J Korean Ophthalmol Soc.
2010 Nov;51(11):1543-1547. 10.3341/jkos.2010.51.11.1543.
A Case of Complete Recovery of Visual Loss Associated With Electroconvulsive Therapy
- Affiliations
-
- 1Department of Ophthalmology, Maryknoll Medical Center, Busan, Korea. kris9352@daum.net
- KMID: 2213994
- DOI: http://doi.org/10.3341/jkos.2010.51.11.1543
Abstract
- PURPOSE
To report a case of complete recovery within 1 day of cortical blindness associated with electroconvulsive therapy (ECT).
CASE SUMMARY
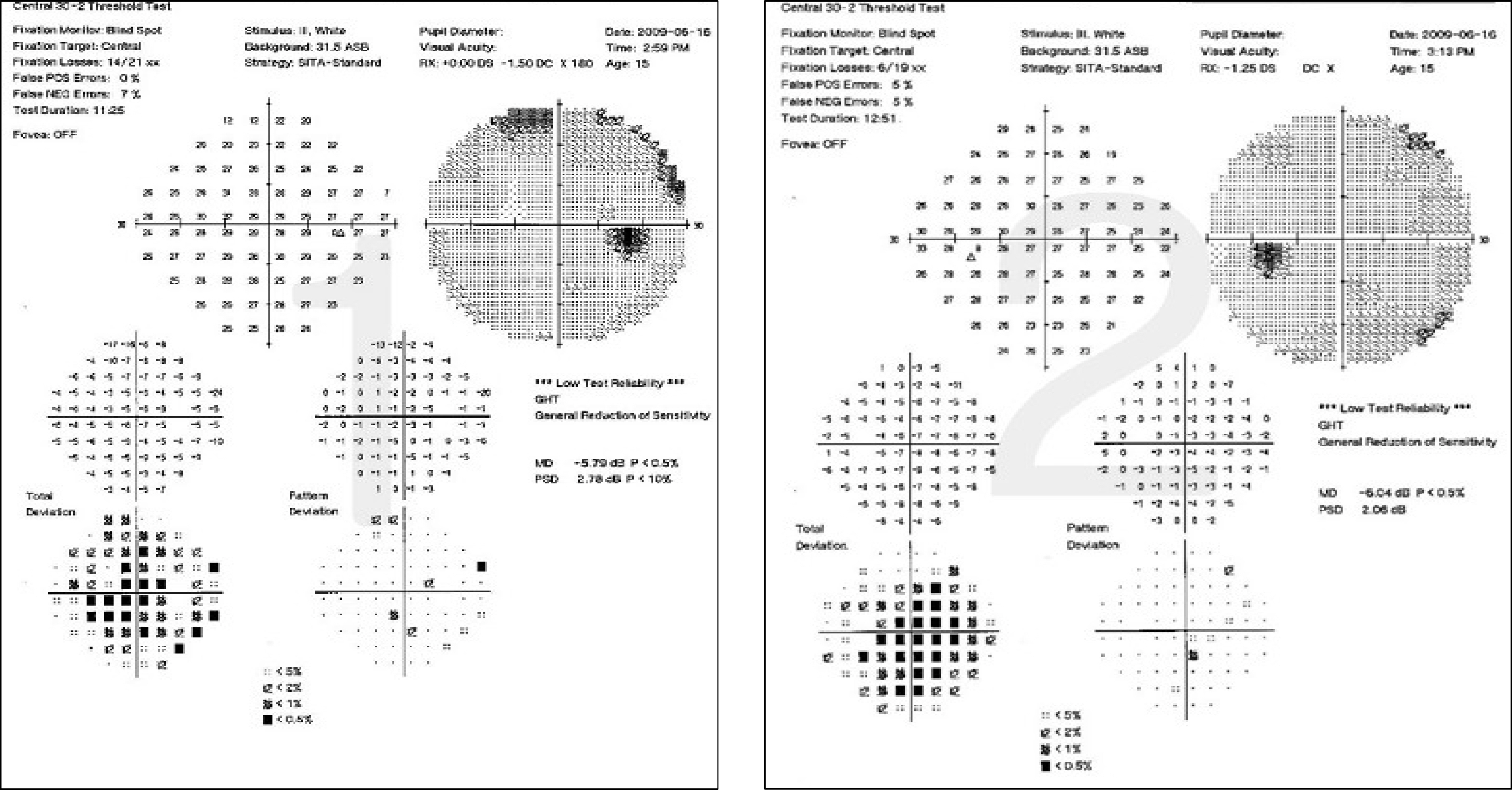
