Ann Dermatol.
2014 Aug;26(4):505-509. 10.5021/ad.2014.26.4.505.
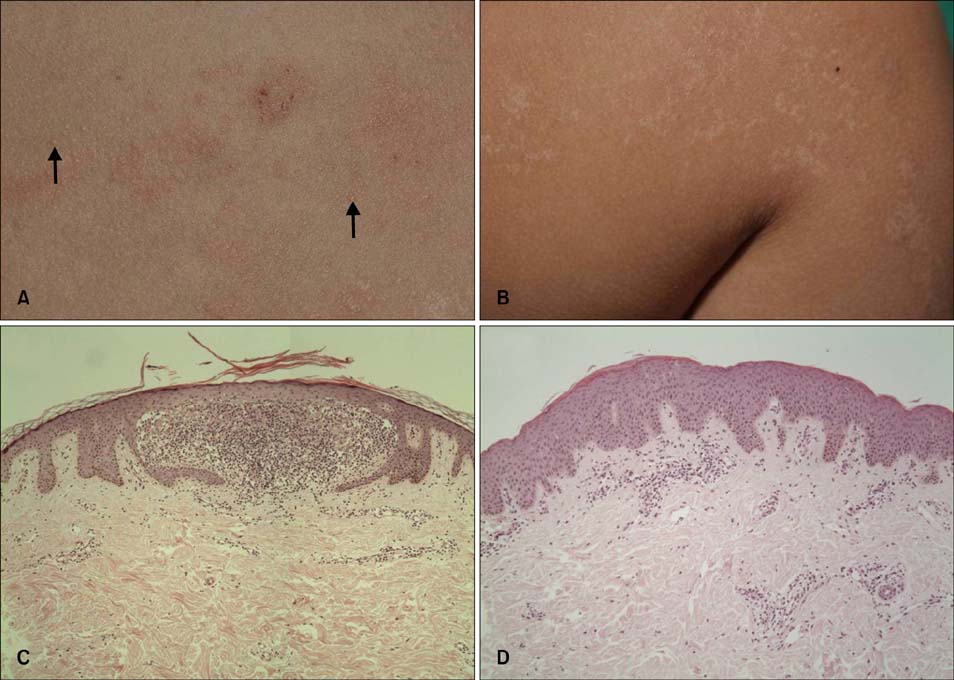
Three Cases of Lichen Nitidus Associated with Various Cutaneous Diseases
- Affiliations
-
- 1Department of Dermatology, Hallym University Sacred Heart Hospital, Anyang, Korea. dermakkh@naver.com
- KMID: 2265594
- DOI: http://doi.org/10.5021/ad.2014.26.4.505
Abstract
- Lichen nitidus (LN) is an uncommon, usually asymptomatic cutaneous eruption characterized by the presence of multiple, small, flesh-colored papules. The epidemiologic and pathophysiologic characteristics of LN have not yet been defined. Furthermore, LN has rarely been described in association with other cutaneous diseases. We herein report 3 cases of LN associated with various cutaneous diseases, including lichen striatus, oral lichen planus, and psoriasis vulgaris.
Keyword
Figure
Reference
-
1. Pinkus F. Verhand. Berlin Dermat Gesel. 1901; 12:3.2. Park JH, Kye YC, Kim SN. A clinical and histopathologic study of lichen nitidus. Korean J Dermatol. 2003; 41:857–868.3. Munro CS, Cox NH, Marks JM, Natarajan S. Lichen nitidus presenting as palmoplantar hyperkeratosis and nail dystrophy. Clin Exp Dermatol. 1993; 18:381–383.
Article4. Thibaudeau A, Maillard H, Croué A, Belperron P, Avenel Audran M, Verret JL. Palmoplantar lichen nitidus: a rare cause of palmoplantar hyperkeratosis. Ann Dermatol Venereol. 2004; 131:822–824.5. Natarajan S, Dick DC. Lichen nitidus associated with nail changes. Int J Dermatol. 1986; 25:461–462.
Article6. Krook G. Purpura in lichen nitidus generalisatus. Report of a case. Acta Derm Venereol. 1959; 39:238–246.7. Tilly JJ, Drolet BA, Esterly NB. Lichenoid eruptions in children. J Am Acad Dermatol. 2004; 51:606–624.
Article8. Mobini N, Toussaint S, Kamino H. Noninfectious erythematous, papular, and squamous diseases. In : Elder DE, Elenitsas R, Johnson BL, Murphy GF, Xu X, editors. Lever's histopathology of the skin. 10th ed. Philadelphia: Lippincott-Raven;2009. p. 192–193.9. Aram H. Association of lichen planus and lichen nitidus. Treatment with etretinate. Int J Dermatol. 1988; 27:117.10. Kano Y, Shiohara T, Yagita A, Nagashima M. Erythema nodosum, lichen planus and lichen nitidus in Crohn's disease: report of a case and analysis of T cell receptor V gene expression in the cutaneous and intestinal lesions. Dermatology. 1995; 190:59–63.
Article11. Kawakami T, Soma Y. Generalized lichen nitidus appearing subsequent to lichen planus. J Dermatol. 1995; 22:434–437.
Article12. Di Lernia V, Piana S, Ricci C. Lichen planus appearing subsequent to generalized lichen nitidus in a child. Pediatr Dermatol. 2007; 24:453–455.
Article13. Agarwal S, Guglani V, Kumar B. Down's syndrome with lichen nitidus and segmental vitiligo. Indian J Dermatol Venereol Leprol. 2009; 75:627–629.
Article14. MacDonald AJ, Drummond A, Chui D, Holmes S. Lichen nitidus and lichen spinulosus or spinous follicular lichen nitidus? Clin Exp Dermatol. 2005; 30:452–453.
Article15. Smoller BR, Flynn TC. Immunohistochemical examination of lichen nitidus suggests that it is not a localized papular variant of lichen planus. J Am Acad Dermatol. 1992; 27:232–236.
Article16. Scheler M, Proelss J, Bräuninger W, Bieber T, Wenzel J. Generalized lichen nitidus with involvement of the palms following interferon alpha treatment. Dermatology. 2007; 215:236–239.
Article17. Berger TG, Dhar A. Lichenoid photoeruptions in human immunodeficiency virus infection. Arch Dermatol. 1994; 130:609–613.
Article18. Sanders S, Collier DA, Scott R, Wu H, MeNutt NS. Periappendageal lichen nitidus: report of a case. J Cutan Pathol. 2002; 29:125–128.
Article19. Madhok R, Winkelmann RK. Spinous, follicular lichen nitidus associated with perifollicular granulomas. J Cutan Pathol. 1988; 15:245–248.
Article20. Petrozzi JW, Shmunes E. Linear lichen nitidus. Cutis. 1970; 6:1109–1112.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Lichen Nitidus Coexisted with Molluscum Contagiosum
- Perforating Lichen Nitidus Associated with Oral Lichen Planus
- Two Cases of Lichen Striatus Mimicking Lichen Nitidus
- Two Cases of Lichen Nitidus Treated with Topical 0.1% Tacrolimus
- A Case of Lichen Nitidus with the Koebner Phenomenon Mimicking Lichen Striatus