J Korean Ophthalmol Soc.
2014 Nov;55(11):1721-1725. 10.3341/jkos.2014.55.11.1721.
Optic Neuritis Mimicking Ischemic Optic Neuropathy and Optic Glioma
- Affiliations
-
- 1Institute of Vision Research, Department of Ophthalmology, Yonsei University College of Medicine, Seoul, Korea. saminhong@gmail.com
- KMID: 2216625
- DOI: http://doi.org/10.3341/jkos.2014.55.11.1721
Abstract
- PURPOSE
To report a case of optic neuritis difficult to differentiate from ischemic optic neuropathy and optic nerve glioma.
CASE SUMMARY
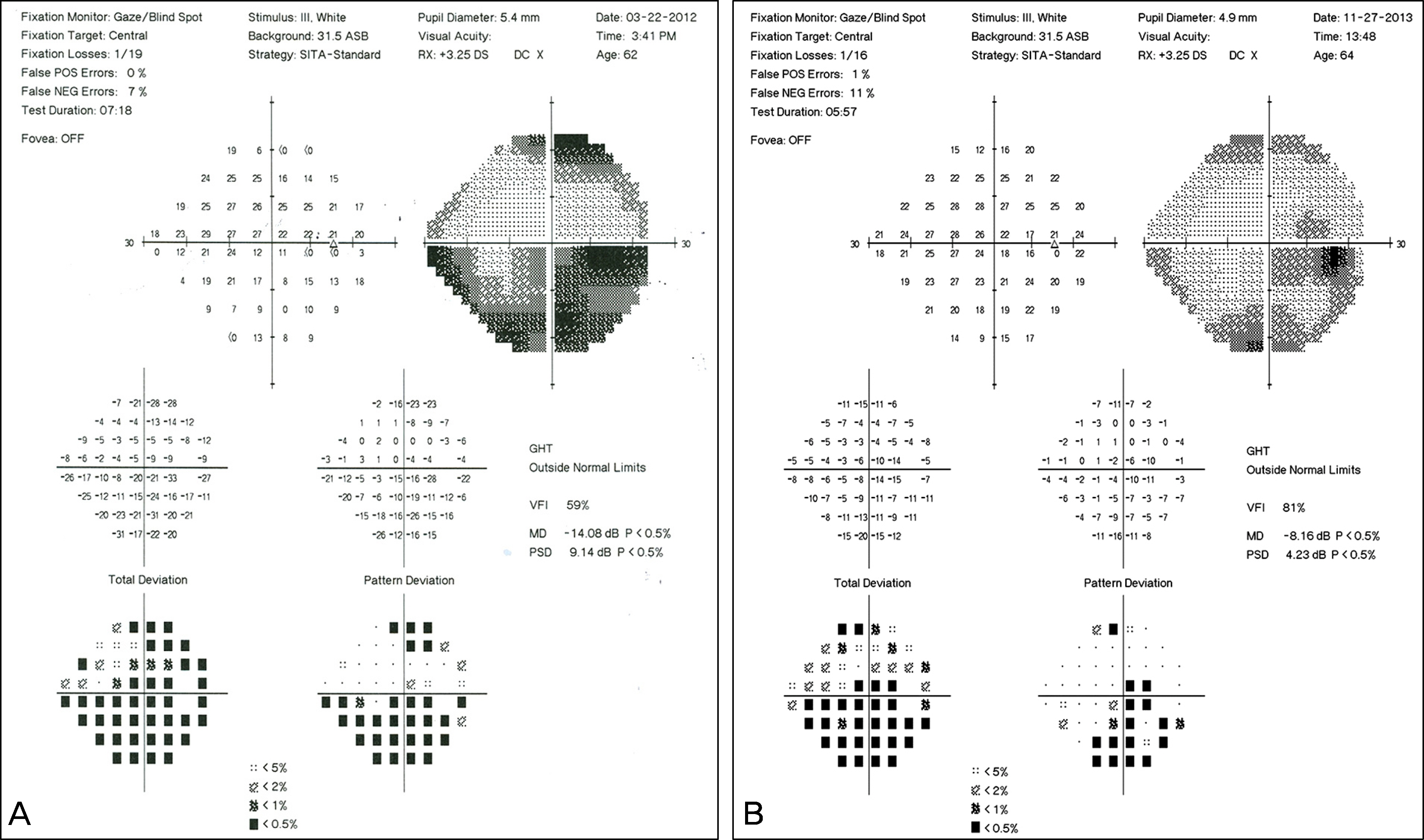
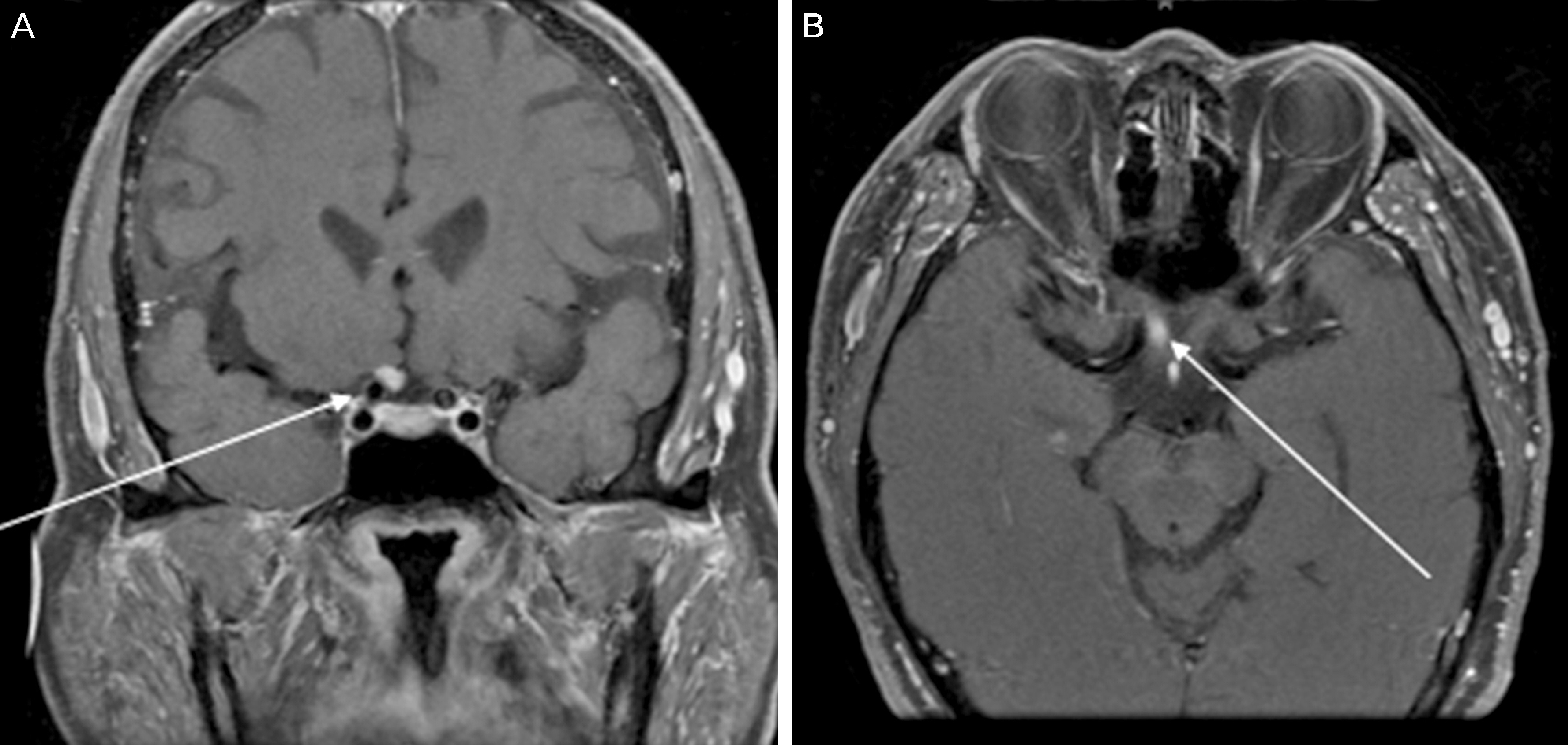
A 63-year-old male visited our clinic because of a sudden painless decrease in visual acuity in his right eye. He had a relative afferent pupillary defect and inferior altitudinal scotoma with disc pallor in his right eye. Ischemic optic neuropathy was suspected based on these clinical observations. However, a focal enhancing lesion was found in the intracranial portion of the right optic nerve on gadolinium-enhanced T1-weighted MRI. The radiologist's report revealed right intracranial optic glioma. Optic neurectomy was planned in accordance with the suspicion for optic glioma. However, a systemic mega-dose methylprednisolone therapy which is relatively less invasive was performed first based on the decision that optic neuritis should be distinguished from optic nerve glioma. The patient was hospitalized and 1 gram of methylprednisolone was injected intravenously daily for 3 days. The patient's visual acuity in the right eye improved from 0.1 before treatment to 0.3 after treatment. MRI scans at 8 months after steroid treatment showed disappearance of the previously enhanced lesion suspicious for optic glioma with developed atrophic change. The patient was finally diagnosed with optic neuritis based on these results.
