J Korean Ophthalmol Soc.
2012 Jan;53(1):27-36. 10.3341/jkos.2012.53.1.27.
Efficacy of the Sutureless Amniotic Membrane Patch for the Treatment of Ocular Surface Disorders
- Affiliations
-
- 1Department of Ophthalmology, Daegu Fatima Hospital, Daegu, Korea. djoph2540@yahoo.co.kr
- KMID: 2215242
- DOI: http://doi.org/10.3341/jkos.2012.53.1.27
Abstract
- PURPOSE
To evaluate the efficacy of the sutureless amniotic membrane (AM) patch for the treatment of ocular surface disorders.
METHODS
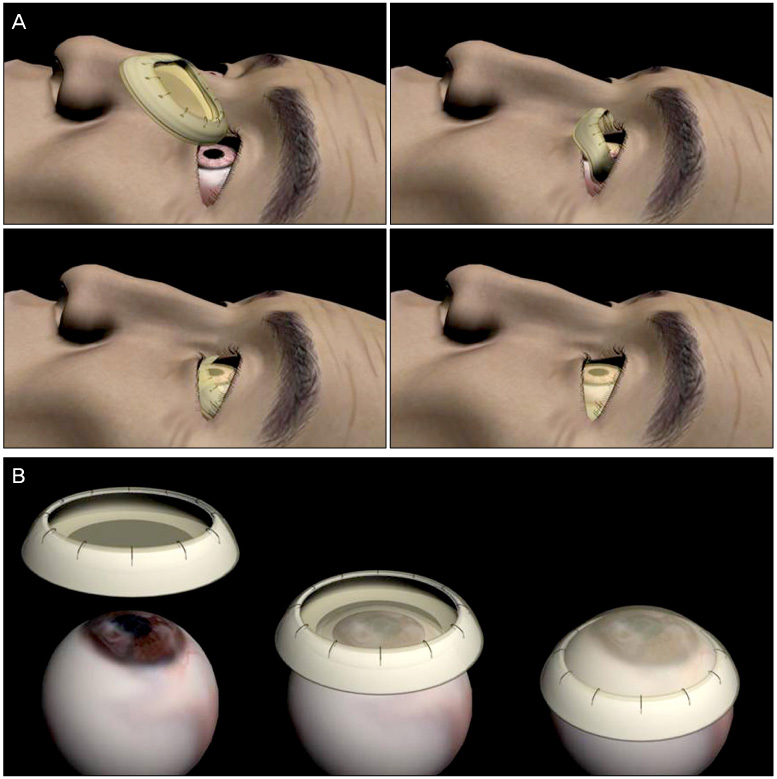
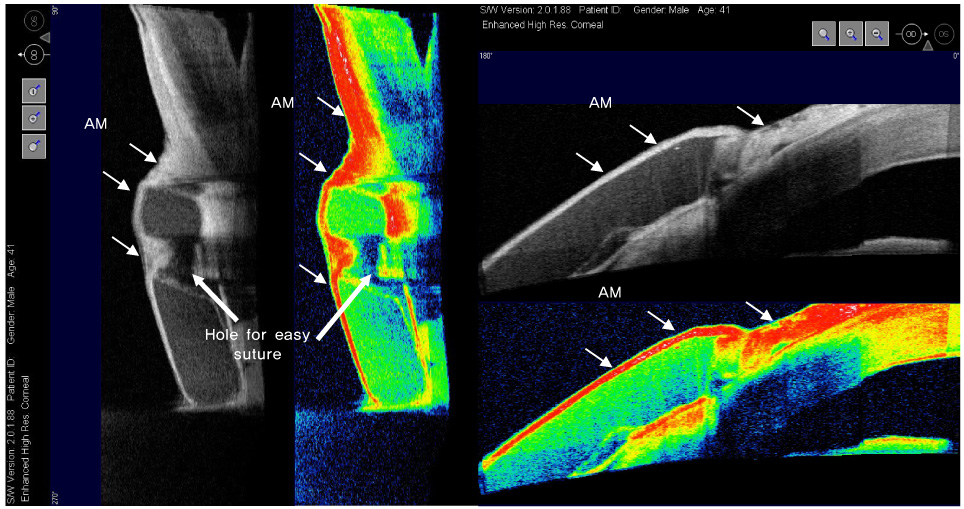
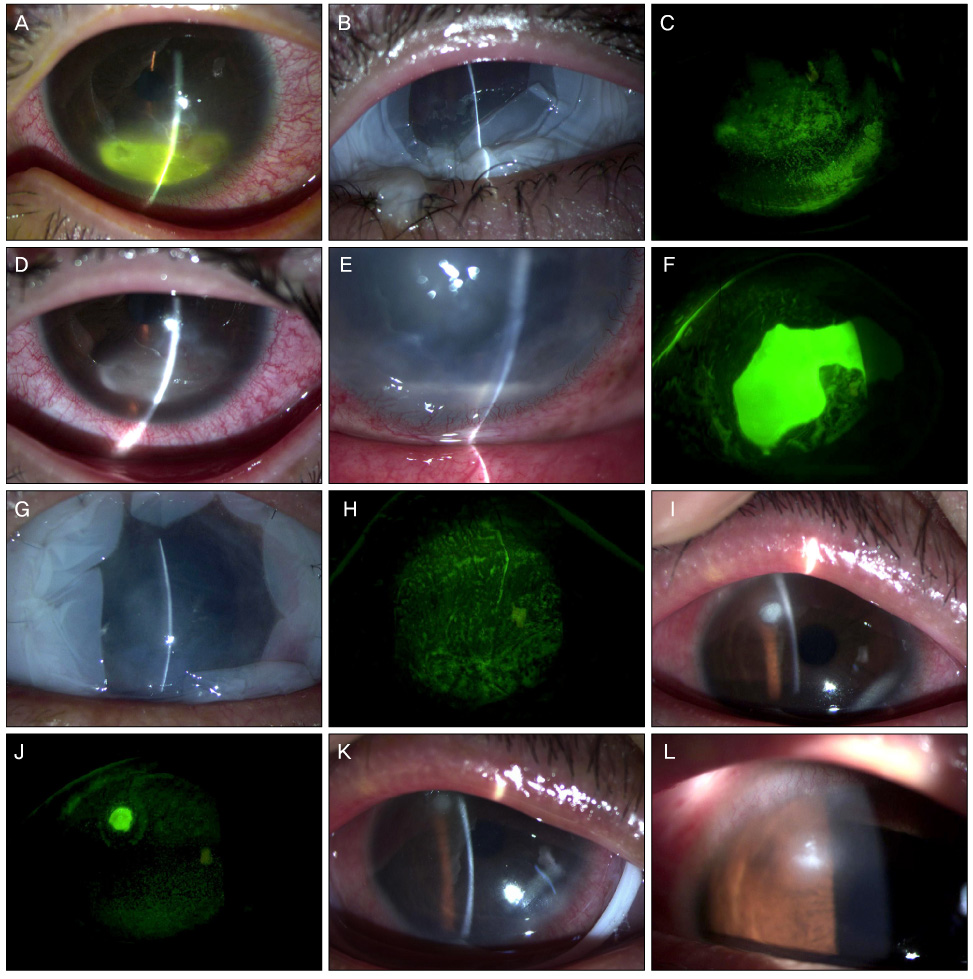
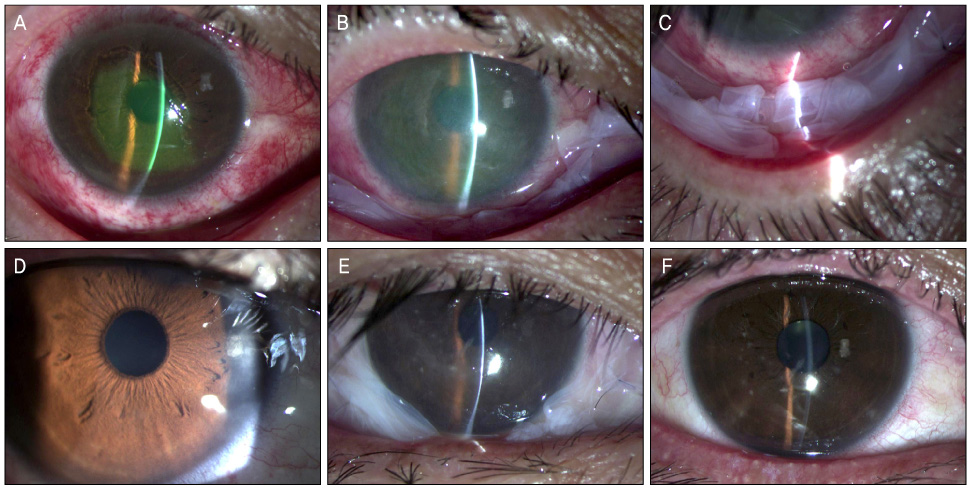
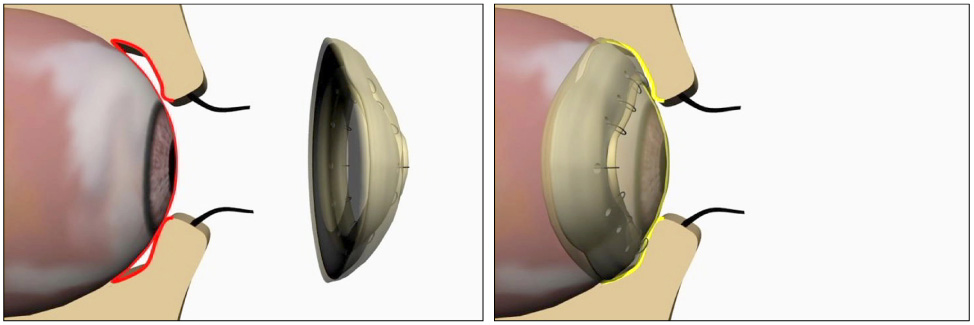
