J Korean Ophthalmol Soc.
2014 Sep;55(9):1366-1371. 10.3341/jkos.2014.55.9.1366.
The Effects of Commodified Growth Factor Products on the Fibrovascularization of Porous Polyethylene Orbital Implants
- Affiliations
-
- 1Department of Ophthalmology, Yeungnam University College of Medicine, Daegu, Korea. sjh@med.yu.ac.kr
- 2Department of Pathology, Yeungnam University College of Medicine, Daegu, Korea.
- KMID: 2217122
- DOI: http://doi.org/10.3341/jkos.2014.55.9.1366
Abstract
- PURPOSE
To investigate the effects of commodified growth factor products used clinically on fibrovascular ingrowth into porous polyethylene orbital implants.
METHODS
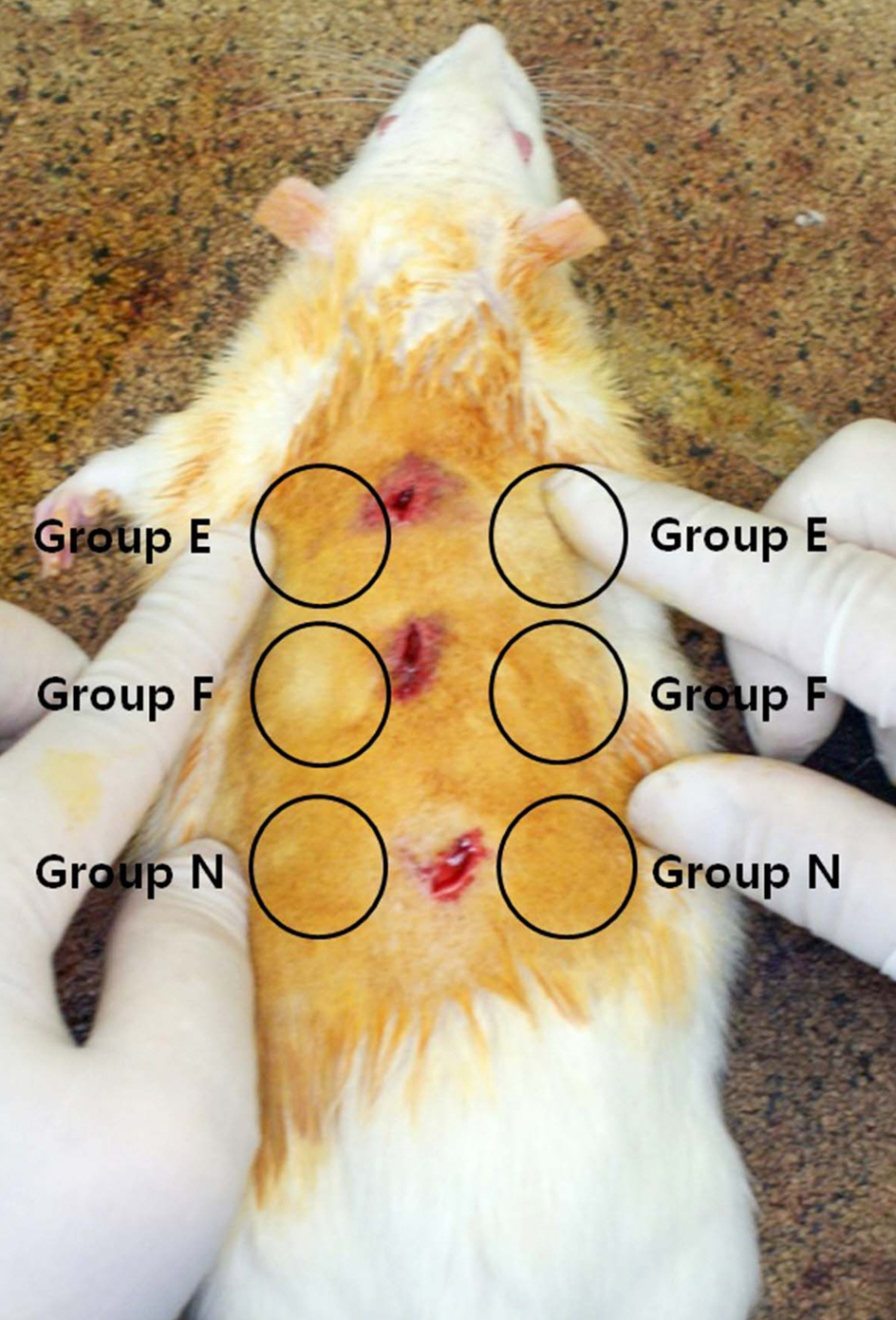
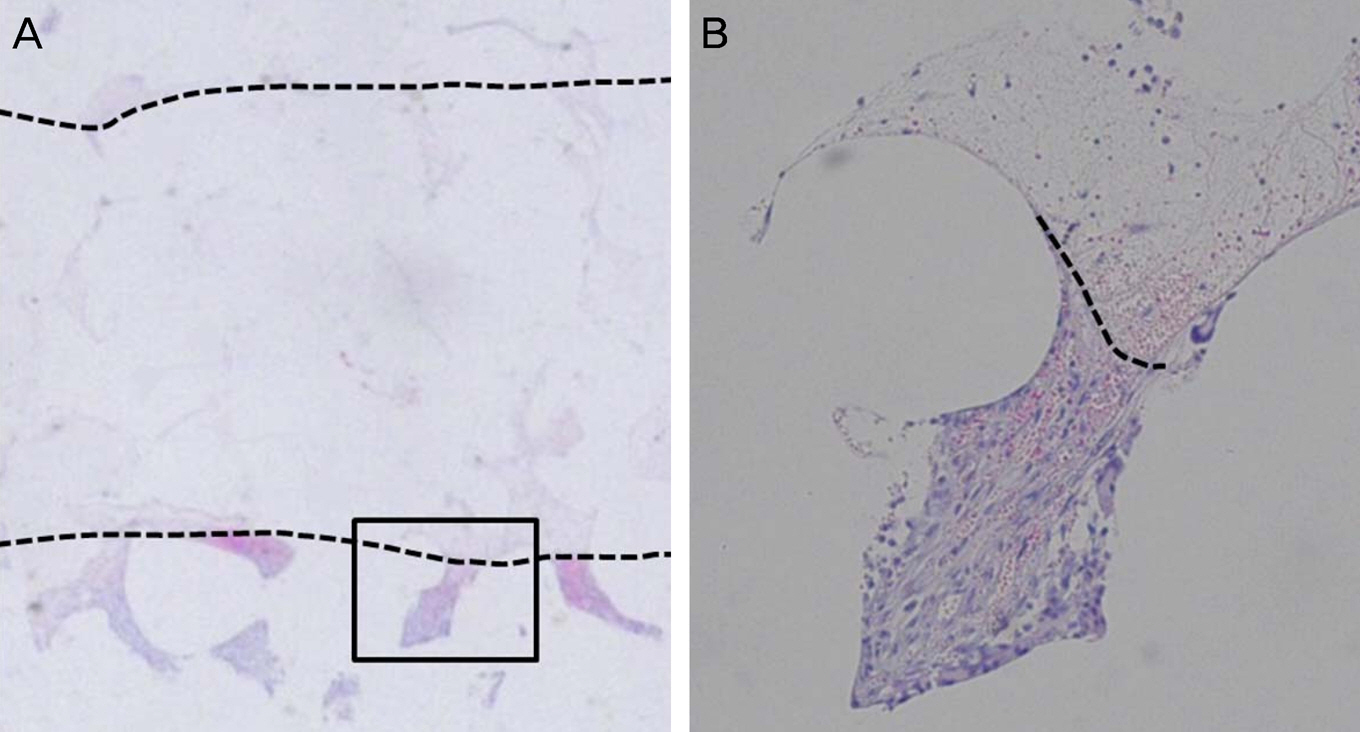
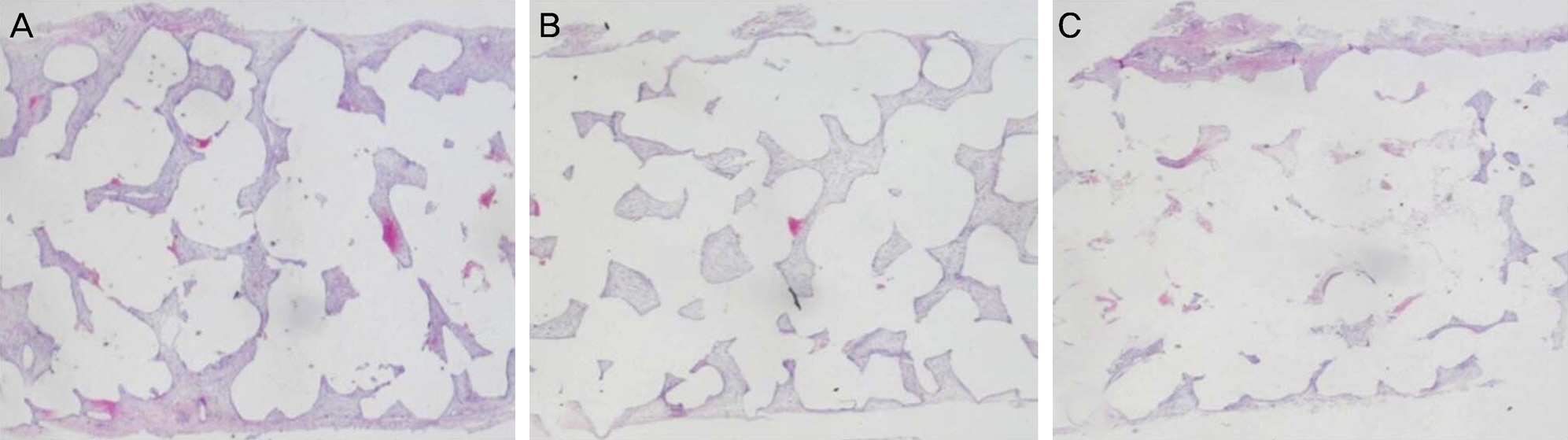
Porous polyethylene orbital implant sheets (Medpor(R)) soaked with Nepidermin (Easyef(R)), Trafermin (Fiblast(R)), and normal saline were implanted into the backs of 18 Sprague-Dawley rats. The degree of fibrovascular ingrowth as observed using a light microscope was compared 1 and 2 weeks after implantation and was calculated as a percentage of the fibrovascular ingrowth length.
RESULTS
