J Rheum Dis.
2013 Dec;20(6):374-377. 10.4078/jrd.2013.20.6.374.
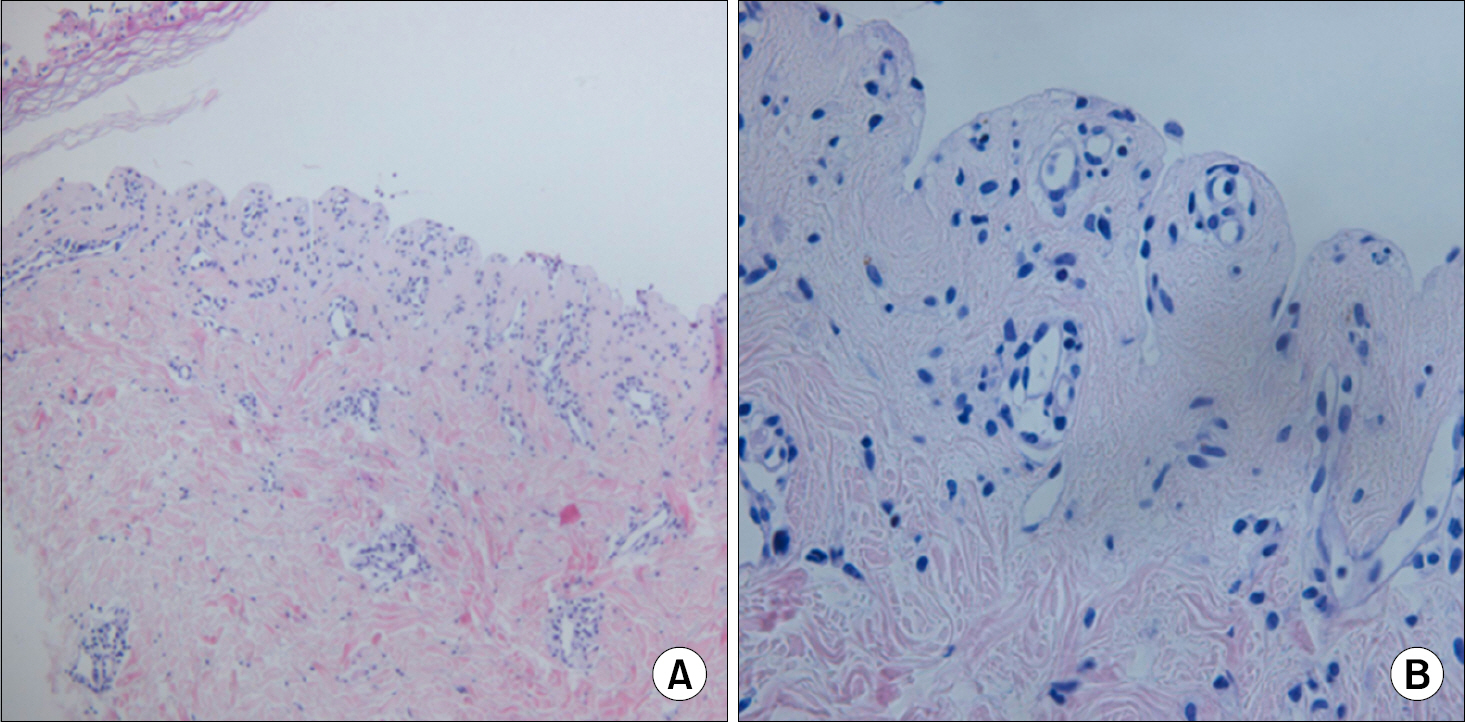
Toxic Epidermal Necrolysis by Ceftriaxone in Patient with Newly Diagnosed Systemic Lupus Erythematosus
- Affiliations
-
- 1Division of Rheumatology, Department of Internal Medicine, School of Medicine, The Catholic University of Korea, Incheon, Korea. rhcow1@yahoo.co.kr
- KMID: 2222997
- DOI: http://doi.org/10.4078/jrd.2013.20.6.374
Abstract
- Toxic epidermal necrolysis (TEN) is a rare disease in absolute numbers with an incidence of 2 cases per million people per year. Most cases of TEN are caused by drugs, but certain infectious diseases may have an impact on the risk. There are rare reports of TEN occurring without history of drug ingestion in systemic lupus erythematosus (SLE), appearing similar to cutaneous lupus and early TEN manifestations, such as erythema multiforme. This report describes a patient with SLE who presented with manifestations of TEN after ceftriaxone treatment. The patient was newly diagnosed with SLE and TEN occurring eight days after cessation of ceftriaxone. Considering possible etiologies, we could not exclude ceftriaxone as the cause of TEN. After intravenous immunoglobulin with glucocorticoid, clinical symptoms improved.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Harr T, French LE. Toxic epidermal necrolysis and Stevens-Johnson syndrome. Orphanet J Rare Dis. 2010; 5:39.
