Korean Circ J.
2015 Jan;45(1):1-8. 10.4070/kcj.2015.45.1.1.
Pediatric Heart Failure: Current State and Future Possibilities
- Affiliations
-
- 1The Cardiac Center, The Children's Hospital of Philadelphia, Department of Pediatrics, Perelman School of Medicine at the University of Pennsylvania, Philadelphia, PA, USA. rossanoj@email.chop.edu
- 2Department of Pediatrics, Korea University Hospital, Ansan, Korea.
- KMID: 2223839
- DOI: http://doi.org/10.4070/kcj.2015.45.1.1
Abstract
- Heart failure is a complex pathophysiological syndrome that can occur in children from a variety of diseases, including cardiomyopathies, myocarditis, and congenital heart disease. The condition is associated with a high rate of morbidity and mortality and places a significant burden on families of affected children and to society as a whole. Current medical therapy is taken largely from the management of heart failure in adults, though clear survival benefit of these medications are lacking. Ventricular assist devices (VADs) have taken an increasingly important role in the management of advanced heart failure in children. The predominant role of these devices has been as a bridge to heart transplantation, and excellent results are currently achieved for most children with cardiomyopathies. There is an ongoing investigation to improve outcomes in high-risk populations, such as small infants and those with complex congenital heart disease, including patients with functionally univentricular hearts. Additionally, there is an active investigation and interest in expansion of VADs beyond the predominant utilization as a bridge to a heart transplant into ventricular recovery, device explant without a heart transplantation (bridge to recovery), and placement of devices without the expectation of recovery or transplantation (destination therapy).
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Pediatric Ventricular Assist Device
Yu Rim Shin, Young-Hwan Park, Han Ki Park
Korean Circ J. 2019;49(8):678-690. doi: 10.4070/kcj.2019.0163.
Reference
-
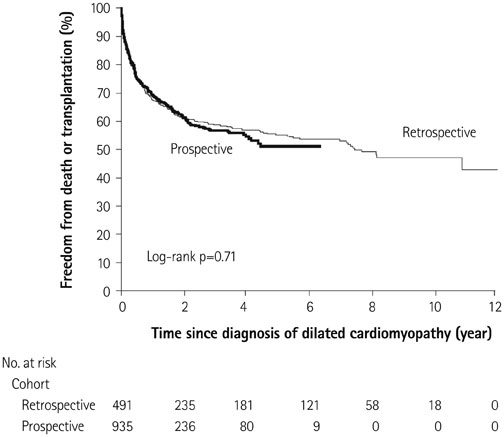
1. Kirk R, Dipchand AI, Rosenthal DN, et al. The International Society of Heart and Lung Transplantation Guidelines for the management of pediatric heart failure: executive summary. J Heart Lung Transplant. 2014; 33:888–909.2. Choi DJ, Han S, Jeon ES, et al. Characteristics, outcomes and predictors of long-term mortality for patients hospitalized for acute heart failure: a report from the Korean heart failure registry. Korean Circ J. 2011; 41:363–371.3. Go AS, Mozaffarian D, Roger VL, et al. Heart disease and stroke statistics--2014 update: a report from the American Heart Association. Circulation. 2014; 129:e28–292.4. Roger VL, Weston SA, Redfield MM, et al. Trends in heart failure incidence and survival in a community-based population. JAMA. 2004; 292:344–350.5. Heidenreich PA, Albert NM, Allen LA, et al. Forecasting the impact of heart failure in the United States: a policy statement from the American Heart Association. Circ Heart Fail. 2013; 6:606–619.6. Tavazzi L, Senni M, Metra M, et al. Multicenter prospective observational study on acute and chronic heart failure: one-year follow-up results of IN-HF (Italian Network on Heart Failure) outcome registry. Circ Heart Fail. 2013; 6:473–481.7. Shiba N, Shimokawa H. Chronic heart failure in Japan: implications of the CHART studies. Vasc Health Risk Manag. 