Korean Circ J.
2015 Nov;45(6):479-485. 10.4070/kcj.2015.45.6.479.
Comparison of Prolonged Atrial Electromechanical Delays with Different Definitions in the Discrimination of Patients with Non-Valvular Paroxysmal Atrial Fibrillation
- Affiliations
-
- 1Department of Cardiology, Dong-A University Medical Center, Busan, Korea. thinkmed@dau.ac.kr
- KMID: 2223786
- DOI: http://doi.org/10.4070/kcj.2015.45.6.479
Abstract
- BACKGROUND AND OBJECTIVES
Previous studies have evaluated atrial electromechanical delays (AEMDs) with a number of different definitions to discriminate patients with paroxysmal atrial fibrillation (PAF) from controls without PAF. However, their discriminative values for PAF have not previously been directly compared.
SUBJECTS AND METHODS
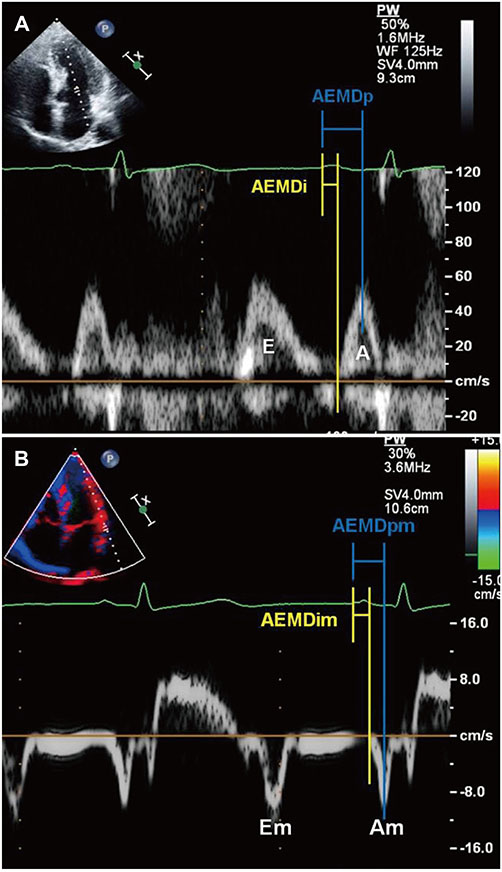
A total of 65 PAF patients and 130 control subjects matched for age, sex, history of hypertension, and diabetes mellitus were selected. The AEMDi and AEMDp were defined as the time intervals from the initiation of the P wave on the surface electrocardiogram to the initiation and peak of the late diastolic transmitral inflow on pulsed wave Doppler images, respectively. The AEMDim and AEMDpm were defined as the time intervals from the initiation of the P wave on the surface electrocardiogram to the initiation and peak of the late diastolic lateral mitral annular motion on tissue Doppler images, respectively.
RESULTS
There were no significant differences in the clinical characteristics between the two groups. All 4 AEMDs were consistently longer in the PAF group, and proven effective to differentiate the PAF patients from the controls. The AEMDi measurement had a larger area under the curve (AUC) than the other AEMDs, left atrial volume index, and P wave amplitude. However, the AEMDp, AEMDim, and AEMDpm measurements had AUCs similar to those of the left atrial volume index and P wave amplitude.
CONCLUSION
The findings suggest that the AEMDi is better than the other AEMDs for the discrimination of PAF patients from the controls.
