Korean J Hepatobiliary Pancreat Surg.
2012 Nov;16(4):138-141. 10.14701/kjhbps.2012.16.4.138.
Clinicopathological features of the intraductal papillary neoplasms of the intrahepatic bile duct
- Affiliations
-
- 1Department of Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. shwang@amc.seoul.kr
- KMID: 2243191
- DOI: http://doi.org/10.14701/kjhbps.2012.16.4.138
Abstract
- BACKGROUNDS/AIMS
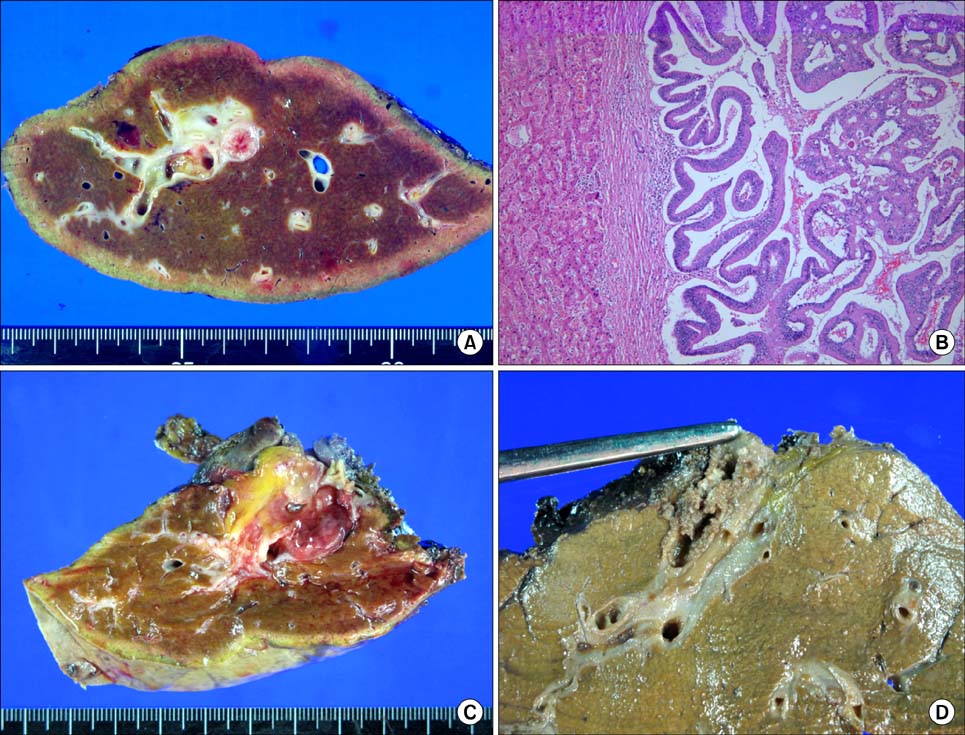
This study is intended to investigate the clinicopathological features of the intraductal papillary neoplasms of the intrahepatic bile duct (IPNB), especially focused on malignant changes.
METHODS
From the institutional database of liver resection cases (Asan Medical Center, University of Ulsan College of Medicine), 18 patients who met the definition of IPNB were selected. They had undergone liver resection between February 2002 and October 2006; thus, the follow-up period was more than 5 years.
RESULTS
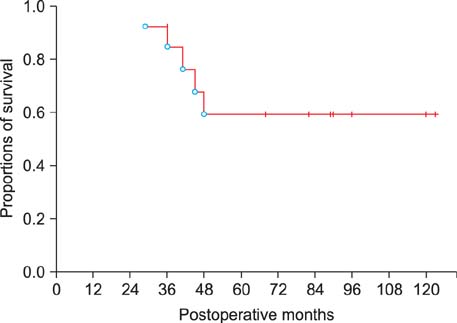
Of the 18 patients, 11 patients were male. Their mean age was 61.3+/-6.7 years. There were no differences between the non-malignant and malignant lesions, in the comparison of the CEA levels (5.6+/-2.7 vs.12.6+/-31.1 ng/ml, p=0.439) and the CA19-9 levels (29.2+/-34.7 vs.31.9+/-30.2 ng/ml, p=0.871). The common radiologic findings were: intraductal growing mass in 10; bile duct dilatation in 6; and saccular duct dilatation in 2. Left and right hepatectomies were performed in 15 and 3, respectively. Five patients showed benign lesions of IPNB, and 13 patients revealed malignant lesions of intraductal papillary adnocarcinoma or cholangiocarcinoma. All 4 patients with benign lesions survived for a mean period of 53 months without recurrence. In 13 patients with the malignant lesions, 1-year, 3-year, and 5-year survival rates were 100%, 84.6%, and 59.2%, respectively.