A sutureless AM patch using a silicone ring was utilized to treat neurotrophic ulcer, persistent epithelial defect (PED), Shield ulcer, chemical injury and Stevens-Johnson syndrome. Primary outcome was the time to complete corneal and conjunctival epithelialization. Secondary outcome was the number of repeated insertions and complications of the inserted ring.
RESULTS
Neurotrophic ulcer was observed in 4 eyes, PED in 2 eyes, Shield ulcer in 1 eye, chemical injury in 4 eyes and Stevens-Johnson syndrome in 4 eyes. The mean (SD) time to complete epithelialization was 13 (7.2) days (6-20 days) in neurotrophic ulcer, 17.5 (7.7) days (12-23) in PED, 5 days in Shield ulcer, 10.6 (6.6) days (3-15) in chemical injury and 13.5 (0.7) days (13-14) in Stevens-Johnson syndrome. There were no protrusion or mechanical trauma of the inserted ring. In 1 case of neurotrophic ulcer and 1 refractory case of chemical injury, repeated insertion was performed due to incomplete healing after dissolution of the AM. In 2 eyes with Stevens-Johnson syndrome, repeated insertion was necessary with heavy accumulation of inflammatory debris on the AM. No symblepharon or fornix contracture was found in chemical injury or Stevens-Johnson syndrome patients.
CONCLUSIONS
The sutureless AM patch using a silicone ring was shown to be effective and safe for the treatment of ocular surface disorders. The patch can help surgeons avoid suture-related trauma to the ocular surface during the acute inflammatory period.
