Allergy Asthma Immunol Res.
2015 May;7(3):290-294. 10.4168/aair.2015.7.3.290.
Association Between PTPN22 Polymorphisms and IgE Responses to Staphylococcal Superantigens in Chronic Urticaria
- Affiliations
-
- 1Department of Biomedical Sciences, Ajou University School of Medicine, Suwon, Korea. hspark@ajou.ac.kr
- 2Department of Allergy and Clinical Immunology, Ajou University School of Medicine, Suwon, Korea.
- KMID: 2260467
- DOI: http://doi.org/10.4168/aair.2015.7.3.290
Abstract
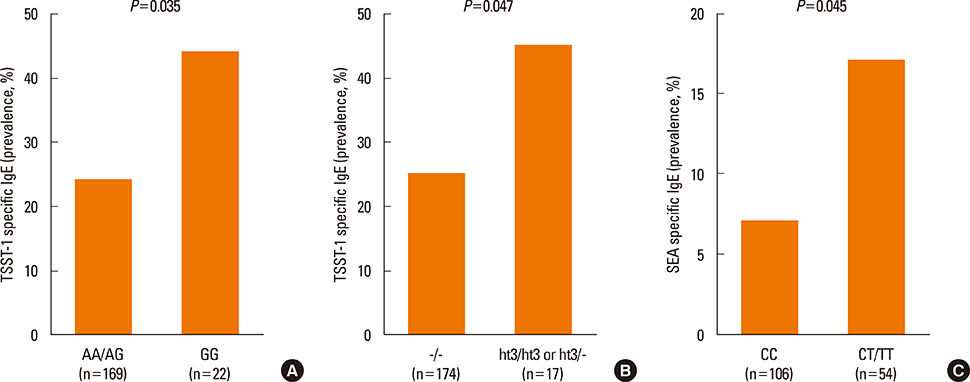
- Protein tyrosine phosphatase-22 (PTPN22) gene encodes lymphoid-specific tyrosine phosphatase (Lyp), an inhibitor of T cell activation. A polymorphism of the PTPN22 gene has been found to be associated with chronic urticaria (CU). We investigated the associations between PTPN22 gene polymorphisms and CU characteristics, including serum specific IgE antibodies response to toxic shock syndrome toxin-1 (TSST-1) and staphylococcal enterotoxin A (SEA). CU patients (n=409) and normal healthy controls (n=388) were enrolled in the present study. Serum specific IgE to TSST-1 and SEA were measured by ImmunoCAP(R). Five PTPN22 single nucleotide polymorphisms, -1123G>C, 1858C>T, 13145A>G, 14943C>T, and 20628A>G, were genotyped. There were no significant differences in genotype or haplotype frequencies of these polymorphisms between the 2 groups. CU patients carrying the GG genotype at 20628A>G (P=0.035) or haplotype 3 [GGG] (P=0.047) had a significantly higher prevalence of serum specific IgE to TSST-1 compared to non-carriers. Similarly, CT/TT genotype at 14943C>T had a significantly higher prevalence of serum specific IgE to SEA (P=0.045). The findings suggest that the PTPN22 gene polymorphisms at 20628A>G and 14943C>T may enhance serum specific IgE responses to TSST-1 and SEA, which may contribute to CU pathogenesis.
MeSH Terms
Figure
Reference
-
1. Kaplan AP. Treatment of chronic spontaneous urticaria. Allergy Asthma Immunol Res. 2012; 4:326–331.2. Greaves M. Chronic urticaria. J Allergy Clin Immunol. 2000; 105:664–672.3. Kaplan AP. Chronic urticaria: pathogenesis and treatment. J Allergy Clin Immunol. 2004; 114:465–474.4. Losol P, Yoo HS, Park HS. Molecular genetic mechanisms of chronic urticaria. Allergy Asthma Immunol Res. 2014; 6:13–21.5. Brzoza Z, Grzeszczak W, Rogala B, Trautsolt W, Moczulski D. PTPN22 polymorphism presumably plays a role in the genetic background of chronic spontaneous autoreactive urticaria. Dermatology. 2012; 224:340–345.6. Kawasaki E, Awata T, Ikegami H, Kobayashi T, Maruyama T, Nakanishi K, et al. Systematic search for single nucleotide polymorphisms in a lymphoid tyrosine phosphatase gene (PTPN22): association between a promoter polymorphism and type 1 diabetes in Asian populations. Am J Med Genet A. 2006; 140:586–593.7. Vang T, Miletic AV, Bottini N, Mustelin T. Protein tyrosine phosphatase PTPN22 in human autoimmunity. Autoimmunity. 2007; 40:453–461.8. Hidvégi B, Nagy E, Szabó T, Temesvári E, Marschalkó M, Kárpáti S, et al. Correlation between T-cell and mast cell activity in patients with chronic urticaria. Int Arch Allergy Immunol. 2003; 132:177–182.9. Losol P, Kim SH, Hwang EK, Shin YS, Park HS. IL-5 Promoter polymorphism enhances IgE responses to staphylococcal superantigens in adult asthmatics. Allergy Asthma Immunol Res. 2013; 5:106–109.10. Tomi NS, Kränke B, Aberer E. Staphylococcal toxins in patients with psoriasis, atopic dermatitis, and erythroderma, and in healthy control subjects. J Am Acad Dermatol. 2005; 53:67–72.11. Balci DD, Duran N, Ozer B, Gunesacar R, Onlen Y, Yenin JZ. High prevalence of Staphylococcus aureus cultivation and superantigen production in patients with psoriasis. Eur J Dermatol. 2009; 19:238–242.12. Liu JN, Shin YS, Yoo HS, Nam YH, Jin HJ, Ye YM, et al. The prevalence of serum specific IgE to superantigens in asthma and allergic rhinitis patients. Allergy Asthma Immunol Res. 2014; 6:263–266.13. Armerding D, van Reijsen FC, Hren A, Mudde GC. Induction of IgE and IgG1 in human B cell cultures with staphylococcal superantigens: role of helper T cell interaction, resistance to interferon-gamma. Immunobiology. 