One week after implantation, the percentage of fibrovascular ingrowth length was 25.33 +/- 5.43%, 22.56 +/- 5.30%, and 21.78 +/- 4.66% in the Easyef(R)-, Fiblast(R)- and normal saline-soaked groups. The degree of fibrovascularization was higher in the Easyef(R)-soaked group than in the other groups (p = 0.020, 0.012). Two weeks after implantation, the degree of fibrovascularization was 98.33 +/- 5.00%, 100.00 +/- 0.00%, and 95.89 +/- 4.57%, which was significantly higher in the Easyef(R)-, and Fiblast(R)-soaked groups than in normal saline-soaked group (p = 0.019, <0.001).
CONCLUSIONS
Commodified growth factor products used in other areas selectively enhanced fibrovascular ingrowth to a greater degree and earlier in ophthalmic plastic and reconstructive surgery.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Rubin PA, Popham JK, Bilyk JR, Shore JW. Comparison of fibrovascular ingrowth into hydroxyapatite and porous polyethylene orbital implants. Ophthal Plast Reconstr Surg. 1994; 10:96–103.
Article2. Romano JJ, Iliff NT, Manson PN. Use of Medpor® porous polyethylene implants in 140 patients with facial fractures. J Craniofac Surg. 1993; 4:142–7.
Article3. Yoon HJ, Kim SJ, Yoon SW, Yoon YS. Effects of Medpor® sheet as substitute for tarsus in eyelid reconstruction. J Korean Ophthalmol Soc. 2009; 50:1098–104.
Article4. Purdy EP. Oculoplastic and orbital applications of porous high-density polyethylene implants. Curr Opin Ophthalmol. 1997; 8:57–63.
