Korean Circ J.
2011 Jan;41(1):38-42. 10.4070/kcj.2011.41.1.38.
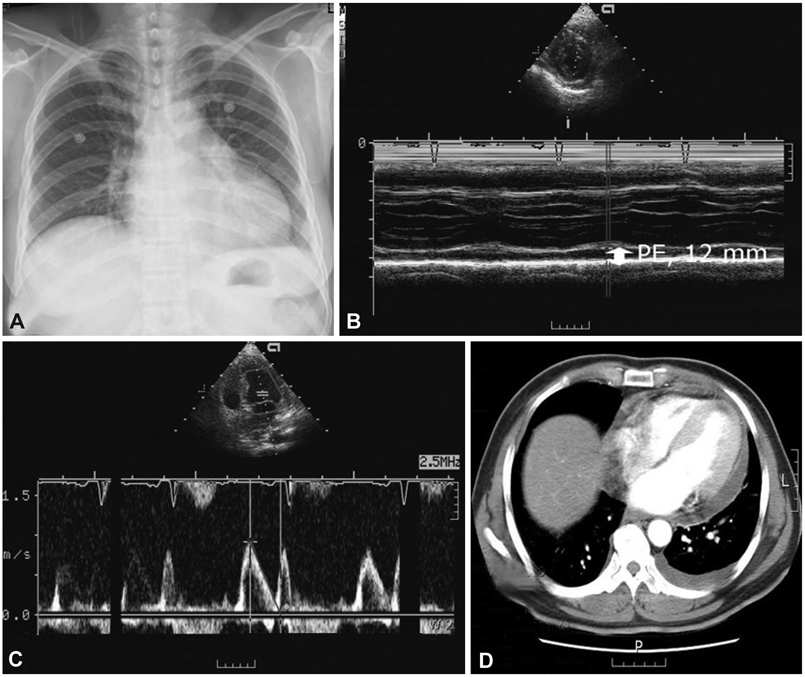
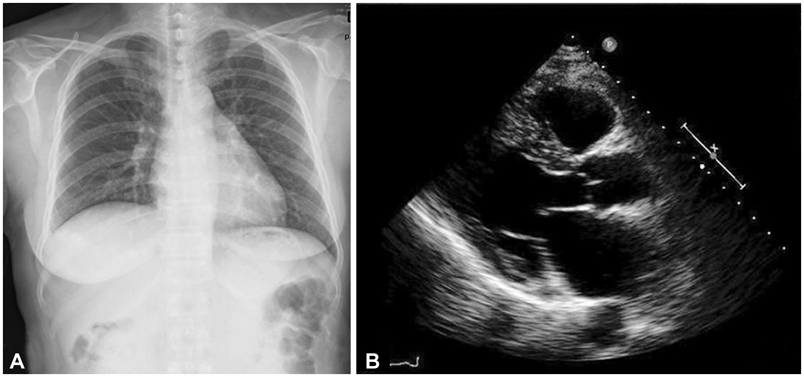
A Case of Sparganosis That Presented as a Recurrent Pericardial Effusion
- Affiliations
-
- 1Department of Internal Medicine, Chungbuk National University School of Medicine, Cheongju, Korea. drcorazon@hanmail.net
- 2Department of Laboratory Medicine, Chungbuk National University School of Medicine, Cheongju, Korea.
- KMID: 2225153
- DOI: http://doi.org/10.4070/kcj.2011.41.1.38
Abstract
- Sparganosis is caused by a larval tapeworm of the genus Spirometra, which commonly invades subcutaneous tissue, but less frequently invades muscle, intestines, spinal cord, and the peritoneopleural cavity. The authors managed a female patient who presented with a recurrent pericardiopleural effusion and peripheral eosinophilia. The anti-sparganum-specific IgG serum level was significantly higher than normal control levels. In this patient, sparganosis was caused by the ingestion of raw frogs in an effort to control her thyroid disease. The recurrent pericardiopleural effusion and peripheral eosinophilia were controlled by 3 consecutive doses of praziquantel (75 mg/kg/day). The patient is doing well 4 years after presentation. Sparganosis should be considered a rare, but possible cause of recurrent pericardial effusion and peripheral eosinophilia. Immunoserologic testing using enzyme linked immunosorbent assays can be helpful in diagnosing human sparganosis, especially in cases without a subcutaneous lump or mass. Praziquantel is an alternative treatment for sparganosis in surgically-unresectable cases.