2008; 4:103–113.8. McMurray JJ, Stewart S. Epidemiology, aetiology, and prognosis of heart failure. Heart. 2000; 83:596–602.9. Massin MM, Astadicko I, Dessy H. Epidemiology of heart failure in a tertiary pediatric center. Clin Cardiol. 2008; 31:388–391.10. Rossano JW, Kim JJ, Decker JA, et al. Prevalence, morbidity, and mortality of heart failure-related hospitalizations in children in the United States: a population-based study. J Card Fail. 2012; 18:459–470.11. Hartman ME, Linde-Zwirble WT, Angus DC, Watson RS. Trends in the epidemiology of pediatric severe sepsis*. Pediatr Crit Care Med. 2013; 14:686–693.12. Nandi D, Lin KY, O'Connor MJ, et al. Hospital charges for pediatric heart failure related hospitalization in the United States from 200-2009. J Am Coll Cardiol. 2014; 33:S84. Abstract.13. Lipshultz SE, Sleeper LA, Towbin JA, et al. The incidence of pediatric cardiomyopathy in two regions of the United States. N Engl J Med. 2003; 348:1647–1655.14. Nugent AW, Daubeney PE, Chondros P, et al. The epidemiology of childhood cardiomyopathy in Australia. N Engl J Med. 2003; 348:1639–1646.15. Andrews RE, Fenton MJ, Ridout DA, Burch M;. New-onset heart failure due to heart muscle disease in childhood: a prospective study in the United Kingdom and Ireland. Circulation. 2008; 117:79–84.16. Daubeney PE, Nugent AW, Chondros P, et al. Clinical features and outcomes of childhood dilated cardiomyopathy: results from a national population-based study. Circulation. 2006; 114:2671–2678.17. Towbin JA, Lowe AM, Colan SD, et al. Incidence, causes, and outcomes of dilated cardiomyopathy in children. JAMA. 2006; 296:1867–1876.18. Kantor PF, Abraham JR, Dipchand AI, Benson LN, Redington AN. The impact of changing medical therapy on transplantation-free survival in pediatric dilated cardiomyopathy. J Am Coll Cardiol. 2010; 55:1377–1384.19. Alexander PM, Daubeney PE, Nugent AW, et al. Long-term outcomes of dilated cardiomyopathy diagnosed during childhood: results from a national population-based study of childhood cardiomyopathy. Circulation. 2013; 128:2039–2046.20. O'Sullivan JJ, Roche SL, Crossland DS, Chaudhari MP, Kirk RC, Asif H. Recovery of heart function in children with acute severe heart failure. Transplantation. 2008; 85:975–979.21. Everitt MD, Sleeper LA, Lu M, et al. Recovery of echocardiographic function in children with idiopathic dilated cardiomyopathy: results from the pediatric cardiomyopathy registry. J Am Coll Cardiol. 2014; 63:1405–1413.22. Macicek SM, Macias CG, Jefferies JL, Kim JJ, Price JF. Acute heart failure syndromes in the pediatric emergency department. Pediatrics. 2009; 124:e898–e904.23. Wong DT, George K, Wilson J, et al. Effectiveness of serial increases in amino-terminal pro-B-type natriuretic peptide levels to indicate the need for mechanical circulatory support in children with acute decompensated heart failure. Am J Cardiol. 2011; 107:573–578.24. Price JF, Thomas AK, Grenier M, et al. B-type natriuretic peptide predicts adverse cardiovascular events in pediatric outpatients with chronic left ventricular systolic dysfunction. Circulation. 2006; 114:1063–1069.25. Gulati A, Jabbour A, Ismail TF, et al. Association of fibrosis with mortality and sudden cardiac death in patients with nonischemic dilated cardiomyopathy. JAMA. 2013; 309:896–908.26. Dass S, Suttie JJ, Piechnik SK, et al. Myocardial tissue characterization using magnetic resonance noncontrast t1 mapping in hypertrophic and dilated cardiomyopathy. Circ Cardiovasc Imaging. 