Korean Circ J.
2013 Dec;43(12):825-829. 10.4070/kcj.2013.43.12.825.
QTc Prolongation after Ventricular Septal Defect Repair in Infants
- Affiliations
-
- 1Division of Pediatric Cardiology, Department of Pediatrics, Congenital Heart Disease Center, Severance Cardiovascular Hospital, Yonsei University College of Medicine, Seoul, Korea. pednk@yuhs.ac
- 2Division of Cardiovascular Surgery, Congenital Heart Disease Center, Severance Cardiovascular Hospital, Yonsei University College of Medicine, Seoul, Korea.
- KMID: 2224777
- DOI: http://doi.org/10.4070/kcj.2013.43.12.825
Abstract
- BACKGROUND AND OBJECTIVES
Prolonging of the corrected QT interval (QTc) has been reported after cardiac surgery in some studies. However, there have not been many studies on infant open cardiac surgery for ventricular septal defect (VSD) repair. This study was performed to define the changes in QTc and to find related post-surgery factors in this patient group.
SUBJECTS AND METHODS
From 2008 to 2012, 154 infants underwent VSD repair at the Severance Cardiovascular Hospital. This study includes 105 of these cases. QTc was measured in these patients retrospectively. Demographic data and peri-procedural data, such as Aristotle score, cross-clamp time and bypass time, were analyzed. The exclusion criteria included multiple and small VSDs that underwent direct closure.
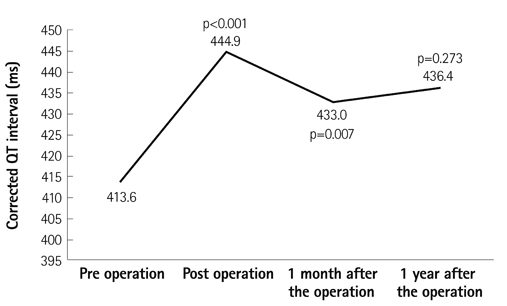
RESULTS
Mean post-operative QTc was increased compared to the pre-operative measurements (from 413.6+/-2.3 to 444.9+/-2.5, p<0.001). In multiple linear regression, the comprehensive Aristotle score was associated with increasing QTc (p=0.047). The incidence of transient arrhythmia, such as atrial tachycardia, junctional ectopic tachycardia, premature atrial contraction, or premature ventricular contraction, was associated with QTc prolongation (p=0.005). Prolonged QTc was also associated with cross-clamp time (p=0.008) and low weight (p=0.042). Total length of stay at the intensive care unit and intubation time after surgery were not associated with QTc prolongation.
CONCLUSION
Prolonged QTc could be seen after VSD repair in infants. This phenomenon was associated with peri-procedural factors such as the Aristotle score and cross-clamp time. Patients with QTc prolongation after cardiac surgery had an increased tendency towards arrhythmogenicity in the post-operative period.
MeSH Terms
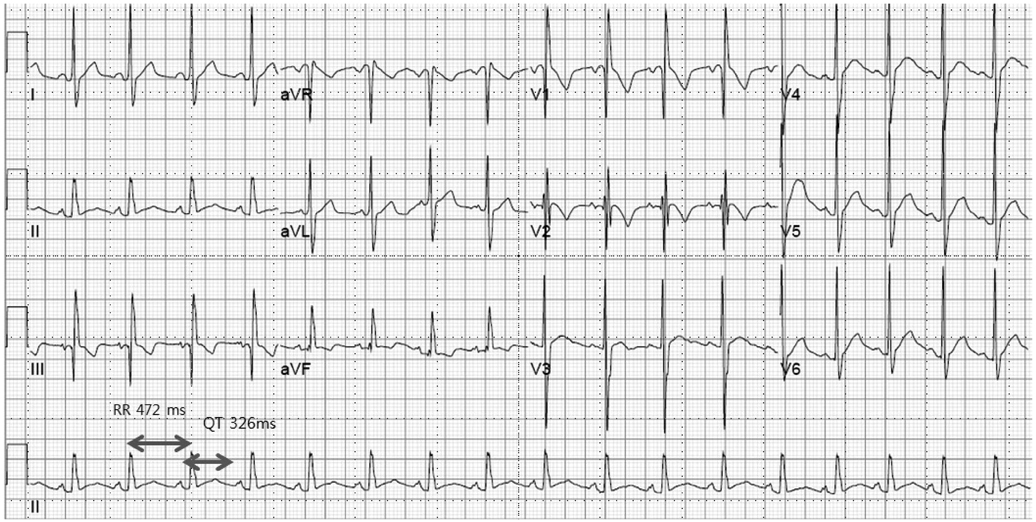
Figure
Reference
-
1. Kim YH, Choi HJ, Kim GJ, Cho JY, Hyun MC, Lee SB. The changes in signal-averaged electrocardiogram after surgical correction of congenital heart disease. Korean J Pediatr. 2009; 52:1364–1369.2. Creswell LL, Schuessler RB, Rosenbloom M, Cox JL. Hazards of postoperative atrial arrhythmias. Ann Thorac Surg. 1993; 56:539–549.3. Ascione R, Lloyd CT, Underwood MJ, Lotto AA, Pitsis AA, Angelini GD. Inflammatory response after coronary revascularization with or without cardiopulmonary bypass. Ann Thorac Surg. 2000; 69:1198–1204.4. Vetter VL, Horowitz LN. Electrophysiologic residua and sequelae of surgery for congenital heart defects. Am J Cardiol. 