Ann Dermatol.
2014 Feb;26(1):61-65. 10.5021/ad.2014.26.1.61.
Clinical Course of Segmental Vitiligo: A Retrospective Study of Eighty-Seven Patients
- Affiliations
-
- 1Department of Dermatology, Kangbuk Samsung Hospital, Seoul, Korea.
- 2Department of Dermatology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. dylee@skku.edu
- 3Division of Dermatology, Loyola University Strich School of Medicine, LaGrange Park, IL, USA.
- KMID: 2265698
- DOI: http://doi.org/10.5021/ad.2014.26.1.61
Abstract
- BACKGROUND
Vitiligo is an acquired disorder characterized by a progressive loss of melanocytes, which is difficult to manage and has an unknown prognosis. The subtype of segmental vitiligo (SV) has been established but it has not been adequately characterized.
OBJECTIVE
To collect long-term follow-up data for evaluating the clinical course of SV.
METHODS
This study included 87 patients who were diagnosed with SV and were monitored at a clinic. Patients were classified into the following three groups according to disease activity.
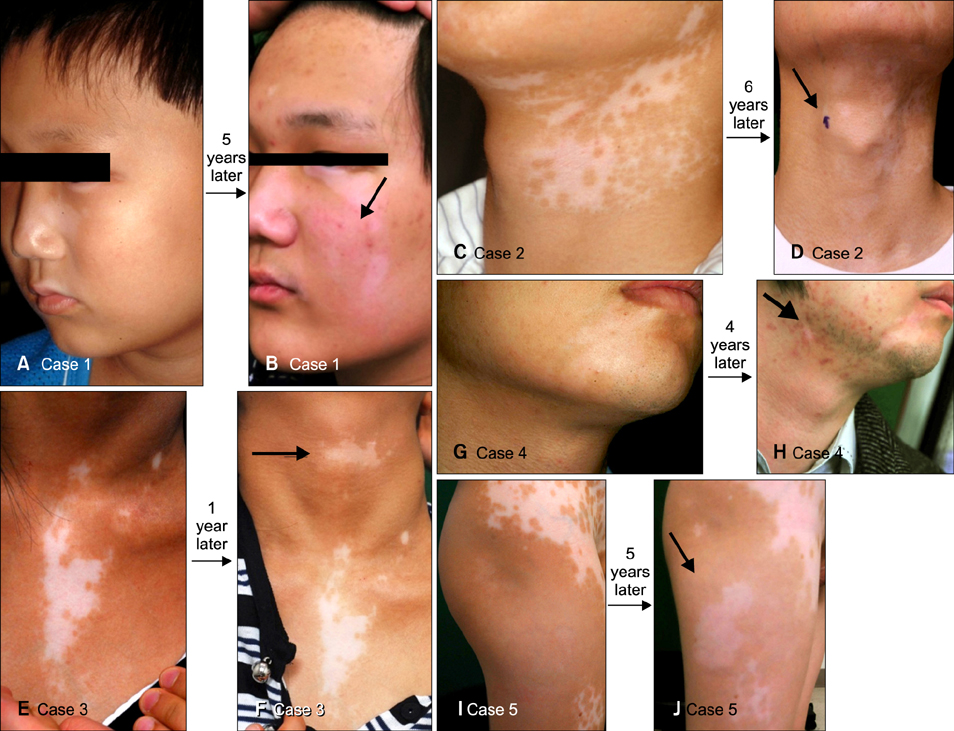
RESULTS
Among the patients with SV, 63.2% had stable disease, 14.9% had disease recurrence between two and four years after disease onset, and 21.8% had disease recurrence at four or more than four years after disease onset. Among the 44 patients (50.2%) who were monitored continuously over a four-year period, 19 (43.2%) experienced a recurrence at four or more than four years after disease onset.
CONCLUSION
Our results suggest that, contrary to previous reports, some patients with SV may not experience disease stability over an extended period of time. Disease recurrence can occur after years of stability, and we propose that long-term follow-up data can be used to characterize SV. This information about the clinical course of SV has implications for treatment and prognosis.
Keyword
Figure
Reference
-
1. Taïeb A. Intrinsic and extrinsic pathomechanisms in vitiligo. Pigment Cell Res. 2000; 13:Suppl 8. 41–47.
Article2. Koga M, Tango T. Clinical features and course of type A and type B vitiligo. Br J Dermatol. 1988; 118:223–228.
Article3. Taïeb A, Picardo M. Clinical practice. Vitiligo. N Engl J Med. 2009; 360:160–169.4. Hann SK, Lee HJ. Segmental vitiligo: clinical findings in 208 patients. J Am Acad Dermatol. 1996; 35:671–674.
Article5. Lee DY, Kim CR, Lee JH. Targeted phototherapy in combination with drug therapy for segmental vitiligo. Photodermatol Photoimmunol Photomed. 2011; 27:108–110.
Article6. Lee DY, Kim CR, Park JH, Lee JH. The incidence of leukotrichia in segmental vitiligo: implication of poor response to medical treatment. Int J Dermatol. 2011; 50:925–927.
Article7. Taïeb A, Morice-Picard F, Jouary T, Ezzedine K, Cario-André M, Gauthier Y. Segmental vitiligo as the possible expression of cutaneous somatic mosaicism: implications for common non-segmental vitiligo. Pigment Cell Melanoma Res. 2008; 21:646–652.
Article8. Ezzedine K, Diallo A, Léauté-Labrèze C, Mossalayi D, Gauthier Y, Bouchtnei S, et al. Multivariate analysis of factors associated with early-onset segmental and nonsegmental vitiligo: a prospective observational study of 213 patients. Br J Dermatol. 2011; 165:44–49.
Article9. Mazereeuw-Hautier J, Bezio S, Mahe E, Bodemer C, Eschard C, Viseux V, et al. Groupe de Recherche Clinique en Dermatologie Pédiatrique (GRCDP). Segmental and nonsegmental childhood vitiligo has distinct clinical characteristics: a prospective observational study. J Am Acad Dermatol. 2010; 62:945–949.
Article10. Mulekar SV. Long-term follow-up study of segmental and focal vitiligo treated by autologous, noncultured melanocyte-keratinocyte cell transplantation. Arch Dermatol. 2004; 140:1211–1215.
Article11. Al-Mutairi N, Manchanda Y, Al-Doukhi A, Al-Haddad A. Long-term results of split-skin grafting in combination with excimer laser for stable vitiligo. Dermatol Surg. 2010; 36:499–505.
Article12. van Geel N, Wallaeys E, Goh BK, De Mil M, Lambert J. Long-term results of noncultured epidermal cellular grafting in vitiligo, halo naevi, piebaldism and naevus depigmentosus. Br J Dermatol. 2010; 163:1186–1193.
Article