Korean Circ J.
2007 Oct;37(10):483-488. 10.4070/kcj.2007.37.10.483.
Effect of Conventional Dose of Simvastatin on Plaque Regression and Vascular Remodeling in the Peristent Reference Segments of Normocholesterolemic Patients: A Serial Intravascular Ultrasound Assessment
- Affiliations
-
- 1The Heart Center of Chonnam National University Hospital, Chonnam National University Research Institute of Medical Sciences, Gwangju, Korea. myungho@chollian.net
- KMID: 2227049
- DOI: http://doi.org/10.4070/kcj.2007.37.10.483
Abstract
-
BACKGROUND AND OBJECTIVES: This study aimed to assess the effect of simvastatin therapy on plaque regression and vascular remodeling in peristent reference segments of normocholesterolemic patients by using serial intravascular ultrasound (IVUS) observation.
SUBJECTS AND METHODS
We retrospectively evaluated the poststenting and follow-up IVUS findings in 208 peristent (bare metal stent) reference segments of 108 normocholesterolemic patients (20 mg/day simvastatin group; n=62 vs. non-simvastatin group; n=46); 100 segments were proximal and 108 segments were distal to the stent. Quantitative volumetric IVUS analysis was performed for 5-mm vessel segments immediately proximal and distal to the stent.
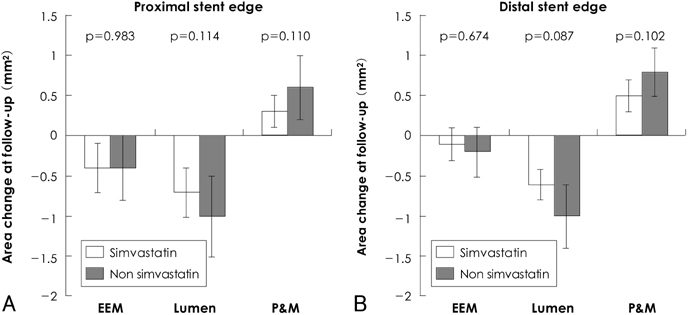
RESULTS
Follow-up IVUS was performed at a mean of 8.7 months after stenting (range: 3-19 months). For the proximal edge, a significant decrease in the mean lumen area and mean external elastic membrane (EEM) area and a significant increase in the mean plaque and media (P&M) area were observed at follow-up in both simvastatin and non-simvastatin groups. However, the changes in EEM (simvastatin: -0.4+/-0.3 mm2 vs. non-simvastatin: -0.4+/-0.4 mm2, p=0.983), lumen (simva-statin: -0.7+/-0.3 mm2 vs. non-simvastatin: -1.0+/-0.5 mm2, p=0.114), and P&M area (simvastatin: 0.3+/-0.2 mm2 vs. non-simvastatin: 0.6+/-0.4 mm2, p=0.110) from poststenting to follow-up at the proximal edge were not significantly different between the 2 groups. For the distal edge, a significant decrease in the mean lumen area and a significant increase in the mean P&M area were observed at follow-up in both the groups. However, the changes in the EEM area (simvastatin: -0.1+/-0.2 mm2 vs. non-simvastatin: -0.2+/-0.3 mm2, p=0.674), lumen area (simvastatin: -0.6+/-0.2 mm2 vs. non-simvastatin: -1.0+/-0.4 mm2, p=0.087), and P&M area (simvastatin: 0.5+/-0.2 mm2 vs. non-simvastatin: 0.8+/-0.3 mm2, p=0.102) from poststenting to follow-up at the distal edge were not significantly different between the groups.
CONCLUSION
A conventional dose of simvastatin does not inhibit plaque progression and lumen loss in the peristent reference segments of normocholesterolemic patients who have undergone bare-metal stent implantation.
MeSH Terms
Figure
Reference
-
1. Hoffmann R, Mintz GS, Popma JJ, et al. Chronic arterial responses to stent implantation: a serial intravascular ultrasound analysis of Palmaz-Schatz stents in native coronary arteries. J Am Coll Cardiol. 1996. 28:1134–1139.2. Hoffmann R, Mintz GS, Dussaillant GR, et al. Patterns and mechanisms of in-stent restenosis: a serial intravascular ultrasound study. Circulation. 1996. 94:1247–1254.3. Mudra H, Regar E, Klauss V, et al. Serial follow-up after optimized ultrasound-guided deployment of Palmaz-Schatz stents: in-stent neointimal proliferation without significant reference segment response. Circulation. 1997. 95:363–370.4. Weissman NJ, Wilensky RL, Tanguay JF, et al. Extent and distribution of in-stent intimal hyperplasia and edge effect in a non-radiation stent population. Am J Cardiol. 2001. 88:248–252.5. Jimenez-Quevedo P, Sabate M, Angiolillo DJ, et al. Vascular effects of sirolimus-eluting versus bare-metal stents in diabetic patients: three-dimensional ultrasound results of the Diabetes and Sirolimus-Eluting Stent (DIABETES) Trial. J Am Coll Cardiol. 2006. 47:2172–2179.6. Serruys PW, Degertekin M, Tanabe K, et al. Vascular responses at proximal and distal edges of paclitaxel-eluting stents: serial intravascular ultrasound analysis from the TAXUS II trial. Circulation. 2004. 109:627–633.7. Honda Y, Grube E, de La Fuente LM, Yock PG, Stertzer SH, Fitzgerald PJ. Novel drug-delivery stent: intravascular ultrasound observations from the first human experience with the QP2-eluting polymer stent system. Circulation. 2001. 104:380–383.8. Cannon CP, Braunwald E, McCabe CH, et al. Intensive versus moderate lipid lowering with statins after acute coronary syndromes. N Engl J Med. 2004. 