Ann Dermatol.
2014 Aug;26(4):478-484. 10.5021/ad.2014.26.4.478.
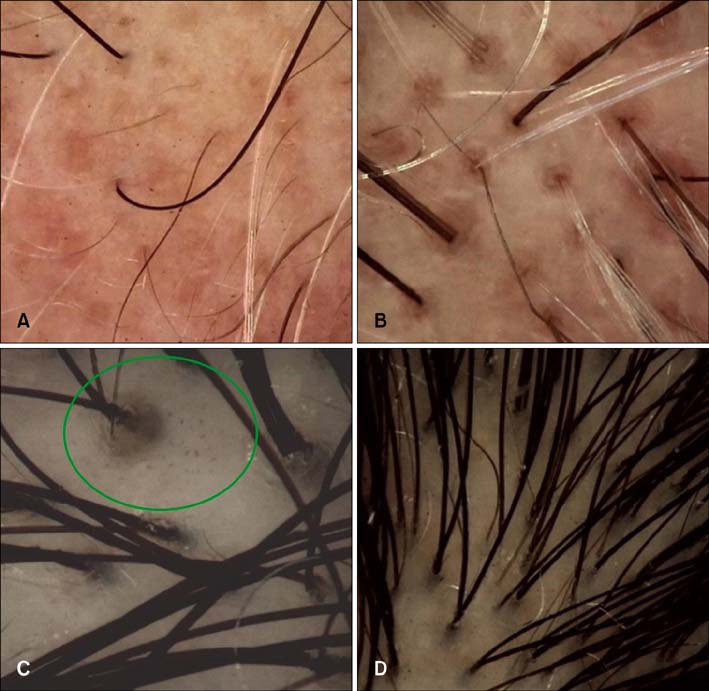
Scalp Dermatoscopic Findings in Androgenetic Alopecia and Their Relations with Disease Severity
- Affiliations
-
- 1Department of Dermatology, Beypazari Public Hospital, Ankara, Turkey. kibarmelike@hotmail.com
- 2Department of Dermatology, Dokuz Eylul University School of Medicine, Izmir, Turkey.
- 3Department of Biostatistics, Eskisehir Osmangazi University School of Medicine, Eskisehir, Turkey.
- KMID: 2265589
- DOI: http://doi.org/10.5021/ad.2014.26.4.478
Abstract
- BACKGROUND
Clinicians are searching for new methods to diagnose and predict the course of androgenetic alopecia noninvasively.
OBJECTIVE
Our aim is to evaluate trichoscopic findings and their relations with disease severity in androgenetic alopecia.
METHODS
The videodermatoscopic findings of 143 female and 63 male patients with androgenetic alopecia were compared with each other, with those of healthy subjects (n=100), and with those of patients with other nonscarring alopecias (n=208). Mann-Whitney U-test, chi2 analyses, and logistic regression analysis were used for statistical analysis.
RESULTS
No statistically significant relation was found between trichoscopic findings and severity in male androgenetic alopecia (MAGA) on the basis of the modified Hamilton Norwood scale (among 7 degrees); however, multihair follicular unit and perifollicular pigmentation were related to low severity whereas white dots, honeycomb pattern pigmentation, and brown dots were related to high severity. On the other hand, according to the Ludwig classification, arborizing red lines were related to low severity and brown dots were related to high severity, whereas there was no difference in stages between the Ebling and Olsen classifications in female androgenetic alopecia (FAGA). In the characteristic trichoscopic findings in this study, perifollicular pigmentation was found as a normal feature of the scalp, whereas multihair follicular unit and honeycomb pigment pattern, which were previously considered as normal features, were observed to be related to androgenetic alopecia.
CONCLUSION
No relation was found between MAGA severity and trichoscopic findings, as well as between FAGA severity according to different disease severity classifications and trichoscopic findings.
Keyword
Figure
Reference
-
1. Gordon KA, Tosti A. Alopecia: evaluation and treatment. Clin Cosmet Investig Dermatol. 2011; 4:101–106.
Article2. Inui S, Nakajima T, Itami S. Scalp dermoscopy of androgenetic alopecia in Asian people. J Dermatol. 2009; 36:82–85.
Article3. Ross EK, Vincenzi C, Tosti A. Videodermoscopy in the evaluation of hair and scalp disorders. J Am Acad Dermatol. 2006; 55:799–806.
Article4. Rakowska A, Slowinska M, Kowalska-Oledzka E, Olszewska M, Rudnicka L. Dermoscopy in female androgenic alopecia: method standardization and diagnostic criteria. Int J Trichology. 2009; 1:123–130.
Article5. Lacarrubba F, Dall'Oglio F, Rita Nasca M, Micali G. Videodermatoscopy enhances diagnostic capability in some forms of hair loss. Am J Clin Dermatol. 2004; 5:205–208.
Article6. Olsen EA. Female pattern hair loss. J Am Acad Dermatol. 2001; 45:3 Suppl. S70–S80.
Article7. Harrison S, Sinclair R. Telogen effluvium. Clin Exp Dermatol. 2002; 27:389–385.
Article8. Camacho-Martínez FM. Hair loss in women. Semin Cutan Med Surg. 2009; 28:19–32.
Article9. Ludwig E. Classification of the types of androgenetic alopecia (common baldness) occurring in the female sex. Br J Dermatol. 1977; 97:247–254.
Article10. Abraham LS, Piñeiro-Maceira J, Duque-Estrada B, Barcaui CB, Sodré CT. Pinpoint white dots in the scalp: dermoscopic and histopathologic correlation. J Am Acad Dermatol. 2010; 63:721–722.
