Korean J Hepatobiliary Pancreat Surg.
2011 Nov;15(4):237-242. 10.14701/kjhbps.2011.15.4.237.
Predictive factors for invasive intraductal papillary mucinous neoplasm of the pancreas
- Affiliations
-
- 1Department of Surgery, Kyungpook National University School of Medicine, Daegu, Korea.
- 2Department of Surgery, Kyungpook National University Medical Center, Daegu, Korea. kwonhj95@naver.com, ksg@knu.ac.kr
- 3Department of Family Medicine, Daegu Catholic University College of Medicine, Daegu, Korea.
- KMID: 2244131
- DOI: http://doi.org/10.14701/kjhbps.2011.15.4.237
Abstract
- BACKGROUNDS/AIMS
Intraductal papillary mucinous neoplasm (IPMN) of the pancreas has malignant potential. Predicting invasive IPMN has proven difficult and controversial. We tried to identify predictive factors for invasive IPMN.
METHODS
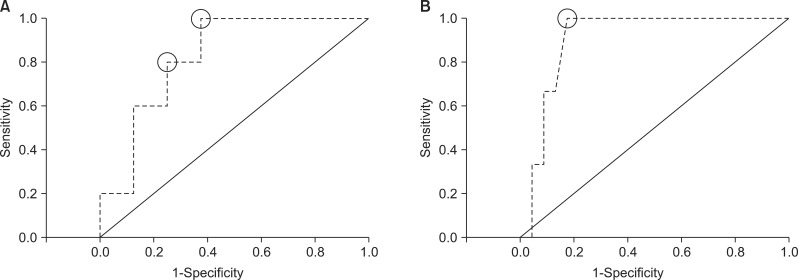
Thirty six patients underwent resection for IPMN from February 2001 to July 2011. Clinicopathological features including demographic, imaging, microscopic, and serological findings were retrospectively reviewed. Receiver operating characteristic (ROC) curve analysis was used to analyze sensitivity and specificity of all possible cut-off values for the diameter of the main pancreatic duct and mass size predicting invasive IPMN. Student t-test, chi-square test, and logistic regression were used for univariate and multivariate analysis.
RESULTS
The mean age was 63.5+/-8.4 years. Males were more commonly affected (58.3% vs 41.7%). Pancreaticoduodenectomy was performed in 55.6% of patients, distal pancreatectomy in 36.1%, and central pancreatic resection in 8.3%. Non-invasive IPMNs were present in 80.6% (n=29), whereas invasive IPMNs were present in 19.4% (n=7). In univariate analysis, tumor location (p=0.036), Kuroda classification (p=0.048), mural nodule (p=0.016), and main duct dilatation (> or =8 mm) (p=0.006) were statistically significant variables. ROC curve analysis showed that a value of 8 mm for the main duct dilatation and a value of 35 mm for the size of the mass lesion have 80% sensitivity and 75% specificity and 100% sensitivity and 82.6% specificity, respectively. However, in multivariate analysis, main ductal dilatation (> or =8 mm) was identified to be the only independent factor for invasive IPMN (p=0.049).
CONCLUSIONS
Main duct dilatation appears to be a useful indicator for predicting invasive IPMN.
MeSH Terms
Figure
Reference
-
1. Kloppel G, Solcia E, Longnecker DS, et al. World Health Organization International Histological Classification of Tumours: Histological Typing of Tumors of the Exocrine Pancreas. 1996. 2nd ed. Berlin: Springer-Verlag.2. Cho KR, Vogelstein B. Genetic alterations in the adenoma--carcinoma sequence. Cancer. 1992; 70(6 Suppl):1727–1731. PMID: 1516027.
Article3. Wilentz RE, Hruban RH. Pathology of cancer of the pancreas. Surg Oncol Clin N Am. 1998; 7:43–65. PMID: 9443986.
Article4. Taouli B, Vilgrain V, O'Toole D, Vullierme MP, Terris B, Menu Y. Intraductal papillary mucinous tumors of the pancreas: features with multimodality imaging. J Comput Assist Tomogr. 2002; 26:223–231. PMID: 11884778.
Article5. Sohn TA, Yeo CJ, Cameron JL, et al. Intraductal papillary mucinous neoplasms of the pancreas: an updated experience. Ann Surg. 2004; 239:788–797. PMID: 15166958.6. Klimstra DS. Cystic, mucin-producing neoplasms of the pancreas: the distinguishing features of mucinous cystic neoplasms and intraductal papillary mucinous neoplasms. Semin Diagn Pathol. 2005; 22:318–329. PMID: 16939060.
