J Korean Ophthalmol Soc.
2011 Jul;52(7):893-896. 10.3341/jkos.2011.52.7.893.
Acute Bilateral Visual Loss with Idiopathic Hypertrophic Pachymeningitis
- Affiliations
-
- 1Department of Ophthalmology, Chungnam National University College of Medicine, Daejeon, Korea. opticalyh@hanmail.net
- KMID: 2214718
- DOI: http://doi.org/10.3341/jkos.2011.52.7.893
Abstract
- PURPOSE
To report a case of bilateral optic neuropathy related with idiopathic hypertropic pachymeningitis.
CASE SUMMARY
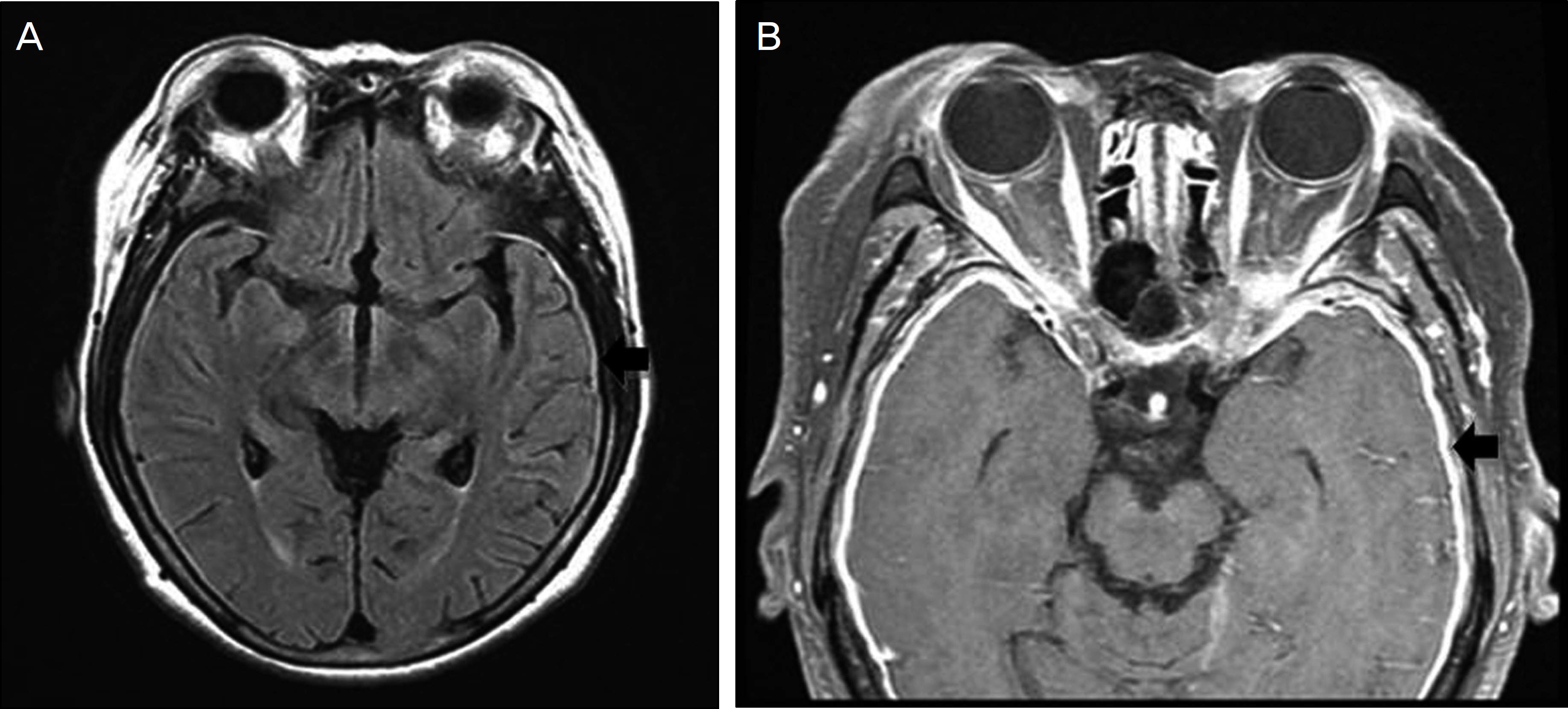
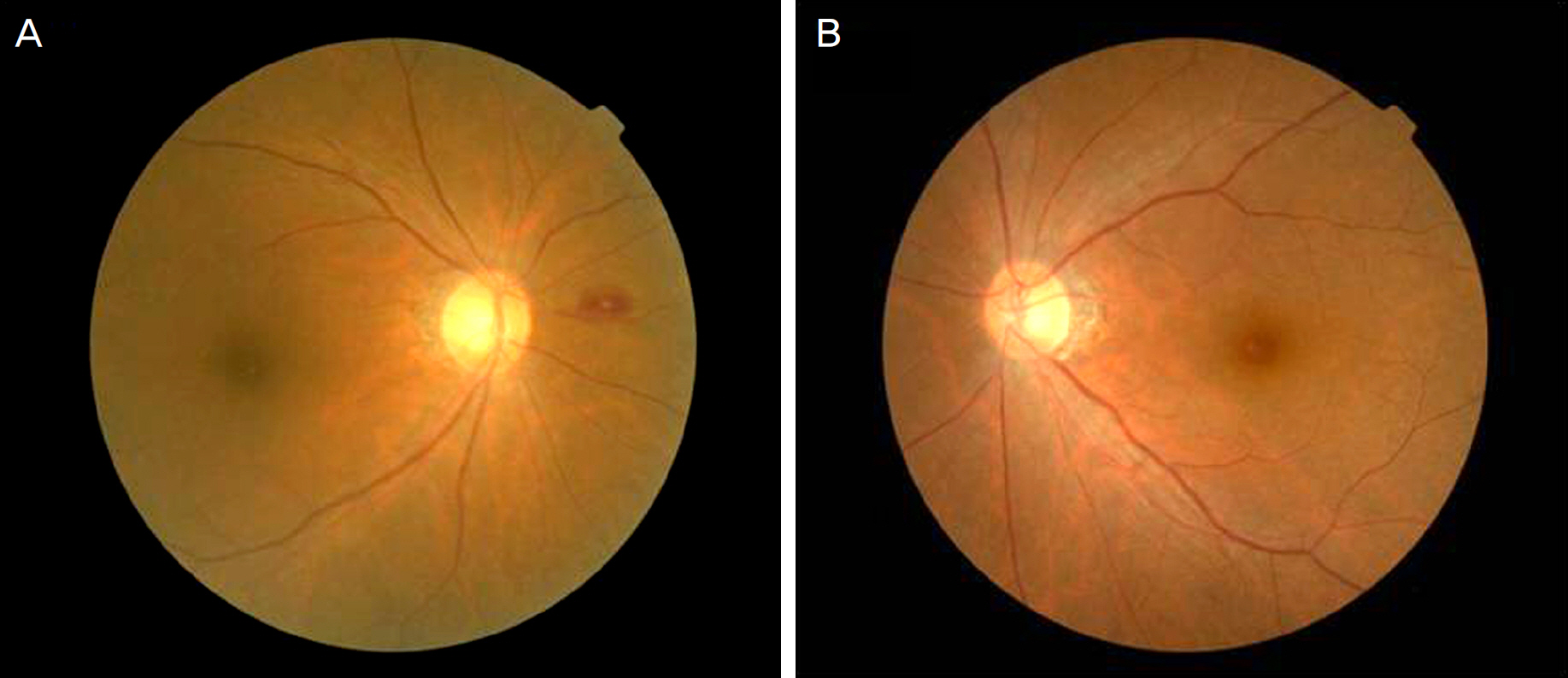
A 66-year old woman presented with acute visual loss that developed 6 days previously in the right eye and 3 days prior in the left eye. During the initial evaluation, her visual acuity was light perception in the right eye and counting fingers at 30 cm in the left eye. A relative afferent papillary defect (RAPD) was noted in the patient's right eye. On brain MRI, the duramater was thickened and enhanced by contrast. The erythrocyte Sedimentation Rate (ESR) and C-reactive protein (CRP) level were increased and myeloperoxidase-antineutrophil cytoplasmic antibody (MPO-ANCA) as positive. Other neurological and medical abnormalities were not found. Under the suspicion of bilateral optic neuropathy due to idiopathic hypertrophic pachymeningitis, the patient was treated with methylprednisolone pulse therapy. Two days after the treatment, the visual acuity was hand movements at 20 cm in the right eye and 0.6 in the left eye. Three months after the treatment, the visual acuity was counting fingers at 20 cm in the right eye, and 0.7 in the left eye. The right eye showed optic disc pallor and diffuse retinal nerve fiber layer (RNFL) defect. The left eye showed a suspicious RNFL defect, and was otherwise normal.
