Ann Dermatol.
2012 Nov;24(4):444-452. 10.5021/ad.2012.24.4.444.
Skin Characteristics in Patients with Pityriasis Versicolor Using Non-Invasive Method, MPA5
- Affiliations
-
- 1Department of Dermatology, Konkuk University School of Medicine, Seoul, Korea. kjahn@kuh.ac.kr
- 2Konkuk University Research Institute of Medical Science, Seoul, Korea.
- KMID: 2266040
- DOI: http://doi.org/10.5021/ad.2012.24.4.444
Abstract
- BACKGROUND
Skin pigmentary changes of pityriasis versicolor may occur as either hyperpigmented or hypopigmented lesions, depending on the outcome of interactions between Malassezia yeasts and the skin, such as lipoperoxidation process, stimulus of inflammatory cell to melanocytes, and increased thickness of keratin layer.
OBJECTIVE
To investigate skin characteristic factors that enhance the susceptibility to Malassezia yeasts and provoke different color changes of pityriasis versicolor patients.
METHODS
To clarify these factors, we investigated the skin characteristics of pityriasis versicolor patients, using a non-invasive method known as MPA 5(R) (Courage and Khazaka, Germany). A total of 90 normal healthy subjects and 30 pityriasis versicolor patients were included in this study.
RESULTS
Both hyperpigmented and hypopigmented pityriasis versicolor skin lesions showed higher humidity, increased sebum excretion rate and increased transepidermal water loss (TEWL) values than normal healthy subjects. But no significant difference of specific Malassezia yeasts species between hyperpigmented and hypopigmented skin lesions was evident.
CONCLUSION
These results indicate that higher humidity and increased sebum level provide a better growing environment of Malassezia yeasts in the skin, leading to the assumption that interaction between Malassezia yeasts and skin barrier materials makes disruption of skin barrier causing increased TEWL.
MeSH Terms
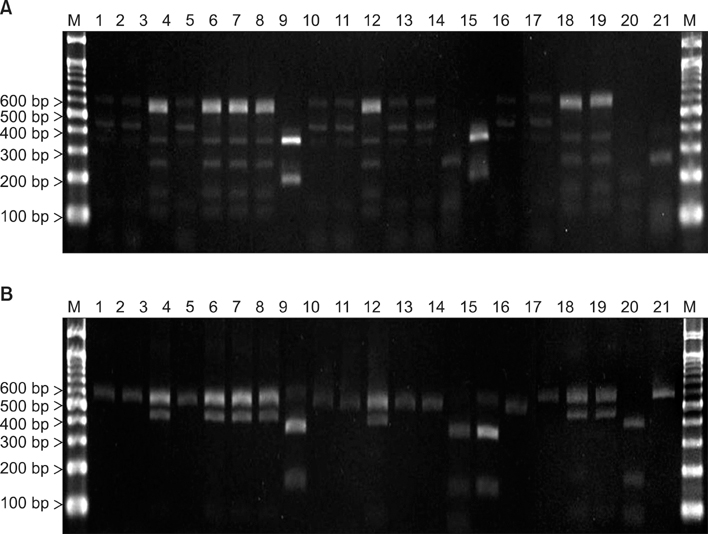
Figure
Cited by 1 articles
-
Progress in Malassezia Research in Korea
Soo Young Kim, Yang Won Lee, Yong Beom Choe, Kyu Joong Ahn
Ann Dermatol. 2015;27(6):647-657. doi: 10.5021/ad.2015.27.6.647.
Reference
-
1. Adamski Z. Studies of a role played by lipophilic yeasts Malassezia furfur (Pityrosporum ovale, Pityrosporum orbiculare) in different dermatoses. Postepy Dermatol (Poznan). 1995. 12:349–454.2. Sunenshine PJ, Schwartz RA, Janniger CK. Tinea versicolor. Int J Dermatol. 1998. 37:648–655.
Article3. Morishita N, Sei Y, Sugita T. Molecular analysis of malassezia microflora from patients with pityriasis versicolor. Mycopathologia. 2006. 161:61–65.
Article4. Ahn KJ. Malassezia species cultured from the lesions of pityriasis versicolor. Korean J Dermatol. 1997. 35:736–743.5. Ahn KJ. Taxonomy of the genus Malassezia. Korean J Med Mycol. 1998. 3:81–88.6. Yoo DW, Kim HJ, Kim YW, Ro BI, Chang CY. Electron microscopic study in tinea versicolor: structural changes of melanosomes accompanying the hyperpigmented and hypopigmented lesions. Korean J Dermatol. 1983. 21:63–70.7. Allen HB, Charles CR, Johnson BL. Hyperpigmented tinea versicolor. Arch Dermatol. 1976. 112:1110–1112.
Article8. Charles CR, Sire DJ, Johnson BL, Beidler JG. Hypopigmentation in tinea versicolor: a histochemical and electronmicroscopic study. Int J Dermatol. 1973. 12:48–58.
Article9. Koh JS, Chae KS, Kim HO. Skin characteristics of normal Korean subjects according to sex and site using non-invasive bioengineering methods. Korean J Dermatol. 1998. 36:855–864.10. Serup J, Jemec GBE. Handbook of non-invasive methods and the skin. 1995. Boca Raton: CRC Press;3–8.11. Moss J. The effect of 3 moistures on skin surface hydration. Skin Res Technol. 1996. 2:32–36.12. Thoma S, Welzel J, Wilhelm KP. Relationship between transepidermal water loss and temperature of measuring probe. Skin Res Technol. 1997. 3:73–80.