Article7. Bosman FT, Carneiro F, Hruban RH, et al. WHO Classification of Tumours of the Digestive System: Tumours of the Pancreas. 2010. 4th ed. Berlin: Springer.8. Baba T, Yamaguchi T, Ishihara T, et al. Distinguishing benign from malignant intraductal papillary mucinous tumors of the pancreas by imaging techniques. Pancreas. 2004; 29:212–217. PMID: 15367887.
Article9. Chiu SS, Lim JH, Lee WJ, et al. Intraductal papillary mucinous tumour of the pancreas: differentiation of malignancy and benignancy by CT. Clin Radiol. 2006; 61:776–783. PMID: 16905386.
Article10. Sahani DV, Kadavigere R, Blake M, et al. Intraductal papillary mucinous neoplasm of pancreas: multi-detector row CT with 2D curved reformations--correlation with MRCP. Radiology. 2006; 238:560–569. PMID: 16436817.
Article11. Ogawa H, Itoh S, Ikeda M, Suzuki K, Naganawa S. Intraductal papillary mucinous neoplasm of the pancreas: assessment of the likelihood of invasiveness with multisection CT. Radiology. 2008; 248:876–886. PMID: 18632526.
Article12. Jang JY, Kim SW, Ahn YJ, et al. Multicenter analysis of clinicopathologic features of intraductal papillary mucinous tumor of the pancreas: is it possible to predict the malignancy before surgery? Ann Surg Oncol. 2005; 12:124–132. PMID: 15827792.
Article13. Tanaka M, Chari S, Adsay V, et al. International Association of Pancreatology. International consensus guidelines for management of intraductal papillary mucinous neoplasms and mucinous cystic neoplasms of the pancreas. Pancreatology. 2006; 6:17–32. PMID: 16327281.
Article14. Pelaez-Luna M, Chari ST, Smyrk TC, et al. Do consensus indications for resection in branch duct intraductal papillary mucinous neoplasm predict malignancy? A study of 147 patients. Am J Gastroenterol. 2007; 102:1759–1764. PMID: 17686073.
Article15. Kobayashi G, Fujita N, Noda Y, et al. Mode of progression of intraductal papillary-mucinous tumor of the pancreas: analysis of patients with follow-up by EUS. J Gastroenterol. 2005; 40:744–751. PMID: 16082592.
Article16. Yamaguchi T, Baba T, Ishihara T, et al. Long-term follow-up of intraductal papillary mucinous neoplasm of the pancreas with ultrasonography. Clin Gastroenterol Hepatol. 2005; 3:1136–1143. PMID: 16271346.
Article17. Schmidt CM, White PB, Waters JA, et al. Intraductal papillary mucinous neoplasms: predictors of malignant and invasive pathology. Ann Surg. 2007; 246:644–651. PMID: 17893501.18. Lee CJ, Scheiman J, Anderson MA, et al. Risk of malignancy in resected cystic tumors of the pancreas < or =3 cm in size: is it safe to observe asymptomatic patients? A multi-institutional report. J Gastrointest Surg. 2008; 12:234–242. PMID: 18040749.19. Bassi C, Crippa S, Salvia R. Intraductal papillary mucinous neoplasms (IPMNs): is it time to (sometimes) spare the knife? Gut. 2008; 57:287–289. PMID: 18268051.
Article20. Vullierme MP, Giraud-Cohen M, Hammel P, et al. Malignant intraductal papillary mucinous neoplasm of the pancreas: in situ versus invasive carcinoma surgical resectability. Radiology. 2007; 245:483–490. PMID: 17848678.21. Yamada Y, Mori H, Matsumoto S, Kamei N, Hongo N. Invasive carcinomas derived from intraductal papillary mucinous neoplasms of the pancreas: a long-term follow-up assessment with CT imaging. J Comput Assist Tomogr. 2006; 30:885–890. PMID: 17082690.22. Cho JH, Park SJ, Lee SM, et al. Surgical treatment of intraductal papillary mucinous tumor of the pancreas. Korean J Hepatobiliary Pancreat Surg. 2007; 11:36–41.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Intraductal Papillary Mucinous Tumor Simultaneously Involving the Liver and Pancreas: A Case Report
- Oncocytic Type Intraductal Papillary Mucinous Neoplasm Mimicking Mucinous Cystic Neoplasm of the Pancreas: A Case Report
- Evaluation of malignant intraductal papillary mucinous neoplasms of the pancreas on computed tomography and magnetic resonance imaging
- Squamous cell carcinoma of the pancreas with a pancreatic intraductal papillary mucinous neoplasm: a case report
- A Case of Intraductal Papillary Mucinous Tumor of the Pancreas with Scant Mucin Production