2012; 5:726–733.27. Hershberger RE, Lindenfeld J, Mestroni L, et al. Genetic evaluation of cardiomyopathy--a Heart Failure Society of America practice guideline. J Card Fail. 2009; 15:83–97.28. Effect of enalapril on survival in patients with reduced left ventricular ejection fractions and congestive heart failure. The SOLVD Investigators. N Engl J Med. 1991; 325:293–302.29. Packer M, Coats AJ, Fowler MB, et al. Effect of carvedilol on survival in severe chronic heart failure. N Engl J Med. 2001; 344:1651–1658.30. Pitt B, Poole-Wilson PA, Segal R, et al. Effect of losartan compared with captopril on mortality in patients with symptomatic heart failure: randomised trial--the Losartan Heart Failure Survival Study ELITE II. Lancet. 2000; 355:1582–1587.31. Pitt B, Zannad F, Remme WJ, et al. The effect of spironolactone on morbidity and mortality in patients with severe heart failure. Randomized Aldactone Evaluation Study Investigators. N Engl J Med. 1999; 341:709–717.32. Poole-Wilson PA, Swedberg K, Cleland JG, et al. Comparison of carvedilol and metoprolol on clinical outcomes in patients with chronic heart failure in the Carvedilol Or Metoprolol European Trial (COMET): randomised controlled trial. Lancet. 2003; 362:7–13.33. Hsu DT, Zak V, Mahony L, et al. Enalapril in infants with single ventricle: results of a multicenter randomized trial. Circulation. 2010; 122:333–340.34. Shaddy RE, Boucek MM, Hsu DT, et al. Carvedilol for children and adolescents with heart failure: a randomized controlled trial. JAMA. 2007; 298:1171–1179.35. Dore A, Houde C, Chan KL, et al. Angiotensin receptor blockade and exercise capacity in adults with systemic right ventricles: a multicenter, randomized, placebo-controlled clinical trial. Circulation. 2005; 112:2411–2416.36. Hechter SJ, Fredriksen PM, Liu P, et al. Angiotensin-converting enzyme inhibitors in adults after the Mustard procedure. Am J Cardiol. 2001; 87:660–663. A11.37. van der Bom T, Winter MM, Bouma BJ, et al. Effect of valsartan on systemic right ventricular function: a double-blind, randomized, placebo-controlled pilot trial. Circulation. 2013; 127:322–330.38. Rossano JW, Shaddy RE. Update on pharmacological heart failure therapies in children: do adult medications work in children and if not, why not? Circulation. 2014; 129:607–612.39. Stauffer BL, Russell G, Nunley K, Miyamoto SD, Sucharov CC. miRNA expression in pediatric failing human heart. J Mol Cell Cardiol. 2013; 57:43–46.40. Miyamoto SD, Stauffer BL, Nakano S, et al. Beta-adrenergic adaptation in paediatric idiopathic dilated cardiomyopathy. Eur Heart J. 2014; 35:33–41.41. Bernstein D, Fajardo G, Zhao M. The role of β-adrenergic receptors in heart failure: differential regulation of cardiotoxicity and cardioprotection. Prog Pediatr Cardiol. 2011; 31:35–38.42. Reddy S, Zhao M, Hu DQ, et al. Dynamic microRNA expression during the transition from right ventricular hypertrophy to failure. Physiol Genomics. 2012; 44:562–575.43. Albers S, Meibohm B, Mir TS, Läer S. Population pharmacokinetics and dose simulation of carvedilol in paediatric patients with congestive heart failure. Br J Clin Pharmacol. 2008; 65:511–522.44. Kwon HW, Kwon BS, Kim GB, et al. The effect of enalapril and carvedilol on left ventricular dysfunction in middle childhood and adolescent patients with muscular dystrophy. Korean Circ J. 2012; 42:184–191.45. Jefferies JL, Eidem BW, Belmont JW, et al. Genetic predictors and remodeling of dilated cardiomyopathy in muscular dystrophy. Circulation. 