J Korean Ophthalmol Soc.
2015 Oct;56(10):1558-1565. 10.3341/jkos.2015.56.10.1558.
Comparison of Ocular Biometry Using Low-Coherence Reflectometry with Other Devices for Intraocular Lens Power Calculation
- Affiliations
-
- 1The Institute of Vision Research, Department of Ophthalmology, Yonsei University College of Medicine, Seoul, Korea. taeimkim@gmail.com
- 2Department of Ophthalmology, International St. Mary's Hospital, Catholic Kwandong University College of Medicine, Incheon, Korea.
- 3Department of Ophthalmology, Inha University School of Medicine, Incheon, Korea.
- 4Myung-Gok Eye Research Institute, Kim's Eye Hospital, Konyang University College of Medicine, Seoul, Korea.
- KMID: 2214415
- DOI: http://doi.org/10.3341/jkos.2015.56.10.1558
Abstract
- PURPOSE
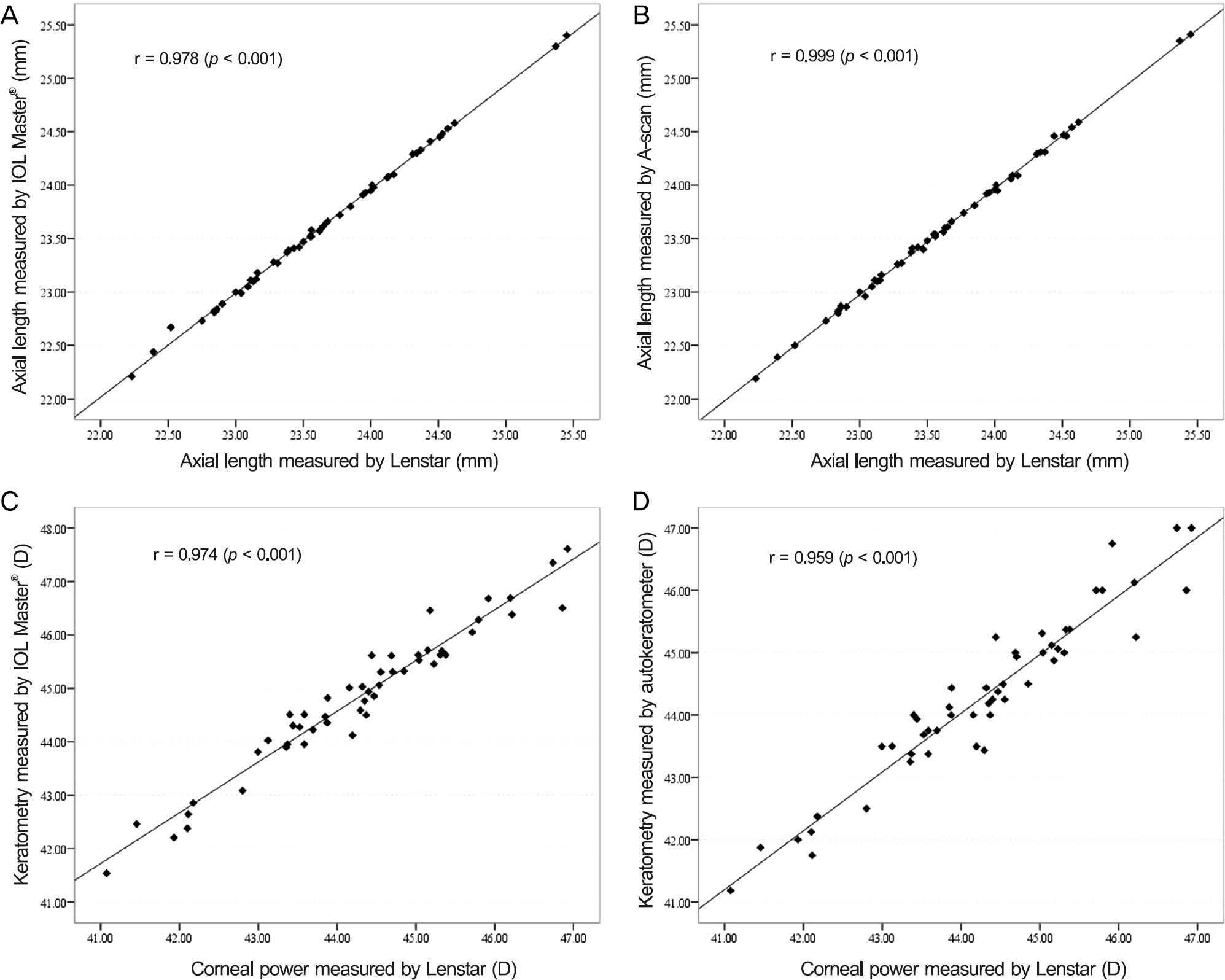
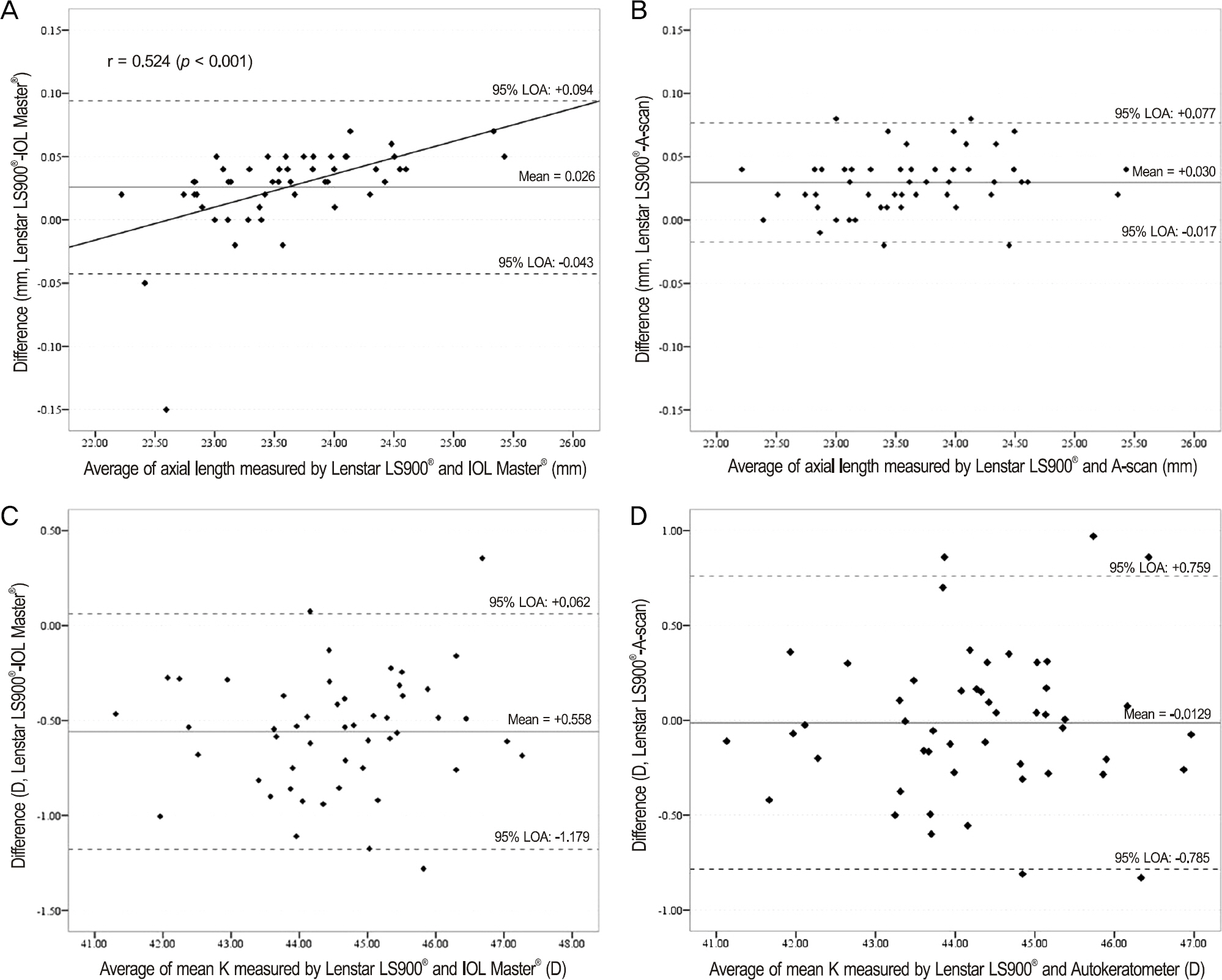
To compare axial length (AL) and keratometry (K) using optical low-coherence reflectometry (OLCR, Lenstar LS900(R), Haag-Streit, Bern, Switzerland) with current ocular biometry devices and evaluate the accuracy of intraocular lens (IOL) power calculation.