Article5. Mawn LA, Jordan DR, Gilberg S. Scanning electron microscopic examination of porous orbital implants. Can J Ophthalmol. 1998; 33:203–9.6. Karesh JW, Dresner SC. High-density porous polyethylene (Medpor®) as a successful anophthalmic socket implant. Ophthalmology. 1994; 101:1688–95. discussion 1695-6.
Article7. Nicaeus TE, Tolentino MJ, Adamis AP, Rubin PA. Sucralfate and basic fibroblast growth factor promote endothelial cell proliferation around porous alloplastic implants in vitro. Ophthal Plast Reconstr Surg. 1996; 12:235–9.
Article8. Soparkar CN, Wong JF, Patrinely JR, Appling D. Epidermal and fibroblast growth factors enhance fibrovascular integration of porous polyethylene implants. Ophthal Plast Reconstr Surg. 2000; 16:337–40.
Article9. Soe SG, Kim YI, Shin SG, Oum BS. Study on fibrovascular ingrowth into the intraocular implant, Medpor®. J Korean Ophthalmol Soc. 2002; 43:1310–22.10. Kim KR, Jung CS, Chung SK. The effect of basic fibroblast growth factor on the vascularization of porous polyethylene orbital implant (Medpor®). J Korean Ophthalmol Soc. 2002; 43:2258–64.11. Choi YS, Yim HB, Choi WC. The effect of vascular endothelial growth factor on vascularization in porous polyethylene orbital implant (Medpor®). J Korean Ophthalmol Soc. 2003; 44:1180–7.12. Han SK, You HJ. Wound coverage using advanced technology in Korea. J Korean Med Assoc. 2011; 54:594–603.
Article13. Hong JP, Jung HD, Kim YW. Recombinant human epidermal growth factor (EGF) to enhance healing for diabetic foot ulcers. Ann Plast Surg. 2006; 56:394–8.
Article14. Cho JH, Lew DH, Kim YS, Tark KC. Treatment of acute and chronic wound in immunodeficiency patients using Easyef® (EGF). J Korean Soc Transplant. 2006; 20:99–103.15. Akita S, Akino K, Imaizumi T, Hirano A. Basic fibroblast growth factor accelerates and improves second-degree burn wound healing. Wound Repair Regen. 2008; 16:635–41.
Article16. Uemura T. Evaluation with trafermin for pediatric thermal burn in outpatients. NESSHO-TOKYO-. 2006; 32:291–7.17. Ishibashi Y, Soeda S, Ohura T, et al. The clinical effects of KCB-1 on skin ulcers: a double blind trial to investigate an optimal dose. Rinsho Iyaku. 1996; 12:1809–34.18. Perry AC. Integrated orbital implants. Adv Ophthalmic Plast Reconstr Surg. 1990; 8:75–81.
Article19. Woo KI, Kim JM, Chang HR, et al. The effect of growth factors and surgical procedures on fibrovascular ingrowth into anophthalmic socket implant of porous polyethylene. J Korean Ophthalmol Soc. 2000; 41:2725–31.20. Rubin PA, Nicaeus TE, Warner MA, Remulla HD. Effect of sucralfate and basic fibroblast growth factor on fibrovascular ingrowth into hydroxyapatite and porous polyethylene alloplastic implants using a novel rabbit model. Ophthal Plast Reconstr Surg. 1997; 13:8–17.
Article21. Park WC, Han SK, Kim NJ, et al. Effect of basic fibroblast growth factor on fibrovascular ingrowth into porous polyethylene anophthalmic socket implants. Korean J Ophthalmol. 2005; 19:1–8.
Article22. Cho NC, Lee MC, Han HJ, Ahn BG. Proliferative effect of retinal glial cells by growth factors. J Korean Ophthalmol Soc. 1997; 38:1179–87.23. Yoon HS, Rho SH, Lee SC, et al. The effects of TGF-β2 and bFGF on the proliferation of retinal pigment epithelial cells. J Korean Ophthalmol Soc. 1998; 39:1192–203.24. Kwak NH, Cuhn MH, Yoo JS, Huh W. Neurotropic effect of basic fibroblast growth factor on laser wound. J Korean Ophthalmol Soc. 2000; 41:1666–73.25. Hirano M, Pavlakis SG. Mitochondrial myopathy, encephalopathy, lactic acidosis, and strokelike episodes (MELAS): current concepts. J Child Neurol. 1994; 9:4–13.26. Kurten RC, Chowdhury P, Sanders RC Jr, et al. Coordinating epidermal growth factor-induced motility promotes efficient wound closure. Am J Physiol Cell Physiol. 2005; 288:C109–21.
Article27. Motomura H, Ohashi N, Harada T, et al. Aggressive conservative therapy for refractory ulcer with diabetes and/or arteriosclerosis. J Dermatol. 2006; 33:353–9.
Article28. Bigham WJ, Stanley P, Cahill JM Jr, et al. Fibrovascular ingrowth in porous ocular implants: the effect of material composition, porosity, growth factors, and coatings. Ophthal Plast Reconstr Surg. 1999; 15:317–25.29. Jang JH, Chang SD. Upper eyelid reconstruction using the Medpor® sheet and median forehead flap. J Korean Ophthalmol Soc. 2009; 50:1105–10.
Article30. Lim JY, Jang JW, Moon SH. Lid reconstruction using the porous polyethylene (Medpor®) sheet. J Korean Ophthalmol Soc. 2003; 44:2111–6.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effect of Basic Fibroblast Growth Factor on Fibrovascular Ingrowth into Porous Polyethylene Anophthalmic Socket Implants
- Study on Fibrovascular Ingrowth into the Intraocular Implant, Medpor(R)
- The Effect of the Synthetic Bone Glass on the Fibrovascularization into Porous Polyethylene Orbital Implant
- Morphological Study of a New Orbital Implant: Hydroxyapatite-Coated Porous Alumina in Rabbit
- Scleral Eversion Technique for Porous Polyethylene Orbital Implant after Evisceration