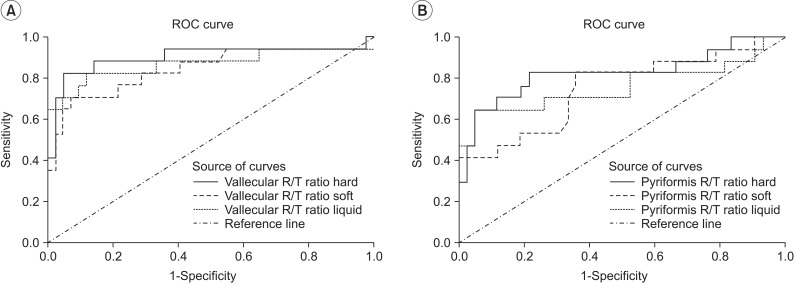
A total of 59 patients concluded the test, in which 42 patients improved well enough to change the dietary methods while 17 did not improve sufficiently. Remnant area to total area (R/T) ratios of the valleculae before treatment in the improved group were 0.120, 0.177, and 0.101 for solid, soft, and liquid foods, respectively, whereas the ratios for the non-improved group were 0.365, 0.396, and 0.281, respectively. The ratios of the pyriformis sinuses were 0.126, 0.159, and 0.121 for the improved group and 0.315, 0.338, and 0.244 for the non-improved group. The R/T ratios of valleculae and pyriformis sinus were significantly lower in the improved group than the non-improved group in all food types before treatment. The R/T ratio cutoff values were 0.267, 0.250, and 0.185 at valleculae and 0.228, 0.218, and 0.185 at pyriformis sinuses.
CONCLUSION
In dysphagia after stroke, less pharyngeal residue before treatment serves as a factor for predicting greater improvement after VitalStim treatment.
Keyword
Figure
Reference
-
1. Allen JE, White CJ, Leonard RJ, Belafsky PC. Prevalence of penetration and aspiration on videofluoroscopy in normal individuals without dysphagia. Otolaryngol Head Neck Surg. 2010; 142:208–213. PMID: 20115976.
Article2. Falsetti P, Acciai C, Palilla R, Bosi M, Carpinteri F, Zingarelli A, et al. Oropharyngeal dysphagia after stroke: incidence, diagnosis, and clinical predictors in patients admitted to a neurorehabilitation unit. J Stroke Cerebrovasc Dis. 2009; 18:329–335. PMID: 19717014.
Article3. Garon BR, Sierzant T, Ormiston C. Silent aspiration: results of 2,000 video fluoroscopic evaluations. J Neurosci Nurs. 2009; 41:178–185. PMID: 19678503.4. Diniz PB, Vanin G, Xavier R, Parente MA. Reduced incidence of aspiration with spoon-thick consistency in stroke patients. Nutr Clin Pract. 2009; 24:414–418. PMID: 19483070.
Article5. Murguia M, Corey DM, Daniels SK. Comparison of sequential swallowing in patients with acute stroke and healthy adults. Arch Phys Med Rehabil. 2009; 90:1860–1865. PMID: 19887209.
Article6. Kim Y, McCullough GH. Maximal hyoid excursion in poststroke patients. Dysphagia. 2010; 25:20–25. PMID: 19655199.
Article7. Han TR, Paik NJ, Park JW. Quantifying swallowing function after stroke: a functional dysphagia scale based on videofluoroscopic studies. Arch Phys Med Rehabil. 2001; 82:677–682. PMID: 11346847.
Article8. Logemann JA, Rademaker A, Pauloski BR, Kelly A, Stangl-McBreen C, Antinoja J, et al. A randomized study comparing the Shaker exercise with traditional therapy: a preliminary study. Dysphagia. 2009; 24:403–411. PMID: 19472007.
Article9. Carnaby-Mann GD, Crary MA. Examining the evidence on neuromuscular electrical stimulation for swallowing: a meta-analysis. Arch Otolaryngol Head Neck Surg. 2007; 133:564–571. PMID: 17576907.10. Blumenfeld L, Hahn Y, Lepage A, Leonard R, Belafsky PC. Transcutaneous electrical stimulation versus traditional dysphagia therapy: a nonconcurrent cohort study. Otolaryngol Head Neck Surg. 2006; 135:754–757. PMID: 17071307.
Article11. Shaw GY, Sechtem PR, Searl J, Keller K, Rawi TA, Dowdy E. Transcutaneous neuromuscular electrical stimulation (VitalStim) curative therapy for severe dysphagia: myth or reality? Ann Otol Rhinol Laryngol. 2007; 116:36–44. PMID: 17305276.
Article12. Kelly AM, Macfarlane K, Ghufoor K, Drinnan MJ, Lew-Gor S. Pharyngeal residue across the lifespan: a first look at what's normal. Clin Otolaryngol. 2008; 33:348–351. PMID: 18983345.
Article13. Han TR, Shin HI, Park JW, Park IC. The effects of viscosity on oropharyngeal phase. J Korean Acad Rehabil Med. 2001; 25:236–240.14. Paolucci S, Antonucci G, Grasso MG, Bragoni M, Coiro P, De Angelis D, et al. Functional outcome of ischemic and hemorrhagic stroke patients after inpatient rehabilitation: a matched comparison. Stroke. 2003; 34:2861–2865. PMID: 14615613.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Neuromuscular Electrical Stimulation Therapy for Patients with Chronic Dysphagia Caused by Stroke
- The Effect of Functional Electrical Stimulation on Swallowing Function in Stroke Patients with Dysphagia
- Effects of Neuromuscular Electrical Stimulation in Combination with Saliva or Dry Swallowing in Stroke Patients with Dysphagia
- The Effect of Early Neuromuscular Electrical Stimulation Therapy in Acute/Subacute Ischemic Stroke Patients With Dysphagia
- Neuromuscular Electrical Stimulation for Dysphagia