Tuberc Respir Dis.
2012 Jul;73(1):61-66. 10.4046/trd.2012.73.1.61.
A Case of Synchronous Lung Adenocarcinoma and Extranodal Marginal Zone B-Cell Lymphoma of Mucosa-Associated Lymphoid Tissue (MALT) Type
- Affiliations
-
- 1Department of Internal Medicine, Keimyung University School of Medicine, Daegu, Korea.
- 2Department of Pathology, Keimyung University School of Medicine, Daegu, Korea. jcy2475@dsmc.or.kr
- KMID: 2050676
- DOI: http://doi.org/10.4046/trd.2012.73.1.61
Abstract
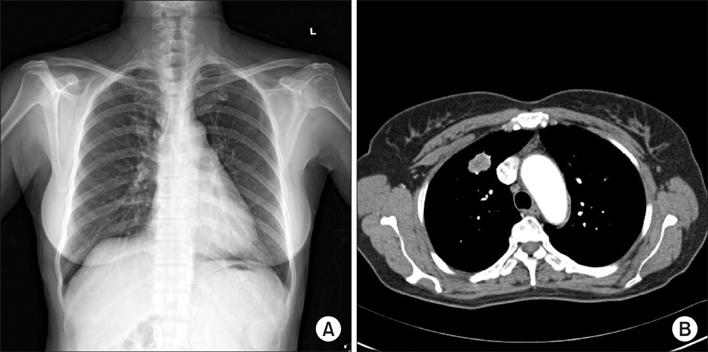
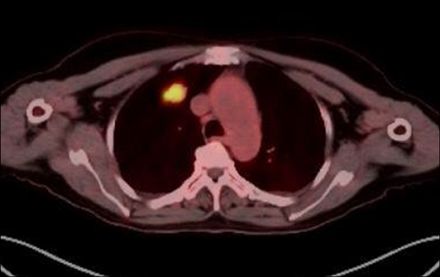
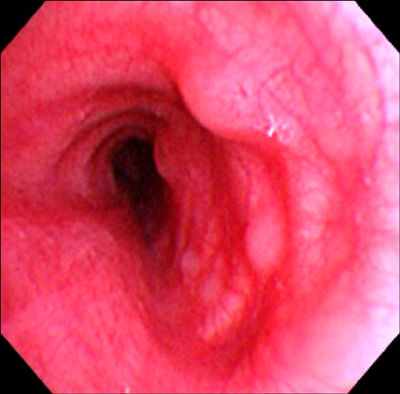
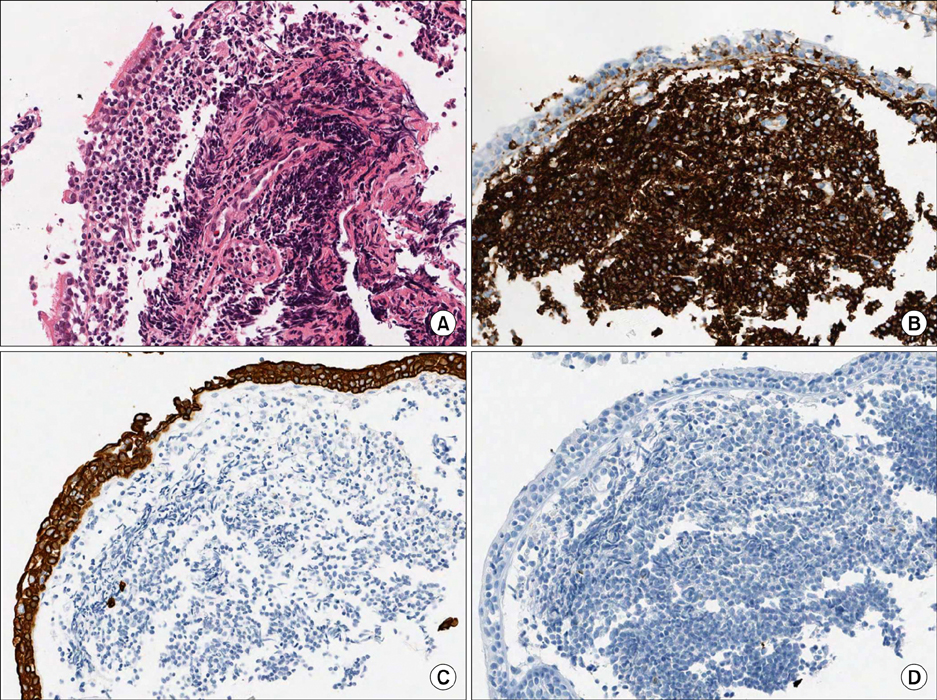
- Extranodal marginal zone B-cell lymphoma of mucosa-associated lymphoid tissue type (extranodal MZL) is a distinct subgroup of non-Hodgkin's lymphoma. Pulmonary extranodal MZL is a rare entity and accounts for less than 0.5% of primary pulmonary malignancies. Only a few cases of simultaneous occurrence of lung cancer and pulmonary extranodal MZL have been reported. A 60-year-old woman was referred to our hospital with a pulmonary nodule. She was diagnosed with lung adenocarcinoma by percutaneous needle biopsy. The protrusions into the left main bronchus were found by accident while performing bronchoscopy during lung cancer evaluation. The bronchial lesions were diagnosed as extranodal MZL. Although the patient underwent surgical resection for the lung adenocarcinoma, the pulmonary extranodal MZL was left untreated; it was monitored during follow-up visits. To our knowledge, this is the first report of synchronous lung adenocarcinoma and primary extranodal MZL of the main bronchus.