Keyword
MeSH Terms
Figure
Cited by 2 articles
-
Praziquantel Treatment in Trematode and Cestode Infections: An Update
Jong-Yil Chai
Infect Chemother. 2013;45(1):32-43. doi: 10.3947/ic.2013.45.1.32.Human Sparganosis in Korea
Jeong-Geun Kim, Chun-Seob Ahn, Woon-Mok Sohn, Yukifumi Nawa, Yoon Kong
J Korean Med Sci. 2018;33(44):. doi: 10.3346/jkms.2018.33.e273.
Reference
-
1. Sun T. Parasitic Disorders: Pathology, Diagnosis, and Management. 1999. 2nd ed. Pennsylvania: Williams & Wilkins;285–290.2. Mueller JF. The biology of Spirometra. J Parasitol. 1974. 60:3–14.3. Cho SY, Bae JH, Seo BS. Some aspects of human sparganosis in Korea. Korean J Parasitol. 1975. 13:60–77.4. Tanaka S, Maruyama H, Ishiwata K, et al. A case report of pleural sparganosis. Parasitol Int. 1997. 46:73–75.5. Ishii H, Mukae H, Inoue Y, et al. A rare case of eosinophilic pleuritis due to sparganosis. Intern Med. 2001. 40:783–785.6. Kamiya H, Shimizu H, Kobayashi N, Kudo K. A case of sparganosis with eosinophilic pleural effusion. Nihon Kokyuki Gakkai Zasshi. 2004. 42:1019–1023.7. Shimada M, Matsumura K, Aoki Y, et al. Two cases of sparganosis having onsets of pleural effusion. Jpn J Parasitol. 1989. 38:145.8. Yamasaki H, Araki K, Aoki T. Parasitic diseases examined during the past 16 years in the Department of Parasitology, Juntendo University School of Medicine. Juntendo Igaku. 1994. 40:262–279.9. Kim DH, Yi IH, Youn HC, et al. Pleural sparganosis: a case report. Korean J Thorac Cardiovasc Surg. 2006. 39:502–504.10. Koh TW, Lee JW, Sohn DS, et al. Empyema thoracis associated with sparganosis: a case report. Korean J Thorac Cardiovasc Surg. 1988. 21:761–765.11. Ha JK, Hong TJ, Chun KJ, et al. Biochemical analysis of serum and pericardial fluid in patients with hemorrhagic pericardial effusion. Korean Circ J. 2003. 33:227–232.12. Eo WK, Lee SK, Choi CJ, et al. Clinical studies on the etiology and clinical course of pericardial effusions. Korean Circ J. 1990. 20:211–219.13. Voller A, Bidwell DE, Bartlett A. The Enzyme-Linked Immunosorbent Assay. 1994. London: Nuffield laboratories of comparative medicine;19–41.14. Min DY. Cestode infections in Korea. Korean J Parasitol. 1990. 28:123–144.15. Sim S, You JK, Lee IY, Im KI, Yong TS. A case of breast sparganosis. Korean J Parasitol. 2002. 40:187–189.16. Kim HJ, Park SH, Yum DJ, et al. A case of sparganosis in the submandibular triangle. J Clin Otolaryngol Head Neck Surg. 2005. 16:330–333.17. Cho KJ, Lee HS, Chi JG. Intramural sparganosis manifested as intestinal obstruction. J Korean Med Sci. 1987. 2:137–139.18. Kim H, Kim SI, Cho SY. Serological diagnosis of human sparganosis by means of micro-ELISA. Korean J Parasitol. 1984. 22:222–228.19. Yeo IS, Yong TS, Im K. Serodiagnosis of human sparganosis by a monoclonal antibody-based competition ELISA. Yonsei Med J. 1994. 35:43–48.20. Sohn WM, Hong ST, Chai JY, Lee SH. Infectivity of the sparganum treated by praziquantel, gamma-irradiation and mechanical cutting. Korean J Parasitol. 1993. 31:135–139.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A case of massive pericardial effusion caused by acute recurrent pancreatitis with complication
- A Case of POEMS Syndrome that Presented with a Moderate Pericardial Effusion
- Large Hypothyroidism-Induced Pericardial Effusion with Increased Serum Tumor Markers
- Two Cases of Primary HypoThyroidism Presenting with Pericardial Effusion
- Primary Intrapericardial Lipoma Simulating Pericardial Effusion -Report of A Case-