Ann Dermatol.
2014 Dec;26(6):706-712. 10.5021/ad.2014.26.6.706.
The Effect of Evening Primrose Oil for the Prevention of Xerotic Cheilitis in Acne Patients Being Treated with Isotretinoin: A Pilot Study
- Affiliations
-
- 1Department of Dermatology, Chung-Ang University College of Medicine, Seoul, Korea. drseo@hanafos.com
- KMID: 2264865
- DOI: http://doi.org/10.5021/ad.2014.26.6.706
Abstract
- BACKGROUND
The most common adverse effects of oral isotretinoin are cheilitis, skin dryness, dry eyes, and conjunctivitis, whereas evening primrose oil (EPO) is known to improve skin moisture and transepidermal water loss (TEWL) in healthy adults and atopic patients.
OBJECTIVE
To evaluate the clinical efficacy and safety of EPO in preventing xerotic cheilitis in acne patients being treated with oral isotretinoin.
METHODS
Forty Korean volunteers of Fitzpatrick skin types III and IV, having moderate acne, were enrolled and randomized to receive either isotretinoin with or without EPO for 8 weeks. The efficacy of treatment was evaluated on the basis of global acne grading system scores, number of inflammatory and noninflammatory lesions, TEWL, corneometry, physician's global assessment, and patient satisfaction.
RESULTS
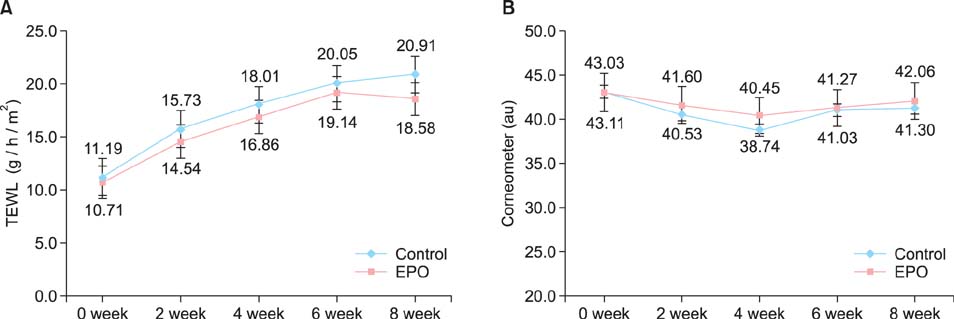
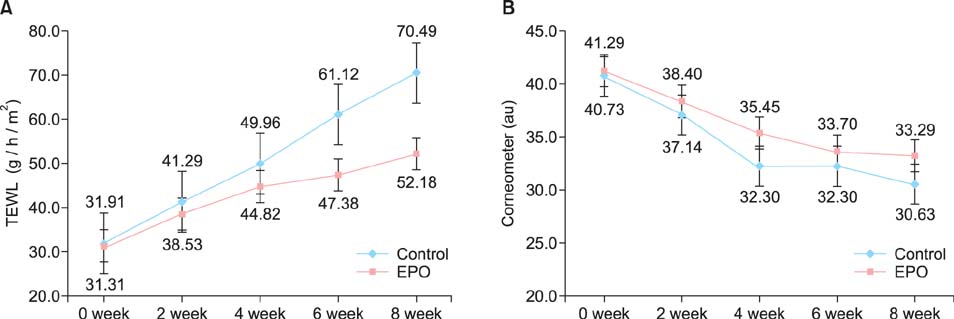
The results after 8 weeks of treatment showed that the TEWL of the lip increased significantly during isotretinoin treatment, whereas the TEWL of the hand dorsum showed no significant change. The increase of the TEWL of the lip was more definite in the control group than in the experimental group. The number of acne lesions decreased significantly in both groups, and there were no differences between them.
CONCLUSION
Our study suggests that the addition of EPO improved xerotic cheilitis in acne patients being treated with oral isotretinoin. However, besides TEWL and corneometry assessments, additional studies are required for a complete understanding of the role of EPO in xerotic cheilitis in acne patients being treated with oral isotretinoin.
MeSH Terms
Figure
Reference
-
1. Layton A. The use of isotretinoin in acne. Dermatoendocrinol. 2009; 1:162–169.
Article2. Haider A, Shaw JC. Treatment of acne vulgaris. JAMA. 2004; 292:726–735.
Article3. Brito Mde F, SantAnna IP, Galindo JC, Rosendo LH, Santos JB. Evaluation of clinical adverse effects and laboratory alterations in patients with acne vulgaris treated with oral isotretinoin. An Bras Dermatol. 2010; 85:331–337.4. Herane MI, Fuenzalida H, Zegpi E, De Pablo C, Espadas MJ, Trullás C, et al. Specific gel-cream as adjuvant to oral isotretinoin improved hydration and prevented TEWL increase--a double-blind, randomized, placebo-controlled study. J Cosmet Dermatol. 2009; 8:181–185.
Article5. McLane J. Analysis of common side effects of isotretinoin. J Am Acad Dermatol. 2001; 45:S188–S194.
Article6. Nykiforuk CL, Shewmaker C, Harry I, Yurchenko OP, Zhang M, Reed C, et al. High level accumulation of gamma linolenic acid (C18:3△6.9,12 cis) in transgenic safflower (Carthamus tinctorius) seeds. Transgenic Res. 2012; 21:367–381.
Article7. Muggli R. Systemic evening primrose oil improves the biophysical skin parameters of healthy adults. Int J Cosmet Sci. 2005; 27:243–249.
