Allergy Asthma Immunol Res.
2014 Mar;6(2):126-130. 10.4168/aair.2014.6.2.126.
The Effects of Inhaled Albuterol in Transient Tachypnea of the Newborn
- Affiliations
-
- 1Department of Pediatrics, Dong-A University, College of Medicine, Busan, Korea.
- 2Department of Pediatrics, Pusan National University School of Medicine, Yangsan, Korea. neonate.kr@gmail.com
- KMID: 2260256
- DOI: http://doi.org/10.4168/aair.2014.6.2.126
Abstract
- PURPOSE
Transient tachypnea of the newborn (TTN) is a disorder caused by the delayed clearance of fetal alveolar fluid. beta-adrenergic agonists such as albuterol (salbutamol) are known to catalyze lung fluid absorption. This study examined whether inhalational salbutamol therapy could improve clinical symptoms in TTN. Additional endpoints included the diagnostic and therapeutic efficacy of salbutamol as well as its overall safety.
METHODS
From January 2010 through December 2010, we conducted a prospective study of 40 newborns hospitalized with TTN in the neonatal intensive care unit. Patients were given either inhalational salbutamol (28 patients) or placebo (12 patients), and clinical indices were compared.
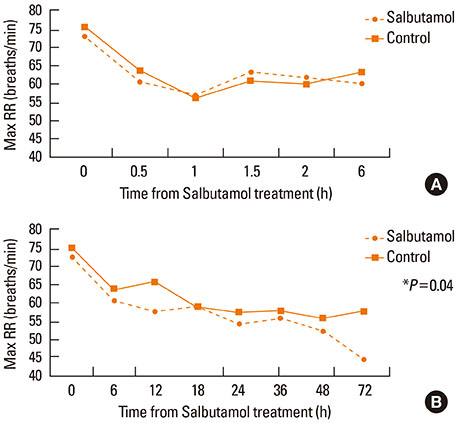
RESULTS
The duration of tachypnea was shorter in patients receiving inhalational salbutamol therapy, although this difference was not statistically significant. The duration of supplemental oxygen therapy and the duration of empiric antibiotic treatment were significantly shorter in the salbutamol-treated group. No adverse effects were observed in either treatment group.
CONCLUSIONS
Inhalational salbutamol therapy reduced the duration of supplemental oxygen therapy and the duration of empiric antibiotic treatment, with no adverse effects. However, the time between salbutamol therapy and clinical improvement was too long to allow definitive conclusions to be drawn. Further studies examining a larger number of patients with strict control over dosage and frequency of salbutamol inhalations are necessary to better direct the treatment of TTN.
MeSH Terms
Figure
Reference
-
1. Abu-Shaweesh JM. Respiratory disorders in preterm and term infants. In : Martin RJ, Fanaroff AA, Walsh MC, editors. Fanaroff and Martin's neonatal-perinatal medicine: diseases of the fetus and infant. 9th ed. St. Louis (MO): Elsevier Mosby;2010. p. 1162–1163.2. Clark RH. The epidemiology of respiratory failure in neonates born at an estimated gestational age of 34 weeks or more. J Perinatol. 2005; 25:251–257.3. Takaya A, Igarashi M, Nakajima M, Miyake H, Shima Y, Suzuki S. Risk factors for transient tachypnea of the newborn in infants delivered vaginally at 37 weeks or later. J Nippon Med Sch. 2008; 75:269–273.4. Lewis V, Whitelaw A. Furosemide for transient tachypnea of the newborn. Cochrane Database Syst Rev. 2002; (1):CD003064.5. Jain L, Eaton DC. Physiology of fetal lung fluid clearance and the effect of labor. Semin Perinatol. 2006; 30:34–43.6. Richardson BS, Czikk MJ, daSilva O, Natale R. The impact of labor at term on measures of neonatal outcome. Am J Obstet Gynecol. 2005; 192:219–226.7. Zanardo V, Simbi AK, Franzoi M, Soldà G, Salvadori A, Trevisanuto D. Neonatal respiratory morbidity risk and mode of delivery at term: influence of timing of elective caesarean delivery. Acta Paediatr. 