Article13. Cunliffe WJ, Kearney JN, Simpson NB. A modified photometric technique for measuring sebum excretion rate. J Invest Dermatol. 1980. 75:394–398.
Article14. Jang HY, Park CW, Lee CH. A study of transepidermal water loss at various anatomical sites of the skin. Korean J Dermatol. 1996. 34:402–406.15. Guého E, Midgley G, Guillot J. The genus Malassezia with description of four new species. Antonie Van Leeuwenhoek. 1996. 69:337–355.
Article16. Sugita T, Kodama M, Saito M, Ito T, Kato Y, Tsuboi R, et al. Sequence diversity of the intergenic spacer region of the rRNA gene of Malassezia globosa colonizing the skin of patients with atopic dermatitis and healthy individuals. J Clin Microbiol. 2003. 41:3022–3027.
Article17. Sugita T, Takashima M, Shinoda T, Suto H, Unno T, Tsuboi R, et al. New yeast species, Malassezia dermatis, isolated from patients with atopic dermatitis. J Clin Microbiol. 2002. 40:1363–1367.
Article18. Sugita T, Takashima M, Kodama M, Tsuboi R, Nishikawa A. Description of a new yeast species, Malassezia japonica, and its detection in patients with atopic dermatitis and healthy subjects. J Clin Microbiol. 2003. 41:4695–4699.
Article19. Hirai A, Kano R, Makimura K, Duarte ER, Hamdan JS, Lachance MA, et al. Malassezia nana sp. nov., a novel lipid-dependent yeast species isolated from animals. Int J Syst Evol Microbiol. 2004. 54:623–627.
Article20. Sugita T, Tajima M, Takashima M, Amaya M, Saito M, Tsuboi R, et al. A new yeast, Malassezia yamatoensis, isolated from a patient with seborrheic dermatitis, and its distribution in patients and healthy subjects. Microbiol Immunol. 2004. 48:579–583.
Article21. Lee YW, Yim SM, Lim SH, Choe YB, Ahn KJ. Quantitative investigation on the distribution of Malassezia species on healthy human skin in Korea. Mycoses. 2006. 49:405–410.
Article22. Cabañes FJ, Theelen B, Castellá G, Boekhout T. Two new lipid-dependent Malassezia species from domestic animals. FEMS Yeast Res. 2007. 7:1064–1076.23. Gandra RF, Simão RC, Matsumoto FE, da Silva BC, Ruiz LS, da Silva EG, et al. Genotyping by RAPD-PCR analyses of Malassezia furfur strains from pityriasis versicolor and seborrhoeic dermatitis patients. Mycopathologia. 2006. 162:273–280.
Article24. Gaitanis G, Velegraki A, Alexopoulos EC, Chasapi V, Tsigonia A, Katsambas A. Distribution of Malassezia species in pityriasis versicolor and seborrhoeic dermatitis in Greece. Typing of the major pityriasis versicolor isolate M. globosa. Br J Dermatol. 2006. 154:854–859.
Article25. King RD, Cunico RL, Maibach HI, Greenberg JH, West ML, Jeppsen JC. The effect of occlusion on carbon dioxide emission from human skin. Acta Derm Venereol. 1978. 58:135–138.26. Faergemann J, Bernander S. Tinea versicolor and Pityrosporum orbiculare: a mycological investigation. Sabouraudia. 1979. 17:171–179.27. Congly H. Pityriasis versicolor in a 3-month-old boy. Can Med Assoc J. 1984. 130:844–845.28. Roberts SO. Pityriasis versicolor: a clinical and mycological investigation. Br J Dermatol. 1969. 81:315–326.
Article29. Burke RC. Tinea versicolor: susceptibility factors and experimental infection in human beings. J Invest Dermatol. 1961. 36:389–402.
Article30. Hayakawa R. Measurement methods and evaluation of skin surface lipids. Fragrance J. 1988. 92:26–30.31. Conti A, Schiavi ME, Seidenari S. Capacitance, transepidermal water loss and causal level of sebum in healthy subjects in relation to site, sex and age. Int J Cosmet Sci. 1995. 17:77–85.
Article32. Ozawa T, Takahashi M. Skin hydration: recent advances. Acta Derm Venereol Suppl (Stockh). 1994. 185:26–28.33. Nakabayashi A, Sei Y, Guillot J. Identification of Malassezia species isolated from patients with seborrhoeic dermatitis, atopic dermatitis, pityriasis versicolor and normal subjects. Med Mycol. 2000. 38:337–341.
Article34. Krisanty RI, Bramono K, Made Wisnu I. Identification of Malassezia species from pityriasis versicolor in Indonesia and its relationship with clinical characteristics. Mycoses. 2009. 52:257–262.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Efficacy and Tolerability of Terbinafine 1% Cream in Patients with Pityriasis Versicolor
- Atrophying Pityriasis Versicolor: Is This a New Variant of Pityriasis Versicolor?
- Malassezia Species Cultured from the Lesions of Pityriasis Versicolor
- Pityriasis Versicolor Atrophicans
- Two Cases of Pityriasis Versicolor on the Scalp in the Course of Treatment for Alopecia Totalis