J Korean Ophthalmol Soc.
2012 Jul;53(7):1023-1026. 10.3341/jkos.2012.53.7.1023.
A Case of Syringocystadenoma Papilliferum of the Eyelid
- Affiliations
-
- 1Department of Ophthalmology, Seoul National University College of Medicine, Seoul, Korea. resourceful@hanmail.net
- 2Department of Ophthalmology, Seoul National University Hospital, Seoul, Korea.
- 3Department of Ophthalmology, Seoul National University Bundang Hospital, Seongnam, Korea.
- 4Department of Pathology, Seoul National University Bundang Hospital, Seongnam, Korea.
- 5Department of Ophthalmology, Seoul Metropolitan Government-Seoul National University Boramae Medical Center, Seoul, Korea.
- KMID: 2215863
- DOI: http://doi.org/10.3341/jkos.2012.53.7.1023
Abstract
- PURPOSE
To report a case of syringocystadenoma papilliferum that presented as an eyelid nodule.
CASE SUMMARY
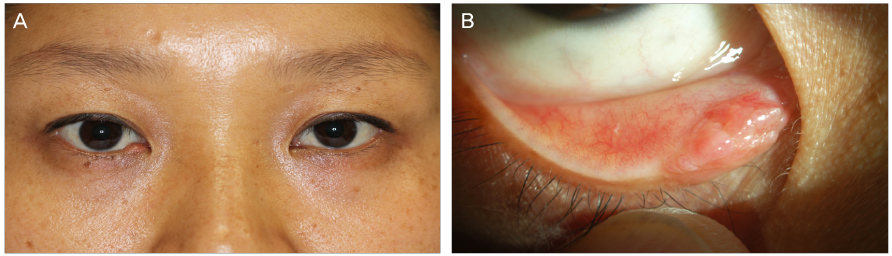
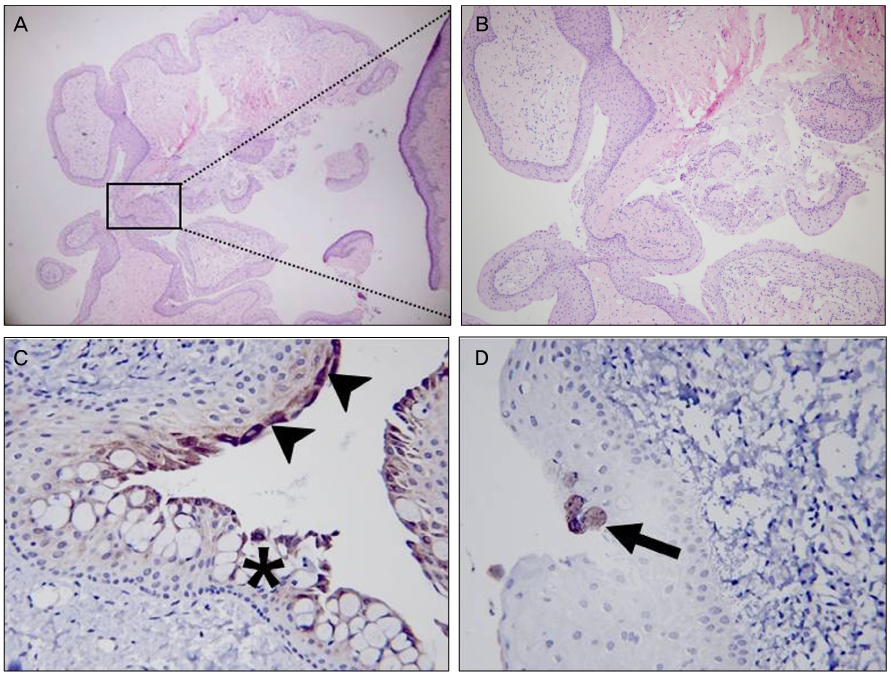
A 37-year-old woman presented with a mass around the punctum in the right lower eyelid margin, which had developed several years earlier and was increasing in size. The mass was a light pinkish nodule consisting of a few smooth-surface papillary lobules. The pathologic findings of the specimen obtained from a shaving biopsy showed a papillary projection which was covered with epithelium and communication with duct-like structures showing glandular configuration in the deep portion of the lesion. EMA-positive cells were found at the invaginated epithelium, implying a glandular epithelial origin. GCDFP-15-positive cells were found in the deep portion of the lesion, implying apocrine differentiation. The findings were compatible with syringocystadenoma papilliferum.
