J Korean Ophthalmol Soc.
2015 Apr;56(4):521-531. 10.3341/jkos.2015.56.4.521.
Protective Effect of Preoperative Intraocular Pressure Reduction on Corneal Endothelium in Cataract Surgery
- Affiliations
-
- 1Department of Ophthalmology and Visual Science, The Catholic University of Korea College of Medicine, Seoul, Korea. yangkyeung@hanmail.net
- KMID: 2215702
- DOI: http://doi.org/10.3341/jkos.2015.56.4.521
Abstract
- PURPOSE
To evaluate whether intraocular pressure reduction by intravenous injection of mannitol before phacoemulsification-cataract surgery can have a protective effect on corneal endothelium.
METHODS
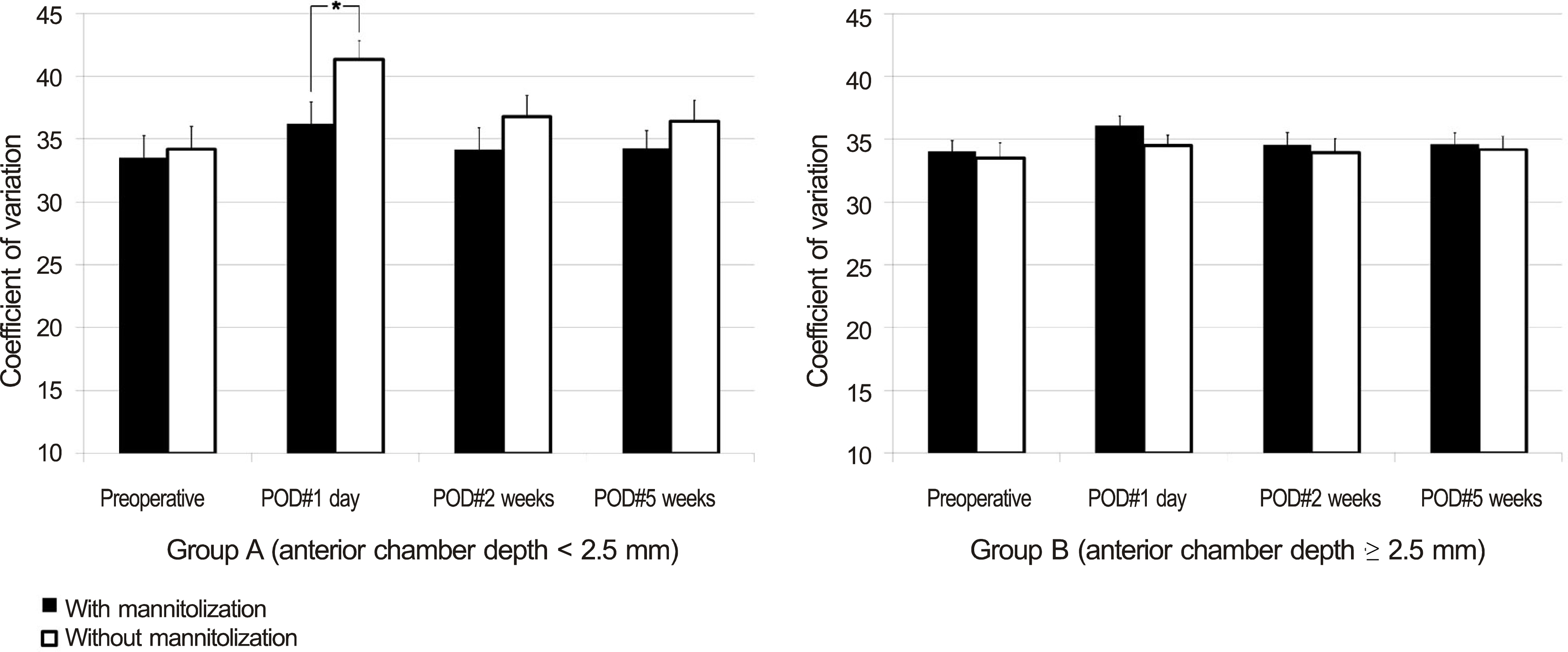
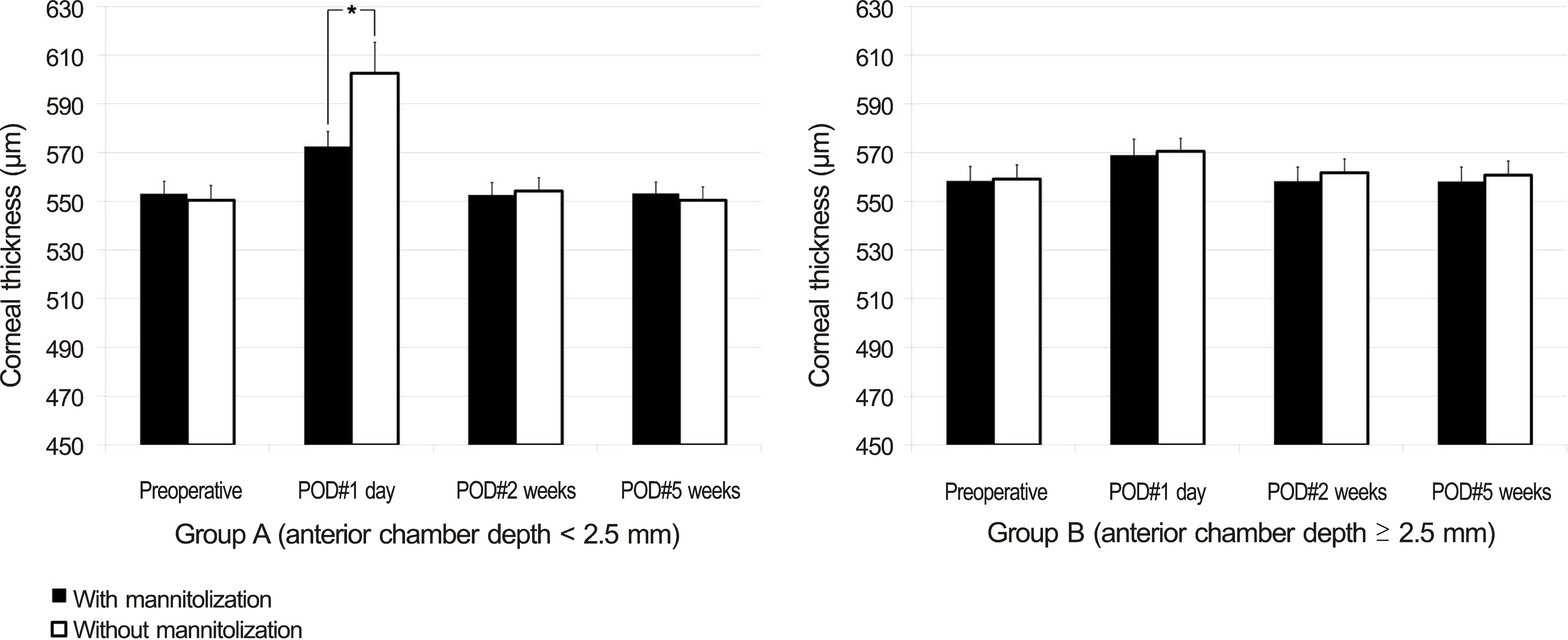
Patients undergoing sequential bilateral cataract surgery were divided into 2 groups, 36 eyes with anterior chamber depth (ACD) < 2.50 mm (group A) and 44 eyes with ACD > or = 2.50 mm (group B). In each group, preoperative intravenous injection of mannitol was performed in 1 randomly selected eye of the patient. The specular microscopic examination including cell density (ECD), coefficient of variation (CV), hexagonality (HA) of corneal endothelium, and corneal thickness was performed on postoperative 1 day, 2 weeks, and 5 weeks. In each group, the parameters were compared between the eyes with mannitolization and the contralateral eyes without mannitolization.
RESULTS
In group A, eyes with preoperative mannitolization showed significantly higher ECD at postoperative 1 day and 5 weeks and showed a significantly thinner cornea at postoperative 1 day than those without mannitolization (all p < 0.05). However, in group B, there was no significant difference of ECD, CV, HA, and corneal thickness between the eyes with and without mannitolization.
CONCLUSIONS
Preoperative intraocular pressure reduction by mannitolization before phacoemulsification can protect the corneal endothelial cells and recover the early postoperative period visual acuity in eyes with shallow anterior chamber.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Jung KI, Yang JW, Lee YC, Kim SY. Cataract surgery in eyes with nanophthalmos and relative anterior microphthalmos. Am J Ophthalmol. 2012; 153:1161–8.e1.
Article2. Nihalani BR, Jani UD, Vasavada AR, Auffarth GU. Cataract surgery in relative anterior microphthalmos. Ophthalmology. 2005; 112:1360–7.
Article3. Auffarth GU, Blum M, Faller U, et al. Relative anterior microphthalmos: morphometric analysis and its implications for cataract surgery. Ophthalmology. 2000; 107:1555–60.