Article2. Halevy S, Ghislain PD, Mockenhaupt M, Fagot JP, Bouwes Bavinck JN, Sidoroff A, et al. EuroSCAR Study Group. Allopurinol is the most common cause of Stevens-Johnson syndrome and toxic epidermal necrolysis in Europe and Israel. J Am Acad Dermatol. 2008; 58:25–32.
Article3. Heymann WR. Toxic epidermal necrolysis 2006. J Am Acad Dermatol. 2006; 55:867–9.
Article4. Mandelcorn R, Shear NH. Lupus-associated toxic epidermal necrolysis: a novel manifestation of lupus? J Am Acad Dermatol. 2003; 48:525–9.
Article5. Obermoser G, Sontheimer RD, Zelger B. Overview of common, rare and atypical manifestations of cutaneous lupus erythematosus and histopathological correlates. Lupus. 2010; 19:1050–70.
Article6. Lee HY, Tey HL, Pang SM, Thirumoorthy T. Systemic lupus erythematosus presenting as Stevens-Johnson syndrome and toxic epidermal necrolysis: a report of three cases. Lupus. 2011; 20:647–52.
Article7. Horne NS, Narayan AR, Young RM, Frieri M. Toxic epidermal necrolysis in systemic lupus erythematosus. Autoimmun Rev. 2006; 5:160–4.
Article8. Lateef A, Tan KB, Lau TC. Acute generalized ex-anthematous pustulosis and toxic epidermal necrolysis induced by hydroxychloroquine. Clin Rheumatol. 2009; 28:1449–52.
Article9. Callaly EL, FitzGerald O, Rogers S. Hydroxychloroquine- associated, photo-induced toxic epidermal necrolysis. Clin Exp Dermatol. 2008; 33:572–4.10. Ziemer M, Kardaun SH, Liss Y, Mockenhaupt M. Stevens-Johnson syndrome and toxic epidermal necrolysis in patients with lupus erythematosus: a descriptive study of 17 cases from a national registry and review of the literature. Br J Dermatol. 2012; 166:575–600.
Article11. Sassolas B, Haddad C, Mockenhaupt M, Dunant A, Liss Y, Bork K, et al. ALDEN, an algorithm for assessment of drug causality in Stevens-Johnson Syndrome and toxic epidermal necrolysis: comparison with case-control analysis. Clin Pharmacol Ther. 2010; 88:60–8.
Article12. Mockenhaupt M. The current understanding of Stevens-Johnson syndrome and toxic epidermal necrolysis. Expert Rev Clin Immunol. 2011; 7:803–13.
Article13. Mockenhaupt M. Severe drug-induced skin reactions: clinical pattern, diagnostics and therapy. J Dtsch Dermatol Ges. 2009; 7:142–60.
Article14. Ghislain PD, Roujeau JC. Treatment of severe drug re-actions: Stevens-Johnson syndrome, toxic epidermal necrolysis and hypersensitivity syndrome. Dermatol Online J. 2002; 8:5.
Article15. Araki Y, Sotozono C, Inatomi T, Ueta M, Yokoi N, Ueda E, et al. Successful treatment of Stevens-Johnson syndrome with steroid pulse therapy at disease onset. Am J Ophthalmol. 2009; 147:1004–11.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Infectious Mononucleosis-like Syndrome Induced by Ceftriaxone and Isepamicin in a Patient with Systemic Lupus Erythematosus
- A Case of Carbamazepine- Induced- Toxic Epidermal Necrolysis
- Adalimumab-induced Lupus Erythematosus Profundus in a Rheumatoid Arthritis Patient
- Salmonella osteomyelitis with osteonecrosis in a patient with systemic lupus erythematosus
- A Case of Transverse Myelitis as a First Manifestation of Systemic Lupus Erythematosus