Korean Circ J.
2015 Sep;45(5):372-377. 10.4070/kcj.2015.45.5.372.
Association between Red Blood Cell Distribution Width and Coronary Artery Calcification in Patients Undergoing 64-Multidetector Computed Tomography
- Affiliations
-
- 1Department of Cardiology, School of Medicine, Turgut Ozal University, Ankara, Turkey. drdemircelik@yahoo.com
- 2Department of Internal Medicine, Section of Nephrology, School of Medicine, Turgut Ozal University, Ankara, Turkey.
- 3Department of Cardiology, Ankara Occupational Diseases Hospital, Ankara, Turkey.
- 4Department of Internal Medicine, School of Medicine, Turgut Ozal University, Ankara, Turkey.
- KMID: 2223800
- DOI: http://doi.org/10.4070/kcj.2015.45.5.372
Abstract
- BACKGROUND AND OBJECTIVES
The red blood cell distribution width (RDW) has been found to be associated with cardiovascular morbidity and mortality. The objective of this study was to determine whether the RDW measures are associated with the coronary artery calcification score (CACS) in patients who did not present with obvious coronary heart disease (CHD).
SUBJECTS AND METHODS
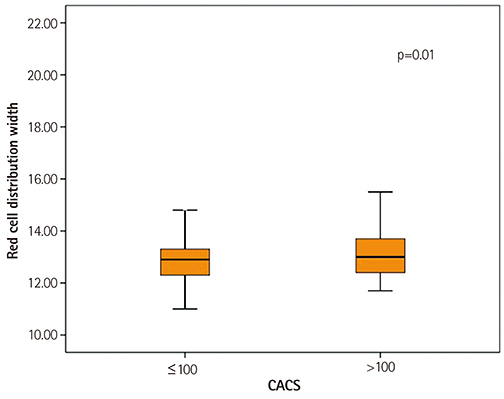
A total of 527 consecutive patients with a low to intermediate risk for CHD but without obvious disease were enrolled in this study. The study subjects underwent coronary computerized tomography angiography and CACS was calculated. The patients were divided into two groups based on CACS: Group I (CACS< or =100) and Group II (CACS>100). The two groups were compared in terms of classic CHD risk factors and haematological parameters, particularly the RDW.
RESULTS
Group I patients were younger than Group II patients. The Framingham risk score (FRS) in patients of Group II was significantly higher than that in patients of Group I. Group II patients had significantly elevated levels of haemoglobin, RDW, neutrophil count, and neutrophil/lymphocyte ratio compared with Group I patients. CACS was correlated with age, RDW, and ejection fraction. In the multivariate analysis, age, RDW, and FRS were independent predictors of CACS. Using the receiver-operating characteristic curve analysis, a RDW value of 13.05% was identified as the best cut-off for predicting the severity of CACS (>100) (area under the curve=0.706).
CONCLUSION
We found that the RDW is an independent predictor of the CACS, suggesting that it might be a useful marker for predicting CAD.
Keyword
MeSH Terms
Figure
Reference
-
1. Demir A, Yarali N, Fisgin T, Duru F, Kara A. Most reliable indices in differentiation between thalassemia trait and iron deficiency anemia. Pediatr Int. 2002; 44:612–616.2. Lappé JM, Horne BD, Shah SH, et al. Red cell distribution width, C-reactive protein, the complete blood count, and mortality in patients with coronary disease and a normal comparison population. Clin Chim Acta. 2011; 412:2094–2099.3. Felker GM, Allen LA, Pocock SJ, et al. Red cell distribution width as a novel prognostic marker in heart failure: data from the CHARM Program and the Duke Databank. J Am Coll Cardiol. 2007; 50:40–47.4. Ye Z, Smith C, Kullo IJ. Usefulness of red cell distribution width to predict mortality in patients with peripheral artery disease. Am J Cardiol. 2011; 107:1241–1245.5. Karabulut A, Uyarel H, Uzunlar B, Çakmak M. Elevated red cell distribution width level predicts worse postinterventional thrombolysis in myocardial infarction flow reflecting abnormal reperfusion in acute myocardial infarction treated with a primary coronary intervention. Coron Artery Dis. 2012; 23:68–72.6. Aung N, Dworakowski R, Byrne J, et al. Progressive rise in red cell distribution width is associated with poor outcome after transcatheter aortic valve implantation. Heart. 2013; 06. 04. [Epub]. DOI: 10.1136/heartjnl-2013-303910.7. Afonso L, Zalawadiya SK, Veeranna V, Panaich SS, Niraj A, Jacob S. Relationship between red cell distribution width and microalbuminuria: a population-based study of multiethnic representative US adults. Nephron Clin Pract. 2011; 119:c277–c282.8. Wexler L, Brundage B, Crouse J, et al. Coronary artery calcification: pathophysiology, epidemiology, imaging methods, and clinical implications. A statement for health professionals from the American Heart Association. Writing Group. Circulation. 1996; 94:1175–1192.9. Arad Y, Goodman KJ, Roth M, Newstein D, Guerci AD. Coronary calcification, coronary disease risk factors, C-reactive protein, and atherosclerotic cardiovascular disease events: the St. Francis Heart Study. J Am Coll Cardiol. 