J Korean Ophthalmol Soc.
2013 May;54(5):704-708. 10.3341/jkos.2013.54.5.704.
Clinical Outcomes of Penetrating Keratoplasty in Patients Five Years or Younger
- Affiliations
-
- 1Department of Ophthalmology, Seoul National University College of Medicine, Seoul, Korea. jooyounoh77@gmail.com
- 2Seoul National University Hospital Healthcare System Gangnam Center, Seoul, Korea.
- KMID: 2217034
- DOI: http://doi.org/10.3341/jkos.2013.54.5.704
Abstract
- PURPOSE
To investigate the clinical outcomes of primary pediatric keratoplasty.
METHODS
Records of patients who underwent penetrating keratoplasty at the age of 5 years or younger were retrospectively reviewed. The survival rates of corneal grafts, postoperative complications, and causes of graft failure were evaluated.
RESULTS
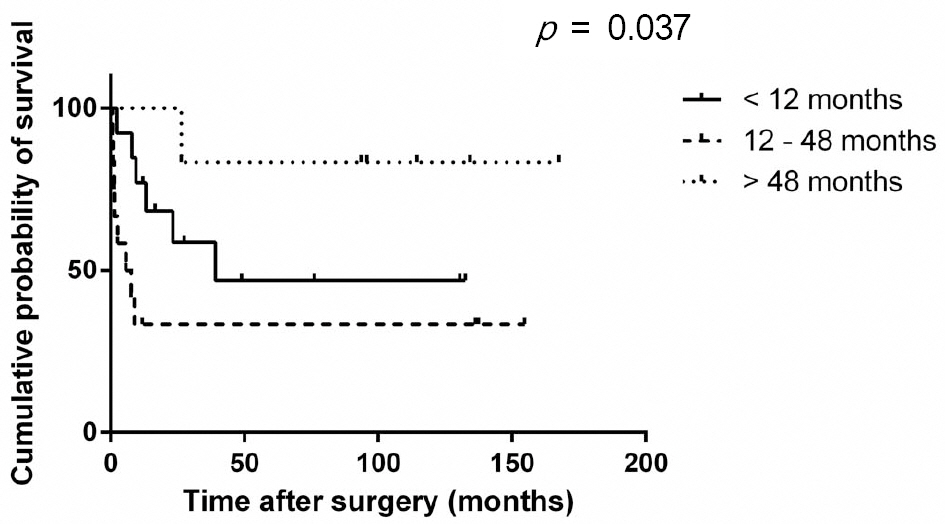
A total of 31 penetrating keratoplasties were performed in 29 patients, two of which were bilateral. The mean follow-up period was 78.72 +/- 8.94 months. The overall graft survival rate was 51.61%. The graft survival rate was 77.4% at 6 months, 61.3% at 12 months, 57.5% at 2 years, and 49.5% at 5 years after the surgery (the median survival time, 39.2 months). The main surgical indications included sclerocornea (35.5%), followed by Peter's anomaly (25.8%) and congenital glaucoma (9.7%). There were significant differences in graft survival time among the surgical indications, of which sclerocornea was the worst (p = 0.003). The main cause of graft failure was rejection (46.7%), followed by infection (26.7%) and primary endothelial decompensation (20%). When patients were sub-grouped according to age (under 12 months, between 12 to 48 months, and over 48 months), there was significant difference in graft survival time (p = 0.037) but not in overall graft survival rate (p = 0.154). Graft rejection occurred more frequently in patients between 12 to 48 months of age compared to other age groups (p = 0.016). Three out of 13 graft infections occurred in patients under 12 months of age.
CONCLUSIONS
The type of disease causing corneal opacity was a significant factor affecting the clinical outcomes of penetrating keratoplasty in children.
MeSH Terms
Figure
Reference
-
References
1. Bermejo E, Martinez-Frias ML. Congenital eye malformations: clinical-epidemiological analysis of 1,124,654 consecutive births in Spain. Am J Med Genet. 1998; 75:497–504.
Article2. Ganekal S, Gangangouda C, Dorairaj S, Jhanji V. Early outcomes of primary pediatric keratoplasty in patients with acquired, atrau-matic corneal pathology. J AAPOS. 2011; 15:353–5.
Article3. Vanathi M, Panda A, Vengayil S, et al. Pediatric keratoplasty. Surv Ophthalmol. 2009; 54:245–71.
Article4. Al-Ghamdi A, Al-Rajhi A, Wagoner MD. Primary pediatric keratoplasty: indications, graft survival, and visual outcome. J AAPOS. 2007; 11:41–7.
Article5. McClellan K, Lai T, Grigg J, Billson F. Penetrating keratoplasty in children: visual and graft outcome. Br J Ophthalmol. 2003; 87:1212–4.
Article6. Stulting RD, Sumers KD, Cavanagh HD, et al. Penetrating kerato-plasty in children. Ophthalmology. 1984; 91:1222–30.
Article7. Lowe MT, Keane MC, Coster DJ, Williams KA. The outcome of corneal transplantation in infants, children, and adolescents. Ophthalmology. 2011; 118:492–7.
Article8. Dana MR, Schaumberg DA, Moyes AL, Gomes JA. Corneal trans-plantation in children with Peters anomaly and mesenchymal dysgenesis. Multicenter Pediatric Keratoplasty Study. Ophthalmology. 1997; 104:1580–6.9. Rao KV, Fernandes M, Gangopadhyay N, et al. Outcome of pene-trating keratoplasty for Peters anomaly. Cornea. 2008; 27:749–53.
Article10. Yang LL, Lambert SR, Drews-Botsch C, Stulting RD. Long-term visual outcome of penetrating keratoplasty in infants and children with Peters anomaly. J AAPOS. 2009; 13:175–80.
Article11. Yang LL, Lambert SR, Lynn MJ, Stulting RD. Long-term results of corneal graft survival in infants and children with peters anomaly. Ophthalmology. 1999; 106:833–48.
Article12. Huang C, O'Hara M, Mannis MJ. Primary pediatric keratoplasty: indications and outcomes. Cornea. 2009; 28:1003–8.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Cataract Extraction after Penetrating Keratoplasty
- Patho-Physiology of Penetrating Keratoplasty
- Traumatic Wound Dehiscence after Penetrating Keratoplasty
- Astigmatism after Penetrating Keratoplasty According to Suture Methods
- A Case of Resolved Massive Suprachoroidal Hemorrhage after Sclerotomy in Penetrating Keratoplasty Patient