2005; 112:2799–2804.46. Duboc D, Meune C, Pierre B, et al. Perindopril preventive treatment on mortality in Duchenne muscular dystrophy: 10 years' follow-up. Am Heart J. 2007; 154:596–602.47. Viollet L, Thrush PT, Flanigan KM, Mendell JR, Allen HD. Effects of angiotensin-converting enzyme inhibitors and/or beta blockers on the cardiomyopathy in Duchenne muscular dystrophy. Am J Cardiol. 2012; 110:98–102.48. Duboc D, Meune C, Lerebours G, Devaux JY, Vaksmann G, Bécane HM. Effect of perindopril on the onset and progression of left ventricular dysfunction in Duchenne muscular dystrophy. J Am Coll Cardiol. 2005; 45:855–857.49. Kantor PF, Lougheed J, Dancea A, et al. Presentation, diagnosis, and medical management of heart failure in children: Canadian Cardiovascular Society guidelines. Can J Cardiol. 2013; 29:1535–1552.50. Packer M, Carver JR, Rodeheffer RJ, et al. Effect of oral milrinone on mortality in severe chronic heart failure. The PROMISE Study Research Group. N Engl J Med. 1991; 325:1468–1475.51. Abraham WT, Adams KF, Fonarow GC, et al. In-hospital mortality in patients with acute decompensated heart failure requiring intravenous vasoactive medications: an analysis from the Acute Decompensated Heart Failure National Registry (ADHERE). J Am Coll Cardiol. 2005; 46:57–64.52. Price JF, Mott AR, Dickerson HA, et al. Worsening renal function in children hospitalized with decompensated heart failure: evidence for a pediatric cardiorenal syndrome? Pediatr Crit Care Med. 2008; 9:279–284.53. Cuffe MS, Califf RM, Adams KF Jr, et al. Short-term intravenous milrinone for acute exacerbation of chronic heart failure: a randomized controlled trial. JAMA. 2002; 287:1541–1547.54. Shamszad P, Hall M, Rossano JW, et al. Characteristics and outcomes of heart failure-related intensive care unit admissions in children with cardiomyopathy. J Card Fail. 2013; 19:672–677.55. Wittlieb-Weber CA, Lin KY, Zaoutis TE, et al. Pediatric versus adult cardiomyopathy and heart failure related hospitlaizations: a valuebased analysis. Circulation. 2014; 128:A11498. Abstract.56. Morales DL, Almond CS, Jaquiss RD, et al. Bridging children of all sizes to cardiac transplantation: the initial multicenter North American experience with the Berlin Heart EXCOR ventricular assist device. J Heart Lung Transplant. 2011; 30:1–8.57. Rossano JW, Mott AR, Mohamad Z, et al. Decreasing mortality of ventricular assist devices at children's hospitals from 2000-2010: improvement at a cost (abstract). Circulation. 2012; 126:A11553.58. Almond CS, Thiagarajan RR, Piercey GE, et al. Waiting list mortality among children listed for heart transplantation in the United States. Circulation. 2009; 119:717–727.59. Benden C, Edwards LB, Kucheryavaya AY, et al. The Registry of the International Society for Heart and Lung Transplantation: Sixteenth Official Pediatric Lung and Heart-Lung Transplantation Report--2013; focus theme: age. J Heart Lung Transplant. 2013; 32:989–997.60. Hetzer R, Alexi-Meskishvili V, Weng Y, et al. Mechanical cardiac support in the young with the Berlin Heart EXCOR pulsatile ventricular assist device: 15 years' experience. Semin Thorac Cardiovasc Surg Pediatr Card Surg Annu. 2006; 99–108.61. Imamura M, Dossey AM, Prodhan P, et al. Bridge to cardiac transplant in children: Berlin Heart versus extracorporeal membrane oxygenation. Ann Thorac Surg. 2009; 87:1894–1901. discussion 1901.62. Fraser CD Jr, Jaquiss RD, Rosenthal DN, et al. Prospective trial of a pediatric ventricular assist device. N Engl J Med. 2012; 367:532–541.63. Kirklin JK, Naftel DC, Kormos RL, et al. Fifth INTERMACS annual report: risk factor analysis from more than 6,000 mechanical circulatory support patients. J Heart Lung Transplant. 