Association between the clinical index and disease severity in infants with acute bronchiolitis
- Affiliations
-
- 1Department of Pediatrics, Seoul National University College of Medicine, Seoul, Korea. dongins0@snu.ac.kr
- KMID: 2262597
- DOI: http://doi.org/10.4168/aard.2013.1.4.377
Abstract
- PURPOSE
We aimed to verify whether the formal clinical index derived from infants and toddlers have a good association with the disease severity when we confine subjects to only infants, who undergo profound changes physically and immunologically.
METHODS
We retrospectively reviewed the medical records of hospitalized infants with acute bronchiolitis caused by respiratory syncytial virus between January 1, 2010 and December 31, 2011 in three hospitals. The age, respiratory rate, presentation of chest retraction, and percutaneous oxygen saturation upon admission; presentation of fever, use of oxygen therapy and inhaled corticosteroid within 24 hours after admission were investigated. We then examined the effect of clinical index on severity of acute bronchiolitis; the mean length of stay, mean duration of fever and oxygen therapy.
RESULTS
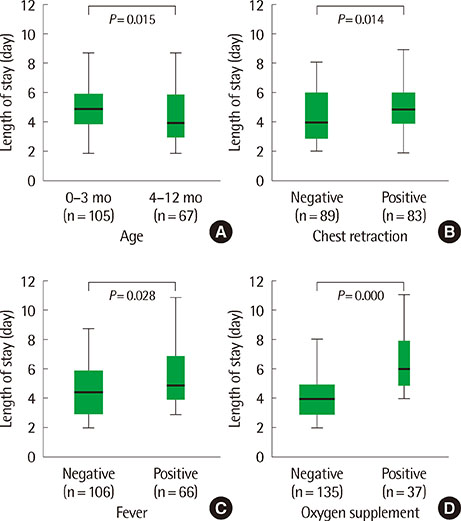
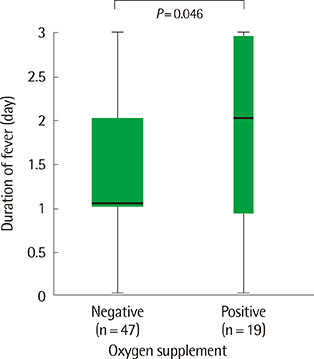
A total of 172 infants were studied. The mean length of stay was longer in patients younger than 3 months (P=0.015), in those with fever (P=0.028) and chest retraction (P=0.014), and in those who needed oxygen supplement (P=0.000). In the patients with fever, the mean duration of fever was longer in those who needed the oxygen supplement than those who did not (P=0.046).
CONCLUSION
Younger than 3 months of age, chest retraction upon admission; fever, need of oxygen supplement within 24 hours after admission may predict the severe course of infants with acute bronchiolitis.
MeSH Terms
Figure
Cited by 3 articles
-
Factors associated with obesity of acute bronchiolitis in infants: association of obesity with disease severity
Min Ah Cha, Yeol Ryoon Woo, Hyun Jin Kim, Min Sub Kim, Yeon Hwa Ahn
Allergy Asthma Respir Dis. 2015;3(4):281-287. doi: 10.4168/aard.2015.3.4.281.Clinical characteristics of patients with acute bronchiolitis who visited 146 Emergency Department in Korea in 2012
Eui Jung Roh, Youn Kyung Won, Mi-Hee Lee, Eun Hee Chung
Allergy Asthma Respir Dis. 2015;3(5):334-340. doi: 10.4168/aard.2015.3.5.334.Prediction of the severity and length of hospital stay in infants with acute bronchiolitis using the severity score
Yeongsang Jeong, Ji Hyen Hwang, Ji Yoon Kwon, Jeonghee Shin, Jung Hyun Kwon, Kyungdo Han, Won Hee Seo, Ji Tae Choung
Allergy Asthma Respir Dis. 2016;4(6):429-435. doi: 10.4168/aard.2016.4.6.429.
Reference
-
1. American Academy of Pediatrics Subcommittee on Diagnosis and Management of Bronchiolitis. Diagnosis and management of bronchiolitis. Pediatrics. 2006; 118:1774–1793.2. Cheong HY, Lee JH, Kim YB, Nam HS, Choi YJ, Kim CJ, et al. Viral etiologic agents in acute viral lower respiratory tract detected by multiplex RT-PCR. Pediatr Allergy Respir Dis. 2007; 17:334–353.3. Kim HJ, Kim JH, Kang IJ. Association of respiratory viral infection and atopy with severity of acute bronchiolitis in infants. Pediatr Allergy Respir Dis. 2011; 21:302–312.
Article4. Mulholland EK, Olinsky A, Shann FA. Clinical findings and severity of acute bronchiolitis. Lancet. 1990; 335:1259–1261.