MeSH Terms
Figure
Reference
-
1. Omi W, Nagai H, Takamura M, et al. Doppler tissue analysis of atrial electromechanical coupling in paroxysmal atrial fibrillation. J Am Soc Echocardiogr. 2005; 18:39–44.2. Cui Q, Wang H, Wang H, Zhang W. Differences in atrial electromechanical coupling and atrial volume in patients with idiopathic paroxysmal atrial fibrillation. Acta Cardiol. 2008; 63:701–705.3. Weijs B, de Vos CB, Limantoro I, Cheriex EC, Tieleman RG, Crijns HJ. The presence of an atrial electromechanical delay in idiopathic atrial fibrillation as determined by tissue Doppler imaging. Int J Cardiol. 2012; 156:121–122.4. Cui QQ, Zhang W, Wang H, et al. Assessment of atrial electromechanical coupling and influential factors in nonrheumatic paroxysmal atrial fibrillation. Clin Cardiol. 2008; 31:74–78.5. Chao TF, Sung SH, Wang KL, et al. Atrial electromechanical interval can identify patients with paroxysmal atrial fibrillation and is associated with CHADS2 score and peak velocity of left atrial appendage. J Cardiovasc Electrophysiol. 2011; 22:1325–1330.6. Park SM, Kim YH, Choi JI, Pak HN, Kim YH, Shim WJ. Left atrial electromechanical conduction time can predict six-month maintenance of sinus rhythm after electrical cardioversion in persistent atrial fibrillation by Doppler tissue echocardiography. J Am Soc Echocardiogr. 2010; 23:309–314.7. Chao TF, Sung SH, Wang KL, et al. Associations between the atrial electromechanical interval, atrial remodelling and outcome of catheter ablation in paroxysmal atrial fibrillation. Heart. 2011; 97:225–230.8. Roshanali F, Mandegar MH, Yousefnia MA, Rayatzadeh H, Alaeddini F, Amouzadeh F. Prediction of atrial fibrillation via atrial electromechanical interval after coronary artery bypass grafting. Circulation. 2007; 116:2012–2017.9. De Vos CB, Weijs B, Crijns HJ, et al. Atrial tissue Doppler imaging for prediction of new-onset atrial fibrillation. Heart. 2009; 95:835–840.10. den Uijl DW, Gawrysiak M, Tops LF, et al. Prognostic value of total atrial conduction time estimated with tissue Doppler imaging to predict the recurrence of atrial fibrillation after radiofrequency catheter ablation. Europace. 2011; 13:1533–1540.11. Lang RM, Bierig M, Devereux RB, et al. Recommendations for chamber quantification: a report from the American Society of Echocardiography's Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J Am Soc Echocardiogr. 2005; 18:1440–1463.12. Quiñones MA, Otto CM, Stoddard M, et al. Recommendations for quantification of Doppler echocardiography: a report from the Doppler Quantification Task Force of the Nomenclature and Standards Committee of the American Society of Echocardiography. J Am Soc Echocardiogr. 2002; 15:167–184.13. Magnani JW, Johnson VM, Sullivan LM, et al. P wave duration and risk of longitudinal atrial fibrillation in persons ≥ 60 years old (from the Framingham Heart Study). Am J Cardiol. 2011; 107:917–921.e1.14. Fukunami M, Yamada T, Ohmori M, et al. Detection of patients at risk for paroxysmal atrial fibrillation during sinus rhythm by P wave-triggered signal-averaged electrocardiogram. Circulation. 1991; 83:162–169.15. Vaziri SM, Larson MG, Benjamin EJ, Levy D. Echocardiographic predictors of nonrheumatic atrial fibrillation. The Framingham Heart Study. Circulation. 1994; 89:724–730.16. Barbier P, Alioto G, Guazzi MD. Left atrial function and ventricular filling in hypertensive patients with paroxysmal atrial fibrillation. J Am Coll Cardiol. 1994; 24:165–170.17. Weijs B, de Vos CB, Tieleman RG, et al. Clinical and echocardiographic correlates of intra-atrial conduction delay. Europace. 2011; 13:1681–1687.18. Pala S, Tigen K, Karaahmet T, et al. Assessment of atrial electromechanical delay by tissue Doppler echocardiography in patients with nonischemic dilated cardiomyopathy. J Electrocardiol. 2010; 43:344–350.19. Erturk M, Aslan M, Aksu HU, et al. Evaluation of atrial electromechanic delay and left atrial mechanical functions in the patients with secundum type atrial septal defect. Echocardiography. 2013; 30:699–705.20. Acar G, Akcay A, Sokmen A, et al. Assessment of atrial electromechanical delay, diastolic functions, and left atrial mechanical functions in patients with type 1 diabetes mellitus. J Am Soc Echocardiogr. 2009; 22:732–738.21. Lim HE, Kim YH, Kim SH, et al. Impact of obstructive sleep apnea on the atrial electromechanical activation time. Circ J. 2009; 73:249–255.22. Mizuno R, Fujimoto S, Nakano H, et al. Atrial conduction abnormalities in patients with systemic progressive sclerosis. Eur Heart J. 1997; 18:1995–2001.23. Karabag T, Aydin M, Dogan SM, et al. Investigation of the atrial electromechanical delay duration in Behcet patients by tissue Doppler echocardiography. Eur Heart J Cardiovasc Imaging. 2012; 13:251–256.24. Sengul C, Cevik C, Ozveren O, et al. Acute alcohol consumption is associated with increased interatrial electromechanical delay in healthy men. Cardiol J. 2011; 18:682–686.25. Ozturk S, Dikbas O, Ozyasar M, et al. Evaluation of left atrial mechanical functions and atrial conduction abnormalities in patients with clinical hypothyroid. Cardiol J. 2012; 19:287–294.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Atrial Electromechanical Coupling in Patients with Lichen Planus
- The Joint Multicenter Study on the Atrial Fibrillation in Korea
- A Case of Paroxysmal Atrial Fibrillation and Sinus Bradycardia due to Coronary Artery Spasm
- Relation of Right Atrial Pathology to Atrial Fibrillation in Mitral Valvular Disease
- A clinical observation on antiarrhythmic efficacy of propafenone for atrial fibrillation