CONCLUSIONS
The authors report a rare case of optic neuropathy related with idiopathic hypertrophic pachymeningitis. Idiopathic hypertrophic pachymeningitis should be considered as one of the various causes of optic neuropathy.
MeSH Terms
Figure
Reference
-
References
1. Victor M, Ropper AH. Disturbances of cerebrospinal fluid and its circulation including hydrocephalus, pseudotumor cerebri, and low pressure syndromes. Victor M, Ropper AH, editors. Principles of Neurology. 7th ed.New York: McGraw-Hill;2001. p. 673.2. Hatano N, Behari S, Nagatani T, et al. Idiopathic hypertrophic cranial pachymeningitis: clinicoradiological spectrum and therapeutic options. Neurosurgery. 1999; 45:1336–42. discussion 1342–4.
Article3. Goyal M, Malik A, Mishra NK, Gaikwad SB. Idiopathic hypertrophic pachymeningitis: spectrum of the disease. Neuroradiology. 1997; 39:619–23.
Article4. Phanthumchinda K, Sinsawaiwong S, Hemachudha T, Yodnophaklao P. Idiopathic hypertrophic cranial pachymeningitis: an unusual cause of subacute and chronic headache. Headache. 1997; 37:249–52.
Article5. Masson C, Hénin D, Hauw JJ, et al. Cranial pachymeningitis of unknown origin: a study of seven cases. Neurology. 1993; 43:1329–34.6. Harada T, Ohashi T, Ohki K, et al. Optic neuropathy associated with hypertrophic cranial pachymeningitis. Br J Ophthalmol. 1996; 80:574–5.
Article7. Rojana-udomsart A, Pulkes T, Viranuwatti K, et al. Idiopathic hypertrophic cranial pachymeningitis. J Clin Neurosci. 2008; 15:465–9.
Article8. Liewluck T, Schatz NJ, Potter PF, Romaguera RL. Compressive retrobulbar optic neuropathy due to hypertrophic pachymeningitis. Intern Med. 2008; 47:1761–2.
Article9. Pareja-Esteban J, Gutiérrez-Solana S, Cedazo M, et al. Hypertrophic pachymeningitis and ophthalmological disturbances: description of two case reports. Arch Soc Esp Oftalmol. 2008; 83:497–500.10. Kim EJ, Kim JM, Yoo JM. Right superior oblique paralysis associated with idopathic hypertropic cranial pachymeningitis. J Korean Ophthalmol Soc. 2006; 47:332–7.11. Miwa H, Koshimura I, Mizuno Y. Recurrent cranial neuropathy as a clinical presentation of idiopathic inflammation of the dura mater: a possible relationship to Tolosa-Hunt syndrome and cranial pachymeningitis. J Neurol Sci. 1998; 154:101–5.
Article12. Moura FC, Pereira IC, Gonçalves AC, et al. Cranial idiopathic hypertrophic pachymeningitis associated with orbital pseudotumor: case report. Arq Neuropsiquiatr. 2005; 63:885–8.13. Schönermarck U, Lamprecht P, Csernok E, Gross WL. Prevalence and spectrum of rheumatic diseases associated with proteinase 3-antineutrophil cytoplasmic antibodies (ANCA) and myeloper-oxidase-ANCA. Rheumatology. 2001; 40:178–84.
Article14. Akahoshi M, Yoshimoto G, Nakashima H, et al. MPO-ANCA-positive Wegener's granulomatosis presenting with hypertrophic cranial pachymeningitis: case report and review of the literature. Mod Rheumatol. 2004; 14:179–83.
Article15. Choi IS, Park SC, Jung YK, Lee SS. Combined therapy of corticosteroid and azathioprine in hypertrophic cranial pachymeningitis. Eur Neurol. 2000; 44:193–8.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Idiopathic Hypertrophic Cranial Pachymeningitis: Case Report
- Rapid Recurrence of Spinal Idiopathic Hypertrophic Pachymeningitis: A Case Report
- Gait Imbalance as the Initial Presentation of Idiopathic Hypertrophic Pachymeningitis
- Two Cases of Perinuclear Anti-neutrophil Cytoplastic Antibodies Associated Hypertrophic Pachymeningitis Presented with Visual Loss
- An Idiopathic Hypertrophic Tentorial Pachymeningitis Presented as an Alternating Recurrent Painful Ophthalmoplegia