J Korean Ophthalmol Soc.
2012 Jul;53(7):918-923. 10.3341/jkos.2012.53.7.918.
Clinical Features and Treatment of Peripunctal Tumors
- Affiliations
-
- 1Department of Ophthalmology, Dong-A University, College of Medicine, Busan, Korea. hbahn@dau.ac.kr
- 2Dong-A University Medical Center Regional Clinical Trial Center, Busan, Korea.
- KMID: 2215847
- DOI: http://doi.org/10.3341/jkos.2012.53.7.918
Abstract
- PURPOSE
To investigate the clinical features and treatment results in peripunctal tumors.
METHODS
A retrospective medical record review was conducted on patients that were clinically diagnosed with peripunctal tumor from October 2005 to June 2011 in Dong-A University Hospital.
RESULTS
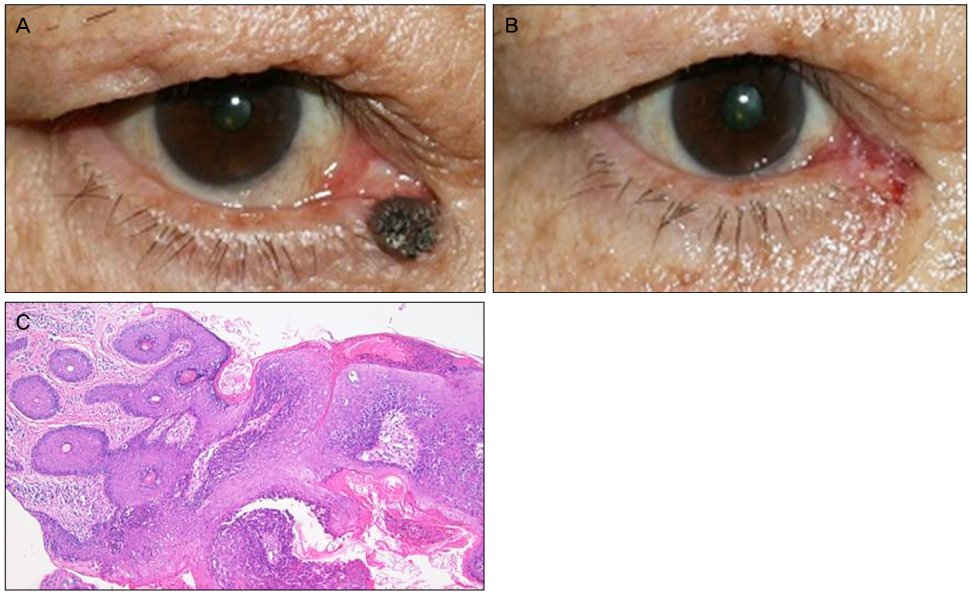
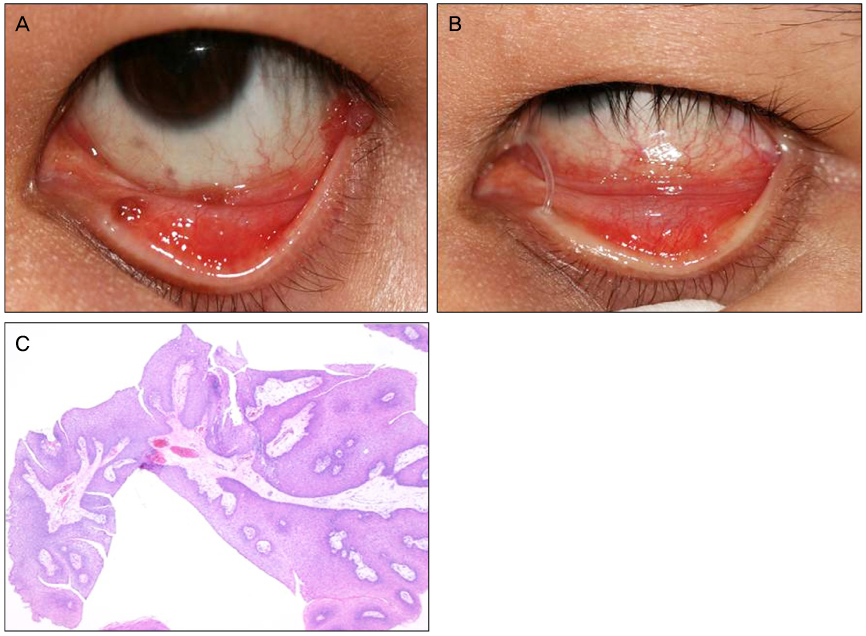
Twenty nine peripunctal tumors were identified. Five cases (17.2%) were involving upper eyelid and 22 cases (75.9%) were involving lower eyelid. Two cases (6.9%) were involving both upper and lower eyelid, which one of them were involving the conjunctiva as well. One of the patients (3.5%), underwent simple observation without surgery. Simple surgical resection and biopsy were performed in 7 cases (24.1%), and additional silicone tube intubation or Minimonoka insertion were carried-out in 21 cases (72.4%). Histology revealed 15 cases (53.6%) of melanocytic nevus, 5 cases (17.9%) of basal cell carcinoma, 2 cases (7.1%) of seborrheic keratosis, and others including malignant melanoma, squamous papilloma, epidermal cyst, and et cetra.