1993; 188:259–273.14. Ong PY, Patel M, Ferdman RM, Dunaway T, Church JA. Association of staphylococcal superantigen-specific immunoglobulin e with mild and moderate atopic dermatitis. J Pediatr. 2008; 153:803–806.15. Bunikowski R, Mielke M, Skarabis H, Herz U, Bergmann RL, Wahn U, et al. Prevalence and role of serum IgE antibodies to the Staphylococcus aureus-derived superantigens SEA and SEB in children with atopic dermatitis. J Allergy Clin Immunol. 1999; 103:119–124.16. Zuberbier T, Asero R, Bindslev-Jensen C, Walter Canonica G, Church MK, Giménez-Arnau A, et al. EAACI/GA(2)LEN/EDF/WAO guideline: definition, classification and diagnosis of urticaria. Allergy. 2009; 64:1417–1426.17. Kim SH, Choi JH, Lee KW, Kim SH, Shin ES, Oh HB, et al. The human leucocyte antigen-DRB1*1302-DQB1*0609-DPB1*0201 haplotype may be a strong genetic marker for aspirin-induced urticaria. Clin Exp Allergy. 2005; 35:339–344.18. Ye YM, Hur GY, Park HJ, Kim SH, Kim HM, Park HS. Association of specific IgE to staphylococcal superantigens with the phenotype of chronic urticaria. J Korean Med Sci. 2008; 23:845–851.19. Fousteri G, Liossis SN, Battaglia M. Roles of the protein tyrosine phosphatase PTPN22 in immunity and autoimmunity. Clin Immunol. 2013; 149:556–565.20. Burn GL, Svensson L, Sanchez-Blanco C, Saini M, Cope AP. Why is PTPN22 a good candidate susceptibility gene for autoimmune disease? FEBS Lett. 2011; 585:3689–3698.21. Taskapan MO, Kumar P. Role of staphylococcal superantigens in atopic dermatitis: from colonization to inflammation. Ann Allergy Asthma Immunol. 2000; 84:3–10.22. Cerosaletti K, Buckner JH. Protein tyrosine phosphatases and type 1 diabetes: genetic and functional implications of PTPN2 and PTPN22. Rev Diabet Stud. 2012; 9:188–200.23. Zhang J, Zahir N, Jiang Q, Miliotis H, Heyraud S, Meng X, et al. The autoimmune disease-associated PTPN22 variant promotes calpain-mediated Lyp/Pep degradation associated with lymphocyte and dendritic cell hyperresponsiveness. Nat Genet. 2011; 43:902–907.24. Durrant DM, Metzger DW. Emerging roles of T helper subsets in the pathogenesis of asthma. Immunol Invest. 2010; 39:526–549.25. Hasegawa K, Martin F, Huang G, Tumas D, Diehl L, Chan AC. PEST domain-enriched tyrosine phosphatase (PEP) regulation of effector/memory T cells. Science. 2004; 303:685–689.26. Jabara HH, Geha RS. The superantigen toxic shock syndrome toxin-1 induces CD40 ligand expression and modulates IgE isotype switching. Int Immunol. 1996; 8:1503–1510.27. Leung DY, Harbeck R, Bina P, Reiser RF, Yang E, Norris DA, et al. Presence of IgE antibodies to staphylococcal exotoxins on the skin of patients with atopic dermatitis. Evidence for a new group of allergens. J Clin Invest. 1993; 92:1374–1380.28. Saloga J, Leung DY, Reardon C, Giorno RC, Born W, Gelfand EW. Cutaneous exposure to the superantigen staphylococcal enterotoxin B elicits a T-cell-dependent inflammatory response. J Invest Dermatol. 1996; 106:982–988.29. Bhattacharyya SP, Drucker I, Reshef T, Kirshenbaum AS, Metcalfe DD, Mekori YA. Activated T lymphocytes induce degranulation and cytokine production by human mast cells following cell-to-cell contact. J Leukoc Biol. 1998; 63:337–341.30. Chang KL, Yang YH, Yu HH, Lee JH, Wang LC, Chiang BL. Analysis of serum total IgE, specific IgE and eosinophils in children with acute and chronic urticaria. J Microbiol Immunol Infect. 2013; 46:53–58.31. Goh CL, Tan KT. Chronic autoimmune urticaria: where we stand? Indian J Dermatol. 2009; 54:269–274.32. Godse KV. Chronic urticaria and treatment options. Indian J Dermatol. 2009; 54:310–312.33. Brzoza Z, Grzeszczak W, Trautsolt W, Moczulski D. Protein tyrosine phosphatase-22 (PTPN-22) polymorphism in the pathogenesis of chronic urticaria. Allergy. 2011; 66:1392–1393.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Association of Specific IgE to Staphylococcal Superantigens with the Phenotype of Chronic Urticaria
- Serum Specific IgE to Staphylococcal Superantigens in Sera of ASA-intolerant Asthma
- IL-5 Promoter Polymorphism Enhances IgE Responses to Staphylococcal Superantigens in Adult Asthmatics
- The Prevalence of Serum Specific IgE to Superantigens in Asthma and Allergic Rhinitis Patients
- Association between specific IgE to staphylococcal enterotoxin B and the eosinophilic phenotype of asthma