CONCLUSIONS
Syringocystadenoma papilliferum should be considered as a differential diagnosis of a solitary eyelid tumor.
Figure
Reference
-
1. Barbarino S, McCormick SA, Lauer SA, Milman T. Syringocystadenoma papilliferum of the eyelid. Ophthal Plast Reconstr Surg. 2009. 25:185–188.2. Jakobiec FA, Streeten BW, Iwamoto T, et al. Syringocystadenoma papilliferum of the eyelid. Ophthalmology. 1981. 88:1175–1181.3. Mammino JJ, Vidmar DA. Syringocystadenoma papilliferum. Int J Dermatol. 1991. 30:763–766.4. Stokes JH. A clinico-pathologic study of an unusual cutaneous neoplasm combining naevus syringadenomatous papilliferus and a granuloma. J Cutan Dis. 1917. 35:411–425.5. Helmi A, Alaraj AM, Alkatan H. Report of 3 histopathologically documented cases of syringocystadenoma papilliferum involving the eyelid. Can J Ophthalmol. 2011. 46:287–289.6. Feuerstein RC, Mims LC. Linear nevus sebaceus with convulsions and mental retardation. Am J Dis Child. 1962. 104:675–679.7. Jancar J. Naevus syringocystadenomatosus papilliferus with skull and brain lesions, hemiparesis, epilepsy and mental retardation. Br J Dermatol. 1970. 82:402–405.8. Helwig EB, Hackney VC. Syringadenoma papilliferum; lesions with and without naevus sebaceous and basal cell carcinoma. AMA Arch Derm. 1955. 71:361–372.9. Shams PN, Hardy TG, El-Bahrawy M, Joshi N. Syringocystadenoma papilliferum of the eyelid in a young girl. Ophthal Plast Reconstr Surg. 2006. 22:67–69.10. Yoon DH, Jang IG, Kim TY, et al. Syringocystadenoma papilliferum, basal cell carcinoma and trichilemmoma arising from nevus sebaceus of Jadassohn. Acta Derm Venereol. 1997. 77:242–243.11. Hsu PJ, Liu CH, Huang CJ. Mixed tubulopapillary hidradenoma and syringocystadenoma papilliferum occurring as a verrucous tumor. J Cutan Pathol. 2003. 30:206–210.12. Ishida-Yamamoto A, Sato K, Wada T, et al. Syringocystadenocarcinoma papilliferum: case report and immunohistochemical comparison with its benign counterpart. J Am Acad Dermatol. 2001. 45:755–759.13. Yamamoto O, Doi Y, Hamada T, et al. An immunohistochemical and ultrastructural study of syringocystadenoma papilliferum. Br J Dermatol. 2002. 147:936–945.14. Nowak M, Pathan A, Fatteh S, et al. Syringocystadenoma papilliferum of the male breast. Am J Dermatopathol. 1998. 20:422–424.15. Coyne JD, Fitzgibbon JF. Mixed syringocystadenoma papilliferum and papillary eccrine adenoma occurring in a scrotal condyloma. J Cutan Pathol. 2000. 27:199–201.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Syringocystadenoma Papilliferum in the Medial Canthus of an Eyelid
- Syringocystadenoma Papilliferum of the Ankle
- A Case of Linear Syringocystadenoma Papilliferum on the Inguinal Area
- Syringocystadenoma Papilliferum Giganteum: Report of A Case
- Syringocystadenoma Papilliferum: Unusual Location and Electron Microscopic Study