Article4. Lee KM, Lee HS, Kim MS. Clinical results of phacoemulsification in eyes with acute angle-closure glaucoma in the aspect of complications. J Korean Ophthalmol Soc. 2009; 50:44–50.
Article5. Kirsch RE, Steinman W. Digital pressure, an important safeguard in cataract surgery. AMA Arch Ophthalmol. 1955; 54:697–703.
Article6. Davidson B, Kratz RP, Mazzocco TR, Maloney WF. An evaluation of the Honan intraocular pressure reducer. J Am Intraocul Implant Soc. 1979; 5:237.
Article7. Miettinen R, Airaksinen PJ, Pihlajaniemi R, Puhakka K. Preoperative timolol and ocular compression in cataract surgery. Acta Ophthalmol (Copenh). 1982; 60:622–7.
Article8. Robbins R, Blumenthal M, Galin MA. Reduction of vitreous weight by ocular massage. Am J Ophthalmol. 1970; 69:603–7.
Article9. Quist LH, Stapleton SS, McPherson SD Jr. Preoperative use of the Honan intraocular pressure reducer. Am J Ophthalmol. 1983; 95:536–8.
Article10. Chan FM, Lee L. Nanophthalmic cataract extraction. Clin Experiment Ophthalmol. 2004; 32:535–8.11. Jabs DA, Nussenblatt RB, Rosenbaum JT; Standardization of Uveitis Nomenclature (SUN) Working Group. Standardization of uveitis nomenclature for reporting clinical data. Results of the First International Workshop. Am J Ophthalmol. 2005; 140:509–16.12. Naumann GOH, Apple DJ. Pathologie des Auges. Berlin, Heidelberg: Springer-Verlag;1980.13. Weiss AH, Kousseff BG, Ross EA, Longbottom J. Simple microphthalmos. Arch Ophthalmol. 1989; 107:1625–30.
Article14. Weiss AH, Kousseff BG, Ross EA, Longbottom J. Complex microphthalmos. Arch Ophthalmol. 1989; 107:1619–24.
Article15. Parrishll RK, Donaldson K, Kairala MBM, Simmons RJ. Nanophthalmos, Relative Anterior Microphthalmos, and Axial Hyperopia. Steinert RF, editor. Cataract Surgery. 3rd ed.Philadelphia: Saunders;2010. chap. 33.16. Steijns D, Bijlsma WR, Van der Lelij A. Cataract surgery in patients with nanophthalmos. Ophthalmology. 2013; 120:266–70.
Article17. Wladis EJ, Gewirtz MB, Guo S. Cataract surgery in the small adult eye. Surv Ophthalmol. 2006; 51:153–61.
Article18. Faucher A, Hasanee K, Rootman DS. Phacoemulsification and intraocular lens implantation in nanophthalmic eyes: report of a me-dium-size series. J Cataract Refract Surg. 2002; 28:837–42.19. Hwang JH, Yeom DJ, Kim JS, Lee JH. A case of acute angle-clo-sure glaucoma in a nanophthalmos patient. J Korean Ophthalmol Soc. 2010; 51:303–6.
Article20. Brockhurst RJ. Cataract surgery in nanophthalmic eyes. Arch Ophthalmol. 1990; 108:965–7.
Article21. Mandal AK. Cataract surgery with primary posterior chamber intraocular lens implantation in nanophthalmos. Ophthalmic Surg Lasers. 2001; 32:333–5.
Article22. Kong M, Kim JH, Kim SJ, Kang SW. Full-thickness sclerotomy for uveal effusion syndrome. Korean J Ophthalmol. 2013; 27:294–8.
Article23. Lee JH, Choi JY, Kim SS. Two cases of uveal effusion syndrome. Korean J Ophthalmol. 2006; 20:124–7.
Article24. Allingham RR, Damji KF, Freedman SF, et al. Cholinergic Stimulators and Hyperosmotic Agents. Allingham RR, Damji KF, Freedman SF, editors. Shields Textbook of Glaucoma. 6th ed.Philadelphia: Lippincott Williams & Wilkins;2011. chap. 32.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effect of Premedication and Honan Balloon prior to Cataract Surgery on Intraocular Pressure measured by Tono-pen
- The Effect of Healon(R) and Metrol(R) on Cornea and Intraocular Pressure in Extracapsular Cataract Extraction with Posterior Chamber Lens Implantation
- Influence of Preoperative Corneal Endothelial Status on Postoperative Corneal Endothelium Density after Cataract Surgery
- Effect of Dorzolamide on Corneal Endothelium
- The Change of Intraocular Pressure after Extracapsular Cataract Extraction in Patients with Angle-closure Glaucoma