Article8. Senapati S, Banerjee S, Gangopadhyay DN. Evening primrose oil is effective in atopic dermatitis: a randomized placebo-controlled trial. Indian J Dermatol Venereol Leprol. 2008; 74:447–452.
Article9. Vahlquist A, Saurat JH. Retinoid. In : Goldsmith LA, Katz SI, Gilchrest BA, Paller AS, Leffell DJ, Wolff K, editors. Fitzpatrick's dermatology in general medicine. 8th ed. New York: McGraw-Hill;2012. p. 2759–2766.10. Orfanos CE, Zouboulis CC, Almond-Roesler B, Geilen CC. Current use and future potential role of retinoids in dermatology. Drugs. 1997; 53:358–388.
Article11. Gollnick H, Cunliffe W, Berson D, Dreno B, Finlay A, Leyden JJ, et al. Management of acne: a report from a Global Alliance to Improve Outcomes in Acne. J Am Acad Dermatol. 2003; 49:1 Suppl. S1–S37.12. Thielitz A, Krautheim A, Gollnick H. Update in retinoid therapy of acne. Dermatol Ther. 2006; 19:272–279.
Article13. Cunliffe WJ, van de, Caputo R, Cavicchini S, Cooper A, Fyrand OL, et al. Roaccutane treatment guidelines: results of an international survey. Dermatology. 1997; 194:351–357.
Article14. Ellis CN, Krach KJ. Uses and complications of isotretinoin therapy. J Am Acad Dermatol. 2001; 45:S150–S157.
Article15. Almond-Roesler B, Blume-Peytavi U, Bisson S, Krahn M, Rohloff E, Orfanos CE. Monitoring of isotretinoin therapy by measuring the plasma levels of isotretinoin and 4-oxo-isotretinoin. A useful tool for management of severe acne. Dermatology. 1998; 196:176–181.
Article16. Wauquier F, Barquissau V, Léotoing L, Davicco MJ, Lebecque P, Mercier S, et al. Borage and fish oils lifelong supplementation decreases inflammation and improves bone health in a murine model of senile osteoporosis. Bone. 2012; 50:553–561.
Article17. Kim DH, Yoo TH, Lee SH, Kang HY, Nam BY, Kwak SJ, et al. Gamma linolenic acid exerts anti-inflammatory and anti-fibrotic effects in diabetic nephropathy. Yonsei Med J. 2012; 53:1165–1175.
Article18. Chang CS, Sun HL, Lii CK, Chen HW, Chen PY, Liu KL. Gamma-linolenic acid inhibits inflammatory responses by regulating NF-kappaB and AP-1 activation in lipopolysaccharide-induced RAW 264.7 macrophages. Inflammation. 2010; 33:46–57.
Article19. Chapkin RS, Ziboh VA. Inability of skin enzyme preparations to biosynthesize arachidonic acid from linoleic acid. Biochem Biophys Res Commun. 1984; 124:784–792.
Article20. Kawamura A, Ooyama K, Kojima K, Kachi H, Abe T, Amano K, et al. Dietary supplementation of gamma-linolenic acid improves skin parameters in subjects with dry skin and mild atopic dermatitis. J Oleo Sci. 2011; 60:597–607.
Article21. Chung S, Kong S, Seong K, Cho Y. Gamma-linolenic acid in borage oil reverses epidermal hyperproliferation in guinea pigs. J Nutr. 2002; 132:3090–3097.
Article22. Kobayashi H, Tagami H. Functional properties of the surface of the vermilion border of the lips are distinct from those of the facial skin. Br J Dermatol. 2004; 150:563–567.
Article23. Picardo M, Ottaviani M, Camera E, Mastrofrancesco A. Sebaceous gland lipids. Dermatoendocrinol. 2009; 1:68–71.
Article24. Pappas A. Epidermal surface lipids. Dermatoendocrinol. 2009; 1:72–76.
Article25. Chapkin RS, Ziboh VA, Marcelo CL, Voorhees JJ. Metabolism of essential fatty acids by human epidermal enzyme preparations: evidence of chain elongation. J Lipid Res. 1986; 27:945–954.
Article26. Brenner RR. Nutritional and hormonal factors influencing desaturation of essential fatty acids. Prog Lipid Res. 1981; 20:41–47.
Article27. Proksch E, Holleran WM, Menon GK, Elias PM, Feingold KR. Barrier function regulates epidermal lipid and DNA synthesis. Br J Dermatol. 1993; 128:473–482.
Article28. Ziboh VA, Cho Y, Mani I, Xi S. Biological significance of essential fatty acids/prostanoids/lipoxygenase-derived monohydroxy fatty acids in the skin. Arch Pharm Res. 2002; 25:747–758.
Article29. Brosche T, Platt D. Effect of borage oil consumption on fatty acid metabolism, transepidermal water loss and skin parameters in elderly people. Arch Gerontol Geriatr. 2000; 30:139–150.
Article30. De Spirt S, Stahl W, Tronnier H, Sies H, Bejot M, Maurette JM, et al. Intervention with flaxseed and borage oil supplements modulates skin condition in women. Br J Nutr. 2009; 101:440–445.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Effect of Oral Isotretinoin on the Barrier Function of the Lipsof Acne Patients and the Protective Role of Moisturizer
- The Efficacy of Topical Tacrolimus Ointment on Cheilitis Induced by Isotretinoin Treatment in Acne Vulgaris Patients
- Evening Primrose (Oenothera biennis) Oil in Management of Female Ailments
- Effect of Evening Primrose Oil on Postmenopausal Psychological Symptoms: A Triple-Blind Randomized Clinical Trial
- Development of a Complete Atrioventricular Block Associated with Intake of Evening Primrose Oil