Korean Circ J.
2010 Dec;40(12):639-644. 10.4070/kcj.2010.40.12.639.
Predicting Myocardial Functional Recovery After Acute Myocardial Infarction: Relationship Between Myocardial Strain and Coronary Flow Reserve
- Affiliations
-
- 1Division of Cardiology, Department of Internal Medicine, Korea University College of Medicine, Seoul, Korea. wjshimmd@unitel.co.kr
- KMID: 2225162
- DOI: http://doi.org/10.4070/kcj.2010.40.12.639
Abstract
- BACKGROUND AND OBJECTIVES
The purpose of this study was to evaluate the relationship between myocardial strain and coronary flow reserve (CFR) in the prediction of myocardial functional recovery after acute myocardial infarction (AMI).
SUBJECTS AND METHODS
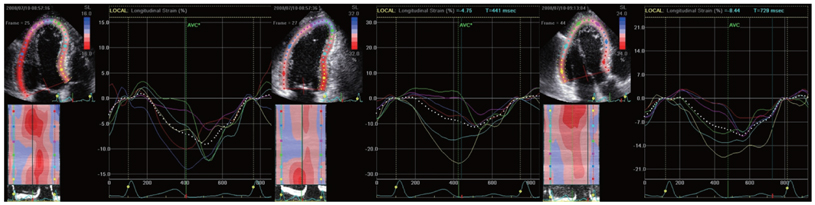
Consecutive patients with anterior ST elevation AMI were analyzed. Left ventricular (LV) strain, determined by 2-dimensional speckle tracking imaging and CFR, determined by intracoronary flow measurement, were obtained on the same day, 3-5 days after primary percutaneous coronary intervention. A-strain was defined as the mean systolic longitudinal strain of 11 LV segments (out of 18) assumed to be supplied by the left anterior descending coronary artery (LAD). Functional recovery was defined as improved wall motion >1 grade seen in at least 2 contiguous dysfunctional segments by echocardiography at the 6-month follow-up.
RESULTS
Of 20 patients, 8 patients had preserved CFR (>2.0) and 12 patients had impaired CFR (< or =2.0). There were no differences between the 2 CFR groups in LV ejection fractions and wall motion score indices in the LAD territory. However, A-strain was greater in patients with preserved CFR than in patients with impaired CFR (-6.4+/-2.0% vs. -4.6+/-1.4%, p=0.03). A-strain and CFR correlated well with each other (r=-0.49, p=0.03). Ten of 20 patients showed functional recovery at 6 months. Of clinical and echocardiographic parameters, A-strain was the only predictor of recovery (odds ratio 2.02, 95% confidence interval=1.03-3.97, p=0.04). For predicting recovery, the sensitivity and specificity were 80.0% and 80.0%, respectively, for CFR (cutoff=1.60), and 60.0% and 90.0%, respectively, for A-strain (cutoff=-6.13%).
CONCLUSION
Myocardial strain correlates well with the extent of microvascular integrity and can be used as a noninvasive method for predicting recovery after AMI.
Keyword
MeSH Terms
Figure
Cited by 2 articles
-
Usefulness of Myocardial Longitudinal Strain in Prediction of Heart Failure in Patients with Successfully Reperfused Anterior Wall ST-segment Elevation Myocardial Infarction
Sun Hwa Lee, Sang-Rok Lee, Kyoung-Suk Rhee, Jei-Keon Chae, Won-Ho Kim
Korean Circ J. 2019;49(10):960-972. doi: 10.4070/kcj.2018.0421.Coronary Flow Reserve in the Remote Myocardium Predicts Left Ventricular Remodeling Following Acute Myocardial Infarction
Rongchao Cheng, Guoqian Wei, Longhao Yu, Zhendong Su, Li Wei, Xiuping Bai, Jiawei Tian, Xueqi Li
Yonsei Med J. 2014;55(4):904-911. doi: 10.3349/ymj.2014.55.4.904.
