Korean J Hematol.
2006 Mar;41(1):66-71. 10.5045/kjh.2006.41.1.66.
Regression of Extensive Colonic Extranodal Marginal Zone B Cell Lymphoma after Treatment with Rituximab
- Affiliations
-
- 1Department of Internal Medicine, Research Institute of Clinical Medicine, Chonbuk National University Medical School, Jeonju, Korea. cyyim@chonbuk.ac.kr
- KMID: 2252331
- DOI: http://doi.org/10.5045/kjh.2006.41.1.66
Abstract
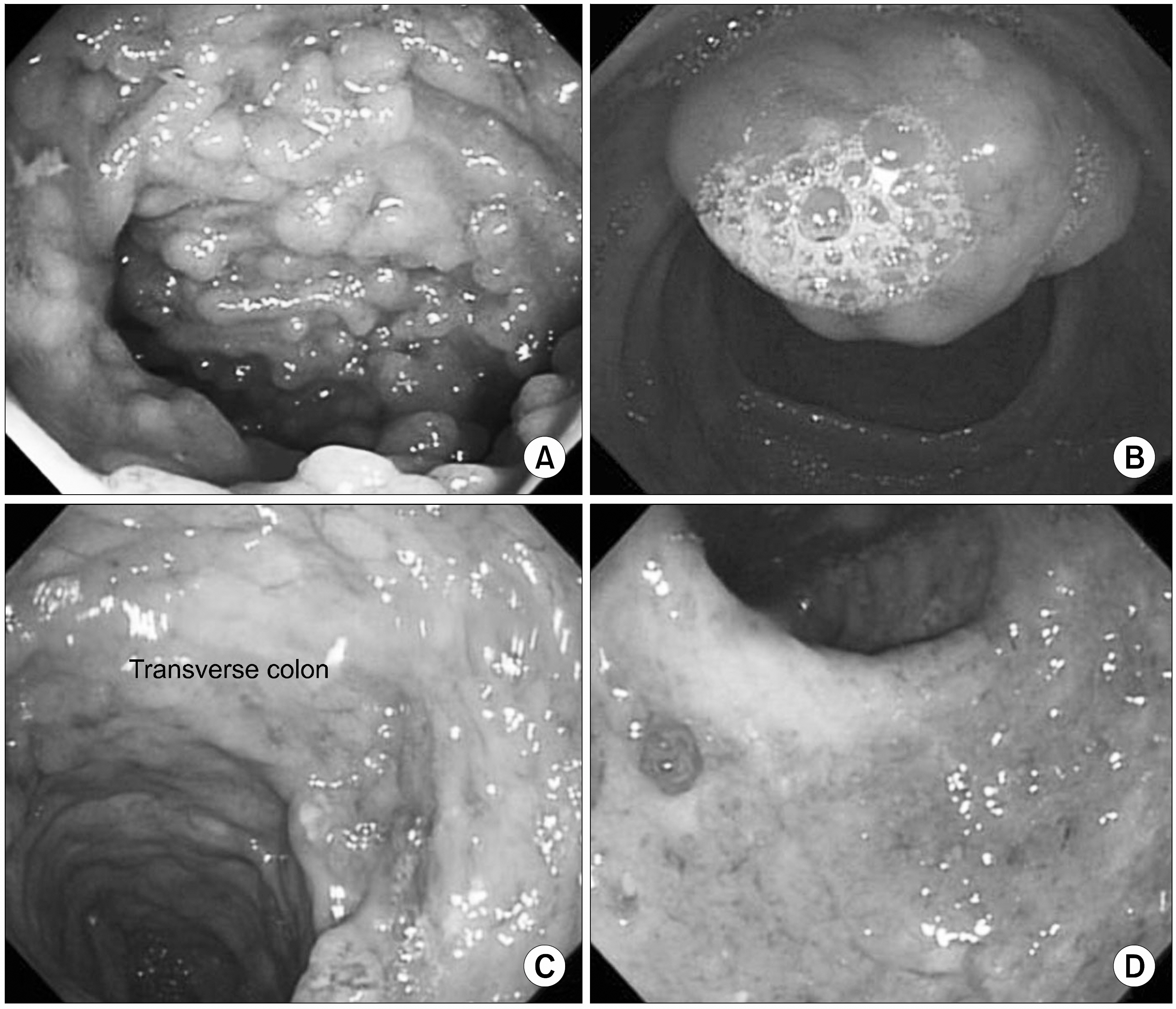
- We report here on a case of colonic extranodal marginal zone B-cell lymphoma of the mucosa-associated lymphoid tissue (MALT) in a 17-year-old male with a history of selective IgA deficiency. The colonoscopic findings showed prominent lymphoid hyperplasia along the terminal ileum and multiple ulceroinfiltrative nodular lesions at the transverse colon and rectum. Immunohistochemically, an extensive infiltration by a CD20-positive lymphoid cell population that displayed a prominent lymphoepithelial structure was detected. Multiple hypermetabolic lymph nodes were found in the cervical, axillary, mediastinal and abdominal regions, in addition to the colon, by performing PET-CT. After administering rituximab weekly for 4 weeks, he had significant regression of the colonic lesions and the lesions in multiple lymph nodes. He remains progression free 10 months after finishing the treatment. This case report demonstrates the potential efficacy of rituximab as a single therapeutic agent for patients with colonic extranodal marginal zone B-cell lymphoma, and even for a patient with an extensive disease status.