MeSH Terms
Figure
Reference
-
1. Armitage JO, Weisenburger DD. New approach to classifying non-Hodgkin's lymphomas: clinical features of the major histologic subtypes. Non-Hodgkin's Lymphoma Classification Project. J Clin Oncol. 1998. 16:2780–2795.2. Harris NL, Jaffe ES, Stein H, Banks PM, Chan JK, Cleary ML, et al. A revised European-American classification of lymphoid neoplasms: a proposal from the International Lymphoma Study Group. Blood. 1994. 84:1361–1392.3. Zucca E, Conconi A, Pedrinis E, Cortelazzo S, Motta T, Gospodarowicz MK, et al. Nongastric marginal zone B-cell lymphoma of mucosa-associated lymphoid tissue. Blood. 2003. 101:2489–2495.4. Jaffe ES, Harris NL, Stein H, Vardiman JW. World Health Organization classification of tumours: pathology and genetics of tumours of haematopoietic and lymphoid tissues. 2001. Lyon: IARC Press.5. Ahmed S, Siddiqui AK, Rai KR. Low-grade B-cell bronchial associated lymphoid tissue (BALT) lymphoma. Cancer Invest. 2002. 20:1059–1068.6. Koss MN. Malignant and benign lymphoid lesions of the lung. Ann Diagn Pathol. 2004. 8:167–187.7. Travis WD, Brambilla E, Müller-Hermelink HK, Harris CC. World Health Organization classification of tumours: pathology and genetics of tumours of the lung, pleura, thymus and heart. 2004. Lyon: IARC Press.8. Wotherspoon AC, Isaacson PG. Synchronous adenocarcinoma and low grade B-cell lymphoma of mucosa associated lymphoid tissue (MALT) of the stomach. Histopathology. 1995. 27:325–331.9. Suzuki T, Akizawa T, Suzuki H, Kitazume K, Omine M, Mitsuya T. Primary tracheal mucosa-associated lymphoid tissue lymphoma accompanying lung cancer. Common tumorigenesis or coincidental coexistence? Jpn J Thorac Cardiovasc Surg. 2000. 48:817–819.10. Chanel S, Burke L, Fiche M, Molina T, Lerochais JP, Icard P, et al. Synchronous pulmonary adenocarcinoma and extranodal marginal zone/low-grade B-cell lymphoma of MALT type. Hum Pathol. 2001. 32:129–132.11. Ichihara E, Tabata M, Takigawa N, Sato Y, Kondo E, Aoe M, et al. Synchronous pulmonary MALT lymphoma and pulmonary adenocarcinoma after metachronous gastric MALT lymphoma and gastric adenocarcinoma. J Thorac Oncol. 2008. 3:1362–1363.12. Solomonov A, Zuckerman T, Goralnik L, Ben-Arieh Y, Rowe JM, Yigla M. Non-Hodgkin's lymphoma presenting as an endobronchial tumor: report of eight cases and literature review. Am J Hematol. 2008. 83:416–419.13. Isaacson P, Wright DH. Malignant lymphoma of mucosa-associated lymphoid tissue. A distinctive type of B-cell lymphoma. Cancer. 1983. 52:1410–1416.14. Oh SY, Kim WS, Kim JS, Kim SJ, Kwon HC, Lee DH, et al. Pulmonary marginal zone B-cell lymphoma of MALT type--what is a prognostic factor and which is the optimal treatment, operation, or chemotherapy?: Consortium for Improving Survival of Lymphoma (CISL) study. Ann Hematol. 2010. 89:563–568.15. Ahmed S, Kussick SJ, Siddiqui AK, Bhuiya TA, Khan A, Sarewitz S, et al. Bronchial-associated lymphoid tissue lymphoma: a clinical study of a rare disease. Eur J Cancer. 2004. 40:1320–1326.16. Bae YA, Lee KS, Han J, Ko YH, Kim BT, Chung MJ, et al. Marginal zone B-cell lymphoma of bronchus-associated lymphoid tissue: imaging findings in 21 patients. Chest. 2008. 133:433–440.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Primary Pulmonary Extranodal Marginal Zone B-Cell Lymphoma of the MALT Type
- A Case of Mucosa-Associated Lymphoid Tissue Lymphoma in Nasopharynx and Thyroid Gland
- Mucosa-associated Lymphoid Tissue Lymphoma of Parotid Gland
- Gastrointestinal Lymphoma
- Role of Chemotherapy in Gastric Marginal Zone B-Cell Lymphoma of Mucosa-Associated Lymphoid Tissue (MALT) Type