1982; 50:588–604.5. Delaney JW, Moltedo JM, Dziura JD, Kopf GS, Snyder CS. Early postoperative arrhythmias after pediatric cardiac surgery. J Thorac Cardiovasc Surg. 2006; 131:1296–1300.6. Rekawek J, Kansy A, Miszczak-Knecht M, et al. Risk factors for cardiac arrhythmias in children with congenital heart disease after surgical intervention in the early postoperative period. J Thorac Cardiovasc Surg. 2007; 133:900–904.7. Punn R, Lamberti JJ, Balise RR, Seslar SP. QTc prolongation in children following congenital cardiac disease surgery. Cardiol Young. 2011; 21:400–410.8. MacLeod RS, Shome S, Stinstra J, Punske BB, Hopenfeld B. Mechanisms of ischemia-induced ST-segment changes. J Electrocardiol. 2005; 38:4 Suppl. 8–13.9. Bae MH, Cheon SS, Song JH, et al. Etiologies and predictors of ST-segment elevation myocardial infarction. Korean Circ J. 2013; 43:370–376.10. Jain U, Wallis DE, Moran JF. Significance of electrocardiographic ST elevation during coronary artery bypass surgery. Anesth Analg. 1994; 78:638–643.11. Ali N, Rizwi F, Iqbal A, Rashid A. Induced remote ischemic pre-conditioning on ischemia-reperfusion injury in patients undergoing coronary artery bypass. J Coll Physicians Surg Pak. 2010; 20:427–431.12. Kenigsberg DN, Khanal S, Kowalski M, Krishnan SC. Prolongation of the QTc interval is seen uniformly during early transmural ischemia. J Am Coll Cardiol. 2007; 49:1299–1305.13. Vrtovec B, Ryazdanbakhsh AP, Pintar T, Collard CD, Gregoric ID, Radovancevic B. QTc interval prolongation predicts postoperative mortality in heart failure patients undergoing surgical revascularization. Tex Heart Inst J. 2006; 33:3–8.14. Aburawi EH, Souid AK, Liuba P, Zoubeidi T, Pesonen E. Early changes in myocardial repolarization and coronary perfusion after cardiopulmonary bypass surgery for ASD repair in children. BMC Cardiovasc Disord. 2013; 13:67.15. Elming H, Brendorp B, Køber L, Sahebzadah N, Torp-Petersen C. QTc interval in the assessment of cardiac risk. Card Electrophysiol Rev. 2002; 6:289–294.16. Trinkley KE, Lee Page R 2nd, Lien H, Yamanouye K, Tisdale JE. QT interval prolongation and the risk of torsades de pointes: essentials for clinicians. Curr Med Res Opin. 2013; [Epub ahead of print].17. Nagele P, Pal S, Brown F, Blood J, Miller JP, Johnston J. Postoperative QT interval prolongation in patients undergoing noncardiac surgery under general anesthesia. Anesthesiology. 2012; 117:321–328.18. Roden DM. Drug-induced prolongation of the QT interval. N Engl J Med. 2004; 350:1013–1022.19. Reingardiene D, Vilcinskaite J. [QTc-prolonging drugs and the risk of sudden death]. Medicina (Kaunas). 2007; 43:347–353.20. Manrique AM, Arroyo M, Lin Y, et al. Magnesium supplementation during cardiopulmonary bypass to prevent junctional ectopic tachycardia after pediatric cardiac surgery: a randomized controlled study. J Thorac Cardiovasc Surg. 2010; 139:162–169.21. Davey P. How to correct the QT interval for the effects of heart rate in clinical studies. J Pharmacol Toxicol Methods. 2002; 48:3–9.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Reoperation of Postinfarction VSD
- The muscular ventricular septal defect and multiple ventricular septal defects in some congenital heart diseases
- A Case of Traumatic Ventricular Septal Defect Secondary to Nonpenetrating Chest Trauma
- Clinical Correlates of QTc Prolongation in Patients with Schizophrenia : A Retrospective Study
- Repair of Postinfarction Ventricular Septal Defect on a Beating Heart: One case report