MeSH Terms
Figure
Cited by 1 articles
-
A Case of Mucosa-Associated Lymphoid Tissue Lymphoma of the Sigmoid Colon Presenting as a Semipedunculated Polyp
Myung Hwan Kim, Jin Tae Jung, Eui Jung Kim, Tae Won Kim, Seon Young Kim, Joong Goo Kwon, Eun Young Kim, Woo Jung Sung
Clin Endosc. 2014;47(2):192-196. doi: 10.5946/ce.2014.47.2.192.
Reference
-
1). Pileri SA., Milani M., Fraternali-Orcii G., Sabattini E. From the R.E.A.L classification to the upcoming WHO scheme: a step towards universal categorization of lymphoma entities? Ann Oncol. 1998. 9:607–12.2). Cavalli F., Isaacson PG., Gascoyne RD., Zucca E. MALT lymphomas. Heamtology (Am Soc Hematol Educ Program). 2001. 241–58.
Article3). Wotherspoon AC., Ortiz-Hidalgo C., Falzon MR., Isaacson PG. Helicobacter pylori-associated gastritis and primary B-cell gastric lymphoma. Lancet. 1991. 338:1175–6.4). Hyjek E., Smith WJ., Isaacson PG. Primary B-cell lymphoma of salivary glands and its relationship to myoepithelial sialadnitis. Hum Pathol. 1988. 19:766–76.5). Hyjek E., Isaacson PG. Primary B cell lymphoma of the thyroid and its relationship to Hashimoto's thyroiditis. Hum Pathol. 1988. 19:1315–26.
Article6). Coiffier B. Immunochemotherapy: the new standard in aggressive non-Hodgkin's lymphoma in the elderly. Semin Oncol. 2003. 30(Suppl 2):21–7.
Article7). Coiffier B. Rituximab in combination with CHOP improves survival in elderly patients with aggressive non-Hodgkin's lymphoma. Semin Oncol. 2002. 29(Suppl 6):18–22.
Article8). Hainsworth JD., Litchy S., Burris HA 3rd, et al. Rituximab as first-line and maintenance therapy for patients with indolent non-Hodgkin's lymphoma. J Clin Oncol. 2002. 20:4261–7.
Article9). Mclaughlin P., Grillo-Lopez AJ., Link BK, et al. Rituximab chimeric anti-CD20 monoclonal antibody therapy for relapsed indolent lymphoma: half of patients respond to a four-dose treatment program. J Clin Oncol. 1998. 16:2825–33.
Article10). Conconi A., Martinelli G., Thieblemont C, et al. Clinical activity of rituximab in extranodal marginal zone B-cell lymphoma of MALT type. Blood. 2003. 102:2741–5.
Article11). Martinelli G., Laszlo D., Ferreri A, et al. Clinical activity of rituximab in gastric marginal zone non-Hodgkin's lymphoma resistant to or not eligible for anti-Helicobacter pylori therapy. J Clin Oncol. 2005. 23:1979–83.
Article12). Chong EA., Svoboda J., Cherian S, et al. Regression of pulmonary MALT lymphoma after treatment with rituximab. Leuk Lymphoma. 2005. 46:1383–6.
Article13). Nuckel H., Meller D., Steuhl KP., Duhrsen U. Anti-CD20 monoclonal antibody therapy in relapsed MALT lymphoma of the conjunctiva. Eur J Haematol. 2004. 73:258–62.14). Foxton MR., Knight L., Knisely AS, et al. Liver transplantation for HCV-related cirrhosis in a patient with gastric mucosa-associated lymphoma (MALToma) pre-treated with rituximab. Liver Transpl. 2005. 11:839–42.
Article15). Raderer M., Jager G., Brugger S, et al. Rituximab for treatment of advanced extranodal marginal zone B cell lymphoma of the mucosa-associated lymphoid tissue lymphoma. Oncology. 2003. 65:306–10.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Primary Pulmonary Extranodal Marginal Zone B-Cell Lymphoma of the MALT Type
- Clinical Study of Ocular Adnexal Extranodal Marginal Zone B-cell Lymphoma: From the Perspective of Dermatology
- A case of nodal marginal zone B-cell lymphoma of the lower eyelid
- Endoscopic Findings of Gastric Extranodal Marginal Zone B-Cell Mucosa-Associated Lymphoid Tissue Lymphoma
- A Case of Synchronous Lung Adenocarcinoma and Extranodal Marginal Zone B-Cell Lymphoma of Mucosa-Associated Lymphoid Tissue (MALT) Type