Reference
-
1. Bates ER, Krell MJ, Dean EN, O'Neill WW, Vogel RA. Demonstration of the "no-reflow" phenomenon by digital coronary arteriography. Am J Cardiol. 1986. 57:177–178.2. Morishima I, Sone T, Mokuno S, et al. Clinical significance of no-reflow phenomenon observed on angiography after successful treatment of acute myocardial infarction with percutaneous transluminal coronary angioplasty. Am Heart J. 1995. 130:239–243.3. Ito H, Okamura A, Iwakura K, et al. Myocardial perfusion patterns related to thrombolysis in myocardial infarction perfusion grades after coronary angioplasty in patients with acute anterior wall myocardial infarction. Circulation. 1996. 93:1993–1999.4. Suryapranata H, Zijlstra F, MacLeod DC, van den Brand M, de Feyter PJ, Serruys PW. Predictive value of reactive hyperemic response on reperfusion on recovery of regional myocardial function after coronary angioplasty in acute myocardial infarction. Circulation. 1994. 89:1109–1117.5. Yoon MH, Tahk SJ, Choi SY, et al. Coronary flow reserve as a predictor of long-term clinical outcome after acute myocardial Infarction. Korean Circ J. 2002. 32:756–765.6. Cho KI, Park JH, Park JR, et al. Assessment of left ventricular function in symptomatic patients with myocardial bridge using two-dimensional strain. Korean Circ J. 2006. 36:617–625.7. Pirat B, Khoury DS, Hartley CJ, et al. A novel feature-tracking echocardiographic method for the quantitation of regional myocardial function: validation in an animal model of ischemia-reperfusion. J Am Coll Cardiol. 2008. 51:651–659.8. Park YH, Kang SJ, Song JK, et al. Prognostic value of longitudinal strain after primary reperfusion therapy in patients with anterior-wall acute myocardial infarction. J Am Soc Echocardiogr. 2008. 21:262–267.9. Vartdal T, Brunvand H, Pettersen E, et al. Early prediction of infarct size by strain Doppler echocardiography after coronary reperfusion. J Am Coll Cardiol. 2007. 49:1715–1721.10. Alpert JS, Thygesen K, Antman E, Bassand JP. Myocardial infarction redefined: a consensus document of The Joint European Society of Cardiology/American College of Cardiology Committee for the redefinition of myocardial infarction. J Am Coll Cardiol. 2000. 36:959–969.11. Schiller NB, Shah PM, Crawford M, et al. American Society of Echocardiography Committee on Standards, Subcommittee on Quantitation of Two-Dimensional Echocardiograms. Recommendations for quantitation of the left ventricle by two-dimensional echocardiography. J Am Soc Echocardiogr. 1989. 2:358–367.12. Doucette JW, Corl PD, Payne HM, et al. Validation of a Doppler guide wire for intravascular measurement of coronary artery flow velocity. Circulation. 1992. 85:1899–1911.13. Lim DS, Kim YH, Lee HS, et al. Coronary flow reserve is reflective of myocardial perfusion status in acute anterior myocardial infarction. Catheter Cardiovasc Interv. 2000. 51:281–286.14. Erdreich LS, Lee ET. Use of relative operating characteristic analysis in epidemiology: a method for dealing with subjective judgement. Am J Epidemiol. 1981. 114:649–662.15. Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986. 1:307–310.16. Irimpen AM, Tenaglia AN, Shin DJ, Buda AJ. Lack of ventricular remodeling in non-Q-wave myocardial infarction. Am Heart J. 1996. 131:466–471.17. Pfeffer MA, Braunwald E. Ventricular remodeling after myocardial infarction: experimental observations and clinical implications. Circulation. 1990. 81:1161–1172.18. St John Sutton M, Pfeffer MA, Plappert T, et al. Quantitative two-dimensional echocardiographic measurements are major predictors of adverse cardiovascular events after acute myocardial infarction: the protective effects of captopril. Circulation. 1994. 89:68–75.19. Perk G, Tunick PA, Kronzon I. Non-Doppler two-dimensional strain imaging by echocardiography: from technical considerations to clinical applications. J Am Soc Echocardiogr. 2007. 20:234–243.20. Chan J, Hanekom L, Wong C, Leano R, Cho GY, Marwick TH. Differentiation of subendocardial and transmural infarction using two-dimensional strain rate imaging to assess short-axis and long-axis myocardial function. J Am Coll Cardiol. 2006. 48:2026–2033.21. Sachdev V, Aletras AH, Padmanabhan S, et al. Myocardial strain decreases with increasing transmurality of infarction: a Doppler echocardiographic and magnetic resonance correlation study. J Am Soc Echocardiogr. 2006. 19:34–39.22. Becker M, Lenzen A, Ocklenburg C, et al. Myocardial deformation imaging based on ultrasonic pixel tracking to identify reversible myocardial dysfunction. J Am Coll Cardiol. 2008. 51:1473–1481.23. Wu KC, Kim RJ, Bluemke DA, et al. Quantification and time course of microvascular obstruction by contrast-enhanced echocardiography and magnetic resonance imaging following acute myocardial infarction and reperfusion. J Am Coll Cardiol. 1998. 32:1756–1764.24. Nijveldt R, Beek AM, Hofman MB, et al. Late gadolinium-enhanced cardiovascular magnetic resonance evaluation of infarct size and microvascular obstruction in optimally treated patients after acute myocardial infarction. J Cardiovasc Magn Reson. 2007. 9:765–770.25. Lim DS, Kim YH, Lee HS, et al. Relation between perfusion status of dysfunctional myocardium and coronary flow reserve in acute myocardial infarction. Korean Circ J. 1998. 28:164–172.26. Rochitte CE, Lima JA, Bluemke DA, et al. Magnitude and time course of microvascular obstruction and tissue injury after acute myocardial infarction. Circulation. 1998. 98:1006–1014.27. Gerber BL, Rochitte CE, Melin JA, et al. Microvascular obstruction and left ventricular remodeling early after acute myocardial infarction. Circulation. 2000. 101:2734–2741.28. Rosen BD, Lima JA, Nasir K, et al. Lower myocardial perfusion reserve is associated with decreased regional left ventricular function in asymptomatic participants of the multi-ethnic study of atherosclerosis. Circulation. 2006. 114:289–297.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Myocardial fractional flow reserve in acute myocardial infarction
- Coronary Slow Flow Phenomenon Leads to ST Elevation Myocardial Infarction
- Assessment of Myocardial Viability Using PET
- A Case of Non-Q Myocardial Infaction in a Patient with Myocardial Bridging
- Myocardial Contrast Echocardiography for the Assessment of Coronary Blood Flow Reserve