Article5. Shay DK, Holman RC, Newman RD, Liu LL, Stout JW, Anderson LJ. Bronchiolitis-associated hospitalizations among US children, 1980-1996. JAMA. 1999; 282:1440–1446.
Article6. Lowell DI, Lister G, Von Koss H, McCarthy P. Wheezing in infants: the response to epinephrine. Pediatrics. 1987; 79:939–945.
Article7. Wang EE, Milner RA, Navas L, Maj H. Observer agreement for respiratory signs and oximetry in infants hospitalized with lower respiratory infections. Am Rev Respir Dis. 1992; 145:106–109.
Article8. Tal A, Bavilski C, Yohai D, Bearman JE, Gorodischer R, Moses SW. Dexamethasone and salbutamol in the treatment of acute wheezing in infants. Pediatrics. 1983; 71:13–18.
Article9. Baumer JH. SIGN guideline on bronchiolitis in infants. Arch Dis Child Educ Pract Ed. 2007; 92:ep149–ep151.
Article10. Shaw KN, Bell LM, Sherman NH. Outpatient assessment of infants with bronchiolitis. Am J Dis Child. 1991; 145:151–155.
Article11. Saunders M, Gorelick MH. Evaluation of the sick child in the office and clinic. In : Kliegman RM, Stanton BF, GemeIII JW, Schor NF, Behrman RE, editors. Nelson textbook of pediatrics. 19th ed. Philadelphia: Elsevier Saunders;2011. p. 280.12. Green M, Brayer AF, Schenkman KA, Wald ER. Duration of hospitalization in previously well infants with respiratory syncytial virus infection. Pediatr Infect Dis J. 1989; 8:601–605.
Article13. El-Radhi AS, Barry W, Patel S. Association of fever and severe clinical course in bronchiolitis. Arch Dis Child. 1999; 81:231–234.
Article14. McIntosh ED, De Silva LM, Oates RK. Clinical severity of respiratory syncytial virus group A and B infection in Sydney, Australia. Pediatr Infect Dis J. 1993; 12:815–819.
Article15. Schroeder AR, Marmor AK, Pantell RH, Newman TB. Impact of pulse oximetry and oxygen therapy on length of stay in bronchiolitis hospitalizations. Arch Pediatr Adolesc Med. 2004; 158:527–530.
Article16. Roback MG, Baskin MN. Failure of oxygen saturation and clinical assessment to predict which patients with bronchiolitis discharged from the emergency department will return requiring admission. Pediatr Emerg Care. 1997; 13:9–11.
Article17. Sarnaik AP, Heidemann SM. Respiratory pathophysiology and regulation. In : Kliegman RM, Stanton BF, GemeIII JW, Schor NF, Behrman RE, editors. Nelson textbook of pediatrics. 19th ed. Philadelphia: Elsevier Saunders;2011. p. 1419.18. El-Radhi AS, Carroll JE. Fever in paediatric practice. Oxford: Blackwell Scientific Publications;1994.19. Bernstein IL, Li JT, Bernstein DI, Hamilton R, Spector SL, Tan R, et al. Allergy diagnostic testing: an updated practice parameter. Ann Allergy Asthma Immunol. 2008; 100:3 Suppl 3. S1–S148.
Article20. Bradley JP, Bacharier LB, Bonfiglio J, Schechtman KB, Strunk R, Storch G, et al. Severity of respiratory syncytial virus bronchiolitis is affected by cigarette smoke exposure and atopy. Pediatrics. 2005; 115:e7–e14.
Article21. Koh YY, Jeong JH, Kim CK, Kim YK, Jee YK, Cho SH, et al. Atopic status and level of bronchial responsiveness in parents of children with acute bronchiolitis. J Asthma. 2000; 37:709–717.
Article22. Bamberger E, Srugo I, Abu Raya B, Segal E, Chaim B, Kassis I, et al. What is the clinical relevance of respiratory syncytial virus bronchiolitis?: findings from a multi-center, prospective study. Eur J Clin Microbiol Infect Dis. 2012; 31:3323–3330.
Article23. Bordley WC, Viswanathan M, King VJ, Sutton SF, Jackman AM, Sterling L, et al. Diagnosis and testing in bronchiolitis: a systematic review. Arch Pediatr Adolesc Med. 2004; 158:119–126.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Factors associated with obesity of acute bronchiolitis in infants: association of obesity with disease severity
- Association of Respiratory Viral Infection and Atopy with Severity of Acute Bronchiolitis in Infants
- Prediction of the severity and length of hospital stay in infants with acute bronchiolitis using the severity score
- The Relationship between the Time of First Respiratory Syncytial Virus Bronchiolitis and Later Wheezing and Asthma Development
- Bronchiolitis severity according to the infected viruses