Article11. Wolff H. Diseases of hair. In : Braun-Falco O, Plewig G, Wolff HH, Landthaler M, editors. Braun-Falco's Dermatology. 3th ed. Heidelberg: Springer Verlag;2009. p. 1029–1059.12. Paus R, Peker S, Sundberg JP. Biology of hair and nails. In : Bolognia JL, Jorizzo JL, Rapini RP, editors. Dermatology. 2th ed. St. Louis: Mosby Elsevier;2008. p. 965–987.13. Whiting DA. Diagnostic and predictive value of horizontal sections of scalp biopsy specimens in male pattern androgenetic alopecia. J Am Acad Dermatol. 1993; 28:755–763.
Article14. Whiting D. Scalp biopsy as a diagnostic and prognostic tool in androgenic alopecia. Dermatol Ther. 1998; 8:24–33.15. Won CH, Kwon OS, Kim YK, Kang YJ, Kim BJ, Choi CW, et al. Dermal fibrosis in male pattern hair loss: a suggestive implication of mast cells. Arch Dermatol Res. 2008; 300:147–152.
Article16. Bertolino PA, Freedberg IM. Disorders of epidermal appendages and related disorders. In : Freedberg IM, Eisen AZ, Wollf K, editors. Dermatology in general medicine. 4th ed. New York: McGraw-Hill;1993.17. Sperling LC, Winton GB. The transverse anatomy of androgenic alopecia. J Dermatol Surg Oncol. 1990; 16:1127–1133.
Article18. Leroy T, Van Neste D. Contrast enhanced phototrichogram pinpoints scalp hair changes in androgen sensitive areas of male androgenetic alopecia. Skin Res Technol. 2002; 8:106–111.
Article19. Kossard S, Zagarella S. Spotted cicatricial alopecia in dark skin. A dermoscopic clue to fibrous tracts. Australas J Dermatol. 1993; 34:49–51.20. Zhang X, Caulloo S, Zhao Y, Zhang B, Cai Z, Yang J. Female pattern hair loss: clinico-laboratory findings and trichoscopy depending on disease severity. Int J Trichology. 2012; 4:23–28.
Article21. Ardigò M, Tosti A, Cameli N, Vincenzi C, Misciali C, Berardesca E. Reflectance confocal microscopy of the yellow dot pattern in alopecia areata. Arch Dermatol. 2011; 147:61–64.
Article22. Tosti A. Alopecia areata. In : Tosti A, editor. Dermoscopy of hair and scalp disorders with clinical and pathological correlations. London: Informa Healthcare;2007. p. 26–50.23. Cotsarelis G, Botchkarev V. Biology of hair follicles. In : Wollf K, Goldsmith LA, Katz SI, Gilchrest BA, Paller AS, Leffell DJ, editors. Fitzpatrick's dermatology in general medicine. 7th ed. New York: McGraw-Hill;2008. p. 39–749.24. Deloche C, de Lacharrière O, Misciali C, Piraccini BM, Vincenzi C, Bastien P, et al. Histological features of peripilar signs associated with androgenetic alopecia. Arch Dermatol Res. 2004; 295:422–428.
Article25. Miteva M, Tosti A. Hair and scalp dermatoscopy. J Am Acad Dermatol. 2012; 67:1040–1048.
Article26. Rakowska A. Trichoscopy (hair and scalp videodermoscopy) in the healthy female. Method standardization and norms for measurable parameters. J Dermatol Case Rep. 2009; 3:14–19.
Article27. Young JW, Conte ET, Leavitt ML, Nafz MA, Schroeter AL. Cutaneous immunopathology of androgenetic alopecia. J Am Osteopath Assoc. 1991; 91:765–771.
Article28. Headington JT. Transverse microscopic anatomy of the human scalp. A basis for a morphometric approach to disorders of the hair follicle. Arch Dermatol. 1984; 120:449–456.
Article29. Jaworsky C, Kligman AM, Murphy GF. Characterization of inflammatory infiltrates in male pattern alopecia: implications for pathogenesis. Br J Dermatol. 1992; 127:239–246.
Article30. Inui S, Nakajima T, Nakagawa K, Itami S. Clinical significance of dermoscopy in alopecia areata: analysis of 300 cases. Int J Dermatol. 2008; 47:688–693.
Article31. Rudnicka L, Rakowska A, Olszewska M. Trichoscopy: how it may help the clinician. Dermatol Clin. 2013; 31:29–41.32. Rudnicka L, Olszewska M, Rakowska A. Atlas of trichoscopy: dermoscopy in hair and scalp disease. London: New York;Springer-Verlag. p. 2012.33. Fu JM, Starace M, Tosti A. A new dermoscopic finding in healthy children. Arch Dermatol. 2009; 145:596–597.
Article34. Inui S. Trichoscopy for common hair loss diseases: algorithmic method for diagnosis. J Dermatol. 2011; 38:71–75.
Article35. Tosti A, Iorizzo M, Piraccini BM. Androgenetic alopecia in children: report of 20 cases. Br J Dermatol. 2005; 152:556–559.
Article36. Lee WS, Ro BI, Hong SP, Bak H, Sim WY, Kim do W, et al. A new classification of pattern hair loss that is universal for men and women: basic and specific (BASP) classification. J Am Acad Dermatol. 2007; 57:37–46.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Representative Trichoscopic Findings of Outpatients with Androgenetic Alopecia and Alopecia Areata
- A Clinical Study of Androgenetic Alopecia (III)
- Immunohistochemical Comparison of androgen Receptor Expression from Lesional and Non - lesional scalp of Androgenetic alopecia
- A Clinical Study of Androgenetic Alopecia(IV)
- A Case of Androgenetic Alopecia Associated with Cushing's Disease