METHODS
In this prospective, comparative observational study of eyes with cataracts, AL and K were measured using an OLCR device (Lenstar LS900(R), Haag-Streit), partial coherence interferometry (PCI, IOL Master(R), Carl Zeiss, Jena, Germany), A-scan (Eyecubed) and automated keratometry (KR-7100, Topcon, Tokyo, Japan). IOL power calculation was performed using the Sanders-Retzlaff-Kraff (SRK/T) formula. The IOL prediction error (PE) was calculated by subtracting the predicted IOL power from the postoperative (PO) IOL power (PO 4 weeks, PO 12 weeks).
RESULTS
A total of 50 eyes of 39 patients with cataracts (mean age 67.12 +/- 8.51 years) were evaluated in this study. AL and K were not significantly different between the OLCR device and other devices (analysis of variance [ANOVA], p = 0.946, 0.062, respectively). The mean PE in IOL power calculation was -0.22 +/- 0.50D with the OLCR device, 0.08 +/- 0.45D with the PCI device and -0.01 +/- 0.48D with A-scan and automated keratometry (ANOVA, p = 0.006). The highest percentage of eyes with PE smaller than +/- 0.5D was IOL Master(R) followed by Eyecubed and then Lenstar LS900(R). The mean absolute PE was not statistically significant among the 3 devices (ANOVA, p = 0.684).
CONCLUSIONS
Ocular biometry measurements were comparable between the OLCR device and the PCI ultrasound device. However, the IOL power prediction showed significant differences among the 3 devices. Therefore, the differences in application of these devices should be considered.
Keyword
MeSH Terms
Figure
Cited by 2 articles
-
Comparison of Ocular Biometry Measurements Using A-Scan Ultrasound and Two Types of Partial Coherence Interferometers
Dae Young Ha, Kang Won Lee, Ji Won Jung
J Korean Ophthalmol Soc. 2016;57(5):757-762. doi: 10.3341/jkos.2016.57.5.757.Comparison of Axial Length and Postoperative Refraction between Applanation Ultrasonography and Low-coherence Reflectometry
Yoon Pyo Lee, Young Joo Shin, Kayoung Yi
J Korean Ophthalmol Soc. 2018;59(7):629-636. doi: 10.3341/jkos.2018.59.7.629.
Reference
-
References
1. Santodomingo-Rubido J, Mallen EA, Gilmartin B, Wolffsohn JS. A new non-contact optical device for ocular biometry. Br J Ophthalmol. 2002; 86:458–62.
Article2. Hill W, Angeles R, Otani T. Evaluation of a new IOLMaster algo-rithm to measure axial length. J Cataract Refract Surg. 2008; 34:920–4.
Article3. Drexler W, Findl O, Menapace R. . Partial coherence inter-ferometry: a novel approach to biometry in cataract surgery. Am J Ophthalmol. 1998; 126:524–34.
Article4. Lam AK, Chan R, Pang PC. The repeatability and accuracy of axial length and anterior chamber depth measurements from the IOLMaster. Ophthalmic Physiol Opt. 2001; 21:477–83.5. Haigis W, Lege B, Miller N, Schneider B. Comparison of im-mersion ultrasound biometry and partial coherence interferometry for intraocular lens calculation according to Haigis. Graefes Arch Clin Exp Ophthalmol. 2000; 238:765–73.