2013; 32:141–156.64. Cabrera AG, Sundareswaran KS, Samayoa AX, et al. Outcomes of pediatric patients supported by the HeartMate II left ventricular assist device in the United States. J Heart Lung Transplant. 2013; 32:1107–1113.65. Miera O, Potapov EV, Redlin M, et al. First experiences with the Heart-Ware ventricular assist system in children. Ann Thorac Surg. 2011; 91:1256–1260.66. Padalino MA, Bottio T, Tarzia V, et al. HeartWare ventricular assist device as bridge to transplant in children and adolescents. Artif Organs. 2014; 38:418–422.67. Baldwin JT, Borovetz HS, Duncan BW, Gartner MJ, Jarvik RK, Weiss WJ. The national heart, lung, and blood institute pediatric circulatory support program: a summary of the 5-year experience. Circulation. 2011; 123:1233–1240.68. Rossano JW, Goldberg DJ, Fuller S, Ravishankar C, Montenegro LM, Gaynor JW. Successful use of the total artificial heart in the failing Fontan circulation. Ann Thorac Surg. 2014; 97:1438–1440.69. VanderPluym CJ, Rebeyka IM, Ross DB, Buchholz H. The use of ventricular assist devices in pediatric patients with univentricular hearts. J Thorac Cardiovasc Surg. 2011; 141:588–590.70. Rossano JW, Lin KY, Paridon SM, et al. Pediatric heart transplantation from donors with depressed ventricular function: an analysis of the United Network of Organ Sharing Database. Circ Heart Fail. 2013; 6:1223–1229.71. Cha MJ, Lee HY, Cho HJ, Hwang HY, Kim KB, Oh BH. Under-utilization of donor hearts in the initial era of the heart transplant program in Korea- review of 13 years' experience from the Korea national registry. Circ J. 2013; 77:2056–2063.72. Rose EA, Gelijns AC, Moskowitz AJ, et al. Long-term use of a left ventricular assist device for end-stage heart failure. N Engl J Med. 2001; 345:1435–1443.73. Amodeo A, Adorisio R. Left ventricular assist device in Duchenne cardiomyopathy: can we change the natural history of cardiac disease. Int J Cardiol. 2012; 161:e43.74. Birks EJ, Tansley PD, Hardy J, et al. Left ventricular assist device and drug therapy for the reversal of heart failure. N Engl J Med. 2006; 355:1873–1884.75. Drakos SG, Kfoury AG, Stehlik J, et al. Bridge to recovery: understanding the disconnect between clinical and biological outcomes. Circulation. 2012; 126:230–241.76. Vatta M, Stetson SJ, Jimenez S, et al. Molecular normalization of dystrophin in the failing left and right ventricle of patients treated with either pulsatile or continuous flow-type ventricular assist devices. J Am Coll Cardiol. 2004; 43:811–817.77. Wilmot I, Morales DL, Price JF, et al. Effectiveness of mechanical circulatory support in children with acute fulminant and persistent myocarditis. J Card Fail. 2011; 17:487–494.78. Morales DL, Braud BE, Price JF, et al. Use of mechanical circulatory support in pediatric patients with acute cardiac graft rejection. ASAIO J. 2007; 53:701–705.79. Irving CA, Crossland DS, Haynes S, Griselli M, Hasan A, Kirk R. Evolving experience with explantation from Berlin Heart EXCOR ventricular assist device support in children. J Heart Lung Transplant. 2014; 33:211–213.