CONCLUSIONS
In conclusion, Peripunctal tumors are mostly found on the lower lids and, they are surgical resection and biopsy should be considered in all cases of peripunctal tumors since they have a potential for spreading to the lacrimal system. It is advised to perform a silicone tube intubation or minimonoka insertion along with the surgical excision to preserve the function of the punctum.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
A Lacrimal Punctal Keratinizing Cyst of the Lower Lid
Tae-Seen Kang, Yeon-Hee Lee, Sung Bok Lee
J Korean Ophthalmol Soc. 2019;60(7):692-695. doi: 10.3341/jkos.2019.60.7.692.
Reference
-
1. Annual report of the Giza Memorial Ophthalmic Laboratory, Annual Report 5. 1931. Cairo, Egypt: Schindler Press;35.2. Khan JA, Grove AS Jr, Joseph MP, et al. Sebaceous carcinoma, Diuretic use, lacrimal system spread, and surgical margins. Ophthal Plast Reconstr Surg. 1989. 5:227–234.3. Morel X, Meyer A, Le Rouic JF, et al. [Nevus mimicking a basal cell carcinoma of the eyelid]. J Fr Ophtalmol. 2002. 25:657–660. (Article in French).4. Pe'er J, Neufeld M, Ilsar M. Peripunctal eyelid oncocytoma. Am J Ophthalmol. 1993. 116:385–387.5. Scott KR, Jakobiec FA, Font RL. Peripunctal melanocytic nevi. Distinctive clinical findings and differential diagnosis. Ophthalmology. 1989. 96:994–998.6. Vrabec J. [Naevus puncti lacrimalis]. Sb Lek. 1966. 68:274–278.7. Imaizumi M, Nakatsuka K. Oncocytoma of the peripunctum. Int Ophthalmol. 2005. 26:111–113.8. Rumelt S, Pe'er J, Rubin PA. The clinicopathological spectrum of benign peripunctal tumours. Graefes Arch Clin Exp Ophthalmol. 2005. 243:113–119.9. Welch RB, Duke JR. Lesions of the lids; a statistical note. Am J Ophthalmol. 1958. 45:415–426.10. Aurora AL, Blodi FC. Reappraisal of basal cell carcinoma of the eyelids. Am J Ophthalmol. 1970. 70:329–336.11. Tesluk GC. Eyelid lesions: incidence and comparison of benign and malignant lesions. Ann Ophthalmol. 1985. 17:704–707.12. Folberg R, Jakobiec FA, Bernardino VB, Iwamoto T. Benign conjunctival melanocytic lesions. Clinicopathologic features. Ophthalmology. 1989. 96:436–461.13. Kersten RC, Ewing-Chow D, Kulwin DR, et al. Accuracy of clinical diagnosis of cutaneous eyelid lesions. Ophthalmology. 1997. 104:479–484.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Fetal tumors: prenatal ultrasonographic findings and clinical characteristics
- Sonographic Features of Phyllodes Tumors of the Breast: A Pictorial Review
- Histopathologic Resemblance of Ovarian Dermoid Cyst to Various Skin Tumors
- Mesenchymal Tumors of the Breast: Imaging and the Histopathologic Correlation
- Clinical and Histopathological Correlations of Phyllodes Tumors of the Breast