Article6. Buckhurst PJ, Wolffsohn JS, Shah S. . A new optical low co-herence reflectometry device for ocular biometry in cataract patients. Br J Ophthalmol. 2009; 93:949–53.
Article7. Rohrer K, Frueh BE, Wälti R. . Comparison and evaluation of ocular biometry using a new noncontact optical low-coherence reflectometer. Ophthalmology. 2009; 116:2087–92.
Article8. Zhao J, Chen Z, Zhou Z. . Evaluation of the repeatability of the Lenstar and comparison with two other non-contact biometric de-vices in myopes. Clin Exp Optom. 2013; 96:92–9.
Article9. Chen YA, Hirnschall N, Findl O. Evaluation of 2 new optical bio-metry devices and comparison with the current gold standard biometer. J Cataract Refract Surg. 2011; 37:513–7.
Article10. Hoffer KJ, Shammas HJ, Savini G. Comparison of 2 laser instru-ments for measuring axial length. J Cataract Refract Surg. 2010; 36:644–8.
Article11. Holzer MP, Mamusa M, Auffarth GU. Accuracy of a new partial coherence interferometry analyser for biometric measurements. Br J Ophthalmol. 2009; 93:807–10.
Article12. Retzlaff JA, Sanders DR, Kraff MC. Development of the SRK/T intraocular lens implant power calculation formula. J Cataract Refract Surg. 1990; 16:333–40.
Article13. Jasvinder S, Khang TF, Sarinder KK. . Agreement analysis of LENSTAR with other techniques of biometry. Eye (Lond). 2011; 25:717–24.
Article14. Salouti R, Nowroozzadeh MH, Zamani M. . Comparison of the ultrasonographic method with 2 partial coherence interferometry methods for intraocular lens power calculation. Optometry. 2011; 82:140–7.
Article15. Shin JW, Seong M, Kang MH. . Comparison of ocular bio-metry and postoperative refraction in cataract patients between Lenstar(R) and IOL Master(R). J Korean Ophthalmol Soc. 2012; 53:833–8.16. Mehravaran S, Asgari S, Bigdeli S. . Keratometry with five dif-ferent techniques: a study of device repeatability and inter-device agreement. Int Ophthalmol. 2014; 34:869–75.
Article17. Huynh SC, Mai TQ, Kifley A. . An evaluation of keratometry in 6-year-old children. Cornea. 2006; 25:383–7.
Article18. Whang WJ, Byun YS, Joo CK. Comparison of refractive outcomes using five devices for the assessment of preoperative corneal power. Clin Experiment Ophthalmol. 2012; 40:425–32.
Article19. Carney LG, Mainstone JC, Henderson BA. Corneal topography and myopia. A cross-sectional study. Invest Ophthalmol Vis Sci. 1997; 38:311–20.20. Speicher L. Intra-ocular lens calculation status after corneal re-fractive surgery. Curr Opin Ophthalmol. 2001; 12:17–29.
Article21. Bjeloš Ronč ević M, Bušić M, Cima I. . Intraobserver and inter-observer repeatability of ocular components measurement in cata-ract eyes using a new optical low coherence reflectometer. Graefes Arch Clin Exp Ophthalmol. 2011; 249:83–7.
Article22. Stattin M, Zehetner C, Bechrakis NE, Speicher L. Comparison of IOL-Master 500 vs. Lenstar LS900 concerning the calculation of target refraction: a retrospective analysis. Ophthalmologe. 2015; 112:444–50.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of Ocular Biometry and Postoperative Refraction in Cataract Patients Between Lenstar(R) and IOL Master(R)
- Comparison of the Accuracies of Intraocular Lens Power Formulae by the Type of Implanted Lens
- Comparison of Biometric Measurements and Refractive Results among Low-coherence Reflectometry, Partial Interferometry and Applanation Ultrasonography
- Comparison of Ocular Biometry Measurements Using A-Scan Ultrasound and Two Types of Partial Coherence Interferometers
- Comparison of Ocular Biometric Measurements Using New Swept-source Optical-coherence Tomography, Low-coherence Reflectometry, A-Scan Biometry, and Autokeratometry