2004; 93:643–647.8. Sakuma T, Tuchihara C, Ishigaki M, Osanai K, Nambu Y, Toga H, Takahashi K, Ohya N, Kurihara T, Matthay MA. Denopamine, a beta(1)-adrenergic agonist, increases alveolar fluid clearance in ex vivo rat and guinea pig lungs. J Appl Physiol. 2001; 90:10–16.9. Sakuma T, Folkesson HG, Suzuki S, Okaniwa G, Fujimura S, Matthay MA. Beta-adrenergic agonist stimulated alveolar fluid clearance in ex vivo human and rat lungs. Am J Respir Crit Care Med. 1997; 155:506–512.10. Mutlu GM, Factor P. Alveolar epithelial beta2-adrenergic receptors. Am J Respir Cell Mol Biol. 2008; 38:127–134.11. Irestedt L, Lagercrantz H, Hjemdahl P, Hägnevik K, Belfrage P. Fetal and maternal plasma catecholamine levels at elective cesarean section under general or epidural anesthesia versus vaginal delivery. Am J Obstet Gynecol. 1982; 142:1004–1010.12. Ronca AE, Abel RA, Ronan PJ, Renner KJ, Alberts JR. Effects of labor contractions on catecholamine release and breathing frequency in newborn rats. Behav Neurosci. 2006; 120:1308–1314.13. Smith DE, Otulakowski G, Yeger H, Post M, Cutz E, O'Brodovich HM. Epithelial Na(+) channel (ENaC) expression in the developing normal and abnormal human perinatal lung. Am J Respir Crit Care Med. 2000; 161:1322–1331.14. Perkins GD, Gao F, Thickett DR. In vivo and in vitro effects of salbutamol on alveolar epithelial repair in acute lung injury. Thorax. 2008; 63:215–220.15. Perkins GD, McAuley DF, Richter A, Thickett DR, Gao F. Bench-to-bedside review: beta2-Agonists and the acute respiratory distress syndrome. Crit Care. 2004; 8:25–32.16. Mutlu GM, Dumasius V, Burhop J, McShane PJ, Meng FJ, Welch L, Dumasius A, Mohebahmadi N, Thakuria G, Hardiman K, Matalon S, Hollenberg S, Factor P. Upregulation of alveolar epithelial active Na+ transport is dependent on beta2-adrenergic receptor signaling. Circ Res. 2004; 94:1091–1100.17. Welty S, Hansen TN, Corbet A. Respiratory distress in the preterm infant. In : Taeusch HW, Ballard RA, Gleason CA, Avery ME, editors. Avery's diseases of the newborn. 8th ed. Philadelphia (PA): Elsevior Saunders;2005. p. 697–699.18. Karabayir N. Intravenous furosemide therapy in transient tachypnea of the newborn. Pediatr Int. 2010; 52:851.19. Kasap B, Duman N, Ozer E, Tatli M, Kumral A, Ozkan H. Transient tachypnea of the newborn: predictive factor for prolonged tachypnea. Pediatr Int. 2008; 50:81–84.20. Fukuda N, Folkesson HG, Matthay MA. Relationship of interstitial fluid volume to alveolar fluid clearance in mice: ventilated vs. in situ studies. J Appl Physiol. 2000; 89:672–679.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Neonatal respiratory distress: recent progress in understanding pathogenesis and treatment outcomes
- Predictable risk factors and clinical courses for prolonged transient tachypnea of the newborn
- A Symptom-free Congenital Sliding Hiatal Hernia Diagnosed within 24 Hours after Birth
- Clinical assessment of neonatal transient tricuspid insufficiency: Doppler echocardiographic study
- Comparative Study on the Clinical Characteristics of Transient Tachypnea of Newborns according to the Need for Invasive Mechanical Ventilation