Keyword
Figure
Reference
-
1. de Rötth A. Plastic repair of conjunctival defects with fetal membranes. Arch Ophthalmol. 1940. 23:522–525.2. Kim JC, Tseng SC. Transplantation of preserved human amniotic membrane for surface reconstruction in severely damaged rabbit corneas. Cornea. 1995. 14:473–484.3. Tseng SC, Prabhasawat P, Lee SH. Amniotic membrane transplantation for conjunctival surface reconstruction. Am J Ophthalmol. 1997. 124:765–774.4. Tsubota K, Satake Y, Ohyama M, et al. Surgical reconstruction of the ocular surface in advanced ocular cicatricial pemphigoid and Stevens-Johnson syndrome. Am J Ophthalmol. 1996. 122:38–52.5. Pires RT, Tseng SC, Prabhasawat P, et al. Amniotic membrane transplantation for symptomatic bullous keratopathy. Arch Ophthalmol. 1999. 117:1291–1297.6. Tseng SC, Prabhasawat P, Barton K, et al. Amniotic membrane transplantation with or without limbal allografts for corneal surface reconstruction in patients with limbal stem cell deficiency. Arch Ophthalmol. 1998. 116:431–441.7. Chun DH, Jeon SL, Lee JY, Choi TH. The effect of amniotic membrane transplantation on corneal epithelial cell proliferation. J Korean Ophthalmol Soc. 2002. 43:1746–1757.8. Shin KS, Chung IY, Seo SW. The effect of amniotic membrane transplantation for corneal ulcer and ocular surface diseases. J Korean Ophthalmol Soc. 2003. 44:1305–1310.9. Lee SH, Tseng SC. Amniotic membrane transplantation for persistent epithelial defects with ulceration. Am J Ophthalmol. 1997. 123:303–312.10. Kruse FE, Rohrschneider K, Völcker HE. Multilayer amniotic membrane transplantation for reconstruction of deep corneal ulcers. Ophthalmology. 1999. 106:1504–1510.11. Roper-Hall MJ. Thermal and chemical burns. Trans Ophthalmol Soc UK. 1965. 85:631–653.12. Kheirkhah A, Johnson DA, Paranipe DR, et al. Temporary sutureless amniotic membrane patch for acute alkaline burns. Arch Ophthalmol. 2008. 126:1059–1066.13. Pachigolla G, Prasher P, Di Pascuale MA, et al. Evaluation of the role of ProKera in the management of ocular surface and orbital disorders. Eye Contact Lens. 2009. 35:172–175.14. Sheha H, Liang L, Li J, Tseng SC. Sutureless amniotic membrane transplantation for severe bacterial keratitis. Cornea. 2009. 28:1118–1123.15. Shammas MC, Lai EC, Sarkar JS, et al. Management of acute Stevens-Johnson syndrome and toxic epidermal necrolysis utilizing amniotic membrane and topical corticosteroids. Am J Ophthalmol. 2010. 149:203–213.16. Shay E, Khadem JJ, Tseng SC. Efficacy and limitation of sutureless amniotic membrane transplantation for acute toxic epidermal necrolysis. Cornea. 2010. 29:359–361.17. Uçakhan OO, Köklü G, Firat E. Nonpreserved human amniotic membrane transplantation in acute and chronic chemical eye injuries. Cornea. 2002. 21:169–172.18. Kobayashi A, Shirao Y, Yoshita T, et al. Temporary amniotic membrane patching for acute chemical burns. Eye (Lond). 2003. 17:149–158.19. Arora R, Mehta D, Jain V. Amniotic membrane transplantation in acute chemical burns. Eye (Lond). 2005. 19:273–278.20. Tamhane A, Vajpayee RB, Biswas NR, et al. Evaluation of amniotic membrane transplantation as an adjunct to medical therapy as compared with medical therapy alone in acute ocular burns. Ophthalmology. 2005. 112:1963–1969.21. Prabhasawat P, Tesavibul N, Prakairungthong N, Booranapong W. Efficacy of amniotic membrane patching for acute chemical and thermal ocular burns. J Med Assoc Thai. 2007. 90:319–326.22. López-García JS, Rivas Jara L, García-Lozano I, Murube J. Histopathologic limbus evolution after alkaline burns. Cornea. 2007. 26:1043–1048.23. Joseph A, Dua HS, King AJ. Failure of amniotic membrane transplantation in the treatment of acute ocular burns. Br J Ophthalmol. 2001. 85:1065–1069.24. Mackie IA. Role of the corneal nerves in destructive disease of the cornea. Trans Ophthalmol Soc U K. 1978. 98:343–347.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Applications and Complications of Contact Lens Type Amniotic Membrane
- New Strategy of Ocular Surface Disease: Ocular Surface Reconstruction Using Amniotic Membrane and Limbal Stem Cell Transplantation
- Clinical Benefits of Amniotic Membrane Contact Lens
- Ocular Surface Reconstruction with Amniotic Membrane Transplantation in Pterygium
- A Novel Application of Amniotic Membrane in Patients with Bullous Keratopathy