2005; 46:158–165.10. Chaikriangkrai K, Kassi M, Alchalabi S, et al. Association between hematological indices and coronary calcification in symptomatic patients without history of coronary artery disease. N Am J Med Sci. 2014; 6:433–439.11. Wilson PW, D'Agostino RB, Levy D, Belanger AM, Silbershatz H, Kannel WB. Prediction of coronary heart disease using risk factor categories. Circulation. 1998; 97:1837–1847.12. Agatston AS, Janowitz WR, Hildner FJ, Zusmer NR, Viamonte M Jr, Detrano R. Quantification of coronary artery calcium using ultrafast computed tomography. J Am Coll Cardiol. 1990; 15:827–832.13. Margolis JR, Chen JT, Kong Y, Peter RH, Behar VS, Kisslo JA. The diagnostic and prognostic significance of coronary artery calcification. A report of 800 cases. Radiology. 1980; 137:609–616.14. Budoff MJ, Shaw LJ, Liu ST, et al. Long-term prognosis associated with coronary calcification: observations from a registry of 25,253 patients. J Am Coll Cardiol. 2007; 49:1860–1870.15. Kondos GT, Hoff JA, Sevrukov A, et al. Electron-beam tomography coronary artery calcium and cardiac events: a 37-month follow-up of 5635 initially asymptomatic low- to intermediate-risk adults. Circulation. 2003; 107:2571–2576.16. Detrano R, Guerci AD, Carr JJ, et al. Coronary calcium as a predictor of coronary events in four racial or ethnic groups. N Engl J Med. 2008; 358:1336–1345.17. Olson JC, Edmundowicz D, Becker DJ, Kuller LH, Orchard TJ. Coronary calcium in adults with type 1 diabetes: a stronger correlate of clinical coronary artery disease in men than in women. Diabetes. 2000; 49:1571–1578.18. Sunkara N, Wong ND, Malik S. Role of coronary artery calcium in cardiovascular risk assessment. Expert Rev Cardiovasc Ther. 2014; 12:87–94.19. Guthrie GJ, Charles KA, Roxburgh CS, Horgan PG, McMillan DC, Clarke SJ. The systemic inflammation-based neutrophil-lymphocyte ratio: experience in patients with cancer. Crit Rev Oncol Hematol. 2013; 88:218–230.20. Bhat T, Teli S, Rijal J, et al. Neutrophil to lymphocyte ratio and cardiovascular diseases: a review. Expert Rev Cardiovasc Ther. 2013; 11:55–59.21. Ani C, Ovbiagele B. Elevated red blood cell distribution width predicts mortality in persons with known stroke. J Neurol Sci. 2009; 277:103–108.22. Weiss G, Goodnough LT. Anemia of chronic disease. N Engl J Med. 2005; 352:1011–1023.23. Lippi G, Targher G, Montagnana M, Salvagno GL, Zoppini G, Guidi GC. Relation between red blood cell distribution width and inflammatory biomarkers in a large cohort of unselected outpatients. Arch Pathol Lab Med. 2009; 133:628–632.24. de Gonzalo-Calvo D, de Luxán-Delgado B, Rodríguez-González S, et al. Interleukin 6, soluble tumor necrosis factor receptor I and red blood cell distribution width as biological markers of functional dependence in an elderly population: a translational approach. Cytokine. 2012; 58:193–198.25. Lippi G, Dipalo M, Teti L, Cervellin G. Relationship between red blood cell distribution width and prognostic biomarkers in patients admitted to the emergency department with acute infections. Eur J Intern Med. 2013; 24:e15–e16.26. Wang T, Zhang X, Li JJ. The role of NF-kappaB in the regulation of cell stress responses. Int Immunopharmacol. 2002; 2:1509–1520.27. Chistiakov DA, Orekhov AN, Bobryshev YV. Contribution of neovascularization and intraplaque haemorrhage to atherosclerotic plaque progression and instability. Acta Physiol (Oxf). 2015; 213:539–553.28. Park BJ, Shim JY, Lee HR, et al. Relationship of neutrophil-lymphocyte ratio with arterial stiffness and coronary calcium score. Clin Chim Acta. 2011; 412:925–929.29. Paulsson J, Dadfar E, Held C, Jacobson SH, Lundahl J. Activation of peripheral and in vivo transmigrated neutrophils in patients with stable coronary artery disease. Atherosclerosis. 2007; 192:328–334.30. Núñez J, Miñana G, Bodi V, et al. Low lymphocyte count and cardiovascular diseases. Curr Med Chem. 2011; 18:3226–3233.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Red Cell Distribution Width and Coronary Artery Calcification
- The Noninvasive Diagnosis and Postoperative Evaluation of Anomalous Right Coronary Artery from the Pulmonary Artery (ARCAPA) using Coronary MDCT: A Case Report
- The Relationship between Coronary Risk Factors and Coronary Calcium Score Detected by Computed Tomography Coronary Angiography in Korean Middle Aged Men
- Anomalous Origin of the Left Circumflex Coronary Artery from the Right Sinus of Valsalva Identified by Imaging with Multidetector Computed Tomography
- A Single Coronary Artery: Right Coronary Artery Originating From the Distal Left Circumflex Artery