350:1495–1504.9. Nissen SE, Tuzcu EM, Schoenhagen P, et al. Effect of intensive compared with moderate lipid-lowering therapy on progression of coronary atherosclerosis: a randomized controlled trial. JAMA. 2004. 291:1071–1080.10. Libby P, Aikawa M. Mechanisms of plaque stabilization with statins. Am J Cardiol. 2003. 91(4A):4B–8B.11. Corsini A, Raiteri M, Soma MR, Gabbiani G, Paoletti R. Simvastatin but not pravastatin has a direct inhibitory effect on rat and human myocyte proliferation. Clin Biochem. 1992. 25:399–400.12. Roberts WL, Moulton L, Law TC, et al. Evaluation of nine automated high-sensitivity C-reactive protein methods: implications for clinical and epidemiological applications: part 2. Clin Chem. 2001. 47:418–425.13. Walter DH, Schachinger V, Elsner M, Dimmeler S, Zeiher AM. Platelet glycoprotein IIIa polymorphisms and risk of coronary stent thrombosis. Lancet. 1997. 350:1217–1219.14. Strandberg TE, Vanhanen H, Tikkanen MJ. Effect of statins on C-reactive protein in patients with coronary artery disease. Lancet. 1999. 353:118–119.15. Ridker PM, Rifai N, Pfeffer MA, et al. Inflammation, pravastatin, and the risk of coronary events after myocardial infarction in patients with average cholesterol levels. Circulation. 1998. 98:839–844.16. Park SY, Kwak JJ, Park SH. Dose dependent changes of lipid profiles, IL-6 and CRP in unstable angina patients after simvastatin therapy. Korean Circ J. 2003. 33:663–670.17. Dupuis J, Tardif JC, Cernacek P, Theroux P. Cholesterol reduction rapidly improves endothelial function after acute coronary syndromes. Circulation. 1999. 99:3227–3233.18. Son JW, Koh KK. Effects of statins on endothelium: vasomotor eunction, inflammation, and hemostasis. Korean Circ J. 1999. 29:1016–1031.19. Lacoste L, Lam JY, Hung J, Letchacovski G, Solymoss CB, Waters D. Hyperlipidemia and coronary disease: correction of the increased thrombogenic potential with cholesterol reduction. Circulation. 1995. 92:3172–3177.20. The Scandinavian Simvastatin Survival Study Group. Randomised trial of cholesterol lowering in 4444 patients with coronary heart disease. Lancet. 1994. 344:1383–1389.21. Sacks FM, Pfeffer MA, Moye LA, et al. The effect of pravastatin on coronary events after myocardial infarction in patients with average cholesterol levels. N Engl J Med. 1996. 335:1001–1009.22. Hong YJ, Jeong MH, Lim JH, et al. The prognostic significance of statin therapy according to the level of C-reactive protein in acute myocardial infarction patients who underwent percutaneous coronary intervention. Korean Circ J. 2003. 33:891–900.23. Nakagawa T, Kobayashi T, Awata N, et al. Randomized, controlled trial of secondary prevention of coronary sclerosis in normocholesterolemic patients using pravastatin: final 5-year angiographic follow-up of the Prevention of Coronary Sclerosis (PCS) study. Int J Cardiol. 2004. 97:107–114.24. Tamura A, Mikuriya Y, Nasu M. Effect of pravastatin (10 mg/day) on progression of coronary atherosclerosis in patients with serum total cholesterol levels from 160 to 220 mg/dL and angiographically documented coronary artery disease. Am J Cardiol. 1997. 79:893–896.25. Suzuki M, Saito M, Nagai T, Saeki H, Kazatani Y. Prevention of positive coronary artery remodeling with statin therapy in patients with coronary artery diseases. Angiology. 2006. 57:259–265.26. Jensen LO, Thayssen P, Mintz GS, Carlier SG, Pedersen KE, Haghfelt T. Effect of simvastatin on coronary lesion site remodeling. Cardiology. 2006. 106:256–263.27. Petronio AS, Amoroso G, Limbruno U, et al. Simvastatin does not inhibit intimal hyperplasia and restenosis but promotes plaque regression in normocholesterolemic patients undergoing coronary stenting: a randomized study with intravascular ultrasound. Am Heart J. 2005. 149:520–526.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Usual Dose of Simvastatin Does Not Inhibit Plaque Progression and Lumen Loss at the Peri-Stent Reference Segments after Bare-Metal Stent Implantation: A Serial Intravascular Ultrasound Analysis
- Intravascular Ultrasonic Predictors of Intimal Hyperplasia after Coronary Stenting
- Intravascular Ultrasound Findings of Arterial Remodeling at the Sites of Focal Coronary Spasm in Patients with Vasospatic Angina
- Plaque Characteristics and Clinical Presentation Associated with Coronary Artery Remodeling: An Intravascular Ultrasound Study
- Lesion Characteristics in Patients with Acute Coronary Syndrome: A Comparison with Lesion in Patients with Stable Angina by Intravascular Ultrasound