CONCLUSIONS
Careful differential diagnoses and therapeutic approaches to possible diseases are necessary because optic neuritis can manifest as a variety of clinical entities and imaging findings.
MeSH Terms
Figure
Reference
-
References
1. Fazzone HE, Lefton DR, Kupersmith MJ. Optic neuritis: correlation of pain and magnetic resonance imaging. Ophthalmology. 2003; 110:1646–9.2. Lepore FE. The origin of pain in optic neuritis. Determinants of pain in 101 eyes with optic neuritis. Arch Neurol. 1991; 48:748–9.3. Lury KM, Smith JK, Matheus MG, Castillo M. Neurosarcoidosis–review of imaging findings. Semin Roentgenol. 2004; 39:495–504.
Article4. Bergmann M, Brück W, Neubauer U, Probst-Cousin S. Diagnostic pitfall: optic neuritis mimicking optic nerve glioma. Neuropathology. 2009; 29:450–3.
Article5. Tumialán LM, Dhall SS, Biousse V, Newman NJ. Optic nerve glioma and optic neuritis mimicking one another: case report. Neurosurgery. 2005; 57:E190. discussion E190.
Article6. Characteristics of patients with nonarteritic anterior ischemic optic neuropathy eligible for the Ischemic Optic Neuropathy Decompression Trial. Arch Ophthalmol. 1996; 114:1366–74.7. The clinical profile of optic neuritis. Experience of the Optic Neuritis Treatment Trial. Optic Neuritis Study Group. Arch Ophthalmol. 1991; 109:1673–8.8. Fazzone HE, Lefton DR, Kupersmith MJ. Optic neuritis: correlation of pain and magnetic resonance imaging. Ophthalmology. 2003; 110:1646–9.9. Kupersmith MJ, Alban T, Zeiffer B, Lefton D. Contrast-enhanced MRI in acute optic neuritis: relationship to visual performance. Brain. 2002; 125(Pt 4):812–22.
Article10. Mesiwala AH, Loeser JD. Visual pathway glioma. Pediatr Neurosurg. 2002; 36:161.
Article11. Rothfus WE, Curtin HD, Slamovits TL, Kennerdell JS. Optic nerve/sheath enlargement. A differential approach based on high-resolution CT morphology. Radiology. 1984; 150:409–15.
Article12. Ahn Y, Cho BK, Kim SK, et al. Optic pathway glioma: outcome and prognostic factors in a surgical series. Childs Nerv Syst. 2006; 22:1136–42.
Article13. CHUTORIAN AM, SCHWARTZ JF, EVANS RA, CARTER S. OPTIC GLIOMAS IN CHILDREN. Neurology. 1964; 14:83–95.
Article14. Millar WS, Tartaglino LM, Sergott RC, et al. MR of malignant optic glioma of adulthood. AJNR Am J Neuroradiol. 1995; 16:1673–6.15. Hoyt WF, Meshel LG, Lessell S, et al. Malignant optic glioma of adulthood. Brain. 1973; 96:121–32.
Article16. Hartel PH, Rosen C, Larzo C, Nestor S. Malignant optic nerve glioma (glioblastoma multiforme): A case report and literature review. W V Med J. 2006; 102:29–31.17. Wabbels B, Demmler A, Seitz J, et al. Unilateral adult malignant optic nerve glioma. Graefes Arch Clin Exp Ophthalmol. 2004; 242:741–8.
Article18. Dinh TT, Wang YY, Rosenfeld JV, Cherny M. Glioblastoma of the optic chiasm. J Clin Neurosci. 2007; 14:502–5.
Article19. Shapey J, Danesh-Meyer HV, Kaye AH. Diagnosis and management of optic nerve glioma. J Clin Neurosci. 2011; 18:1585–91.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Etiology of Optic Neuropathy
- Comparison of Optic Disc Appearance in Anterior ischemic optic neuropathy and Optic neuritis
- Correlation between Visual Acuity and Retinal Nerve Fiber Layer Thickness in Optic Neuropathies
- Optic Neuropathy with Diffusion Weighted High Signal Changes in Optic Nerve
- A Clinical Study of the Optic Nerve Diseases