CONCLUSIONS
We concluded that intrahepatic IPNB is a rare type of biliary neoplasm which includes a histological spectrum, ranging from benign disease to invasive malignancy. The long-term survival was anticipated after complete curative resection.
MeSH Terms
Figure
Cited by 1 articles
-
Intrahepatic and extrahepatic intraductal papillary neoplasms of bile duct
Myunghee Yoon
Korean J Hepatobiliary Pancreat Surg. 2013;17(1):48-52. doi: 10.14701/kjhbps.2013.17.1.48.
Reference
-
1. Itatsu K, Zen Y, Ohira S, et al. Immunohistochemical analysis of the progression of flat and papillary preneoplastic lesions in intrahepatic cholangiocarcinogenesis in hepatolithiasis. Liver Int. 2007. 27:1174–1184.2. Jang KT, Hong SM, Lee KT, et al. Intraductal papillary neoplasm of the bile duct associated with Clonorchis sinensis infection. Virchows Arch. 2008. 453:589–598.3. Nakanuma Y, Sato Y, Harada K, et al. Pathological classification of intrahepatic cholangiocarcinoma based on a new concept. World J Hepatol. 2010. 2:419–427.4. Zen Y, Fujii T, Itatsu K, et al. Biliary papillary tumors share pathological features with intraductal papillary mucinous neoplasm of the pancreas. Hepatology. 2006. 44:1333–1343.5. Shimonishi T, Sasaki M, Nakanuma Y. Precancerous lesions of intrahepatic cholangiocarcinoma. J Hepatobiliary Pancreat Surg. 2000. 7:542–550.6. Nakanuma Y. A novel approach to biliary tract pathology based on similarities to pancreatic counterparts: is the biliary tract an incomplete pancreas? Pathol Int. 2010. 60:419–429.7. Kloek JJ, van der Gaag NA, Erdogan D, et al. A comparative study of intraductal papillary neoplasia of the biliary tract and pancreas. Hum Pathol. 2011. 42:824–832.8. Naito Y, Kusano H, Nakashima O, et al. Intraductal neoplasm of the intrahepatic bile duct: clinicopathological studyof 24 cases. World J Gastroenterol. 2012. 18:3673–3680.9. Lee SS, Kim MH, Lee SK, et al. Clinicopathologic review of 58 patients with biliary papillomatosis. Cancer. 2004. 100:783–793.10. Wu SD, Lu CD, Lu CJ, et al. Mucin-producing intrahepatic biliary papillomatosis. Surg Today. 2010. 40:845–850.11. Nakanuma Y, Zen Y, Harada K, et al. Tumorigenesis and phenotypic characteristics of mucin-producing bile duct tumors: an immunohistochemical approach. J Hepatobiliary Pancreat Sci. 2010. 17:211–222.12. Nakanishi Y, Zen Y, Hirano S, et al. Intraductal oncocytic papillary neoplasm of the bile duct: the first case of peribiliary gland origin. J Hepatobiliary Pancreat Surg. 2009. 16:869–873.13. Ohtsuka M, Kimura F, Shimizu H, et al. Similarities and differences between intraductal papillary tumors of the bile duct with and without macroscopically visible mucin secretion. Am J Surg Pathol. 2011. 35:512–521.14. Yang J, Wang W, Yan L. The clinicopathological features of intraductal papillary neoplasms of the bile duct in a Chinese population. Dig Liver Dis. 2012. 44:251–256.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Intrahepatic and extrahepatic intraductal papillary neoplasms of bile duct
- Photodynamic Therapy Followed by Left Hepatectomy Used to Treat an Intraductal Papillary Mucinous Neoplasm of the Bile Duct
- Characterization of Intraductal Papillary Neoplasm of the Bile Duct with Respect to the Histopathologic Similarities to Pancreatic Intraductal Papillary Mucinous Neoplasm
- Extrahepatic Bile Duct Duplication with Intraductal Papillary Neoplasm: A Case Report
- Radiological Spectrum of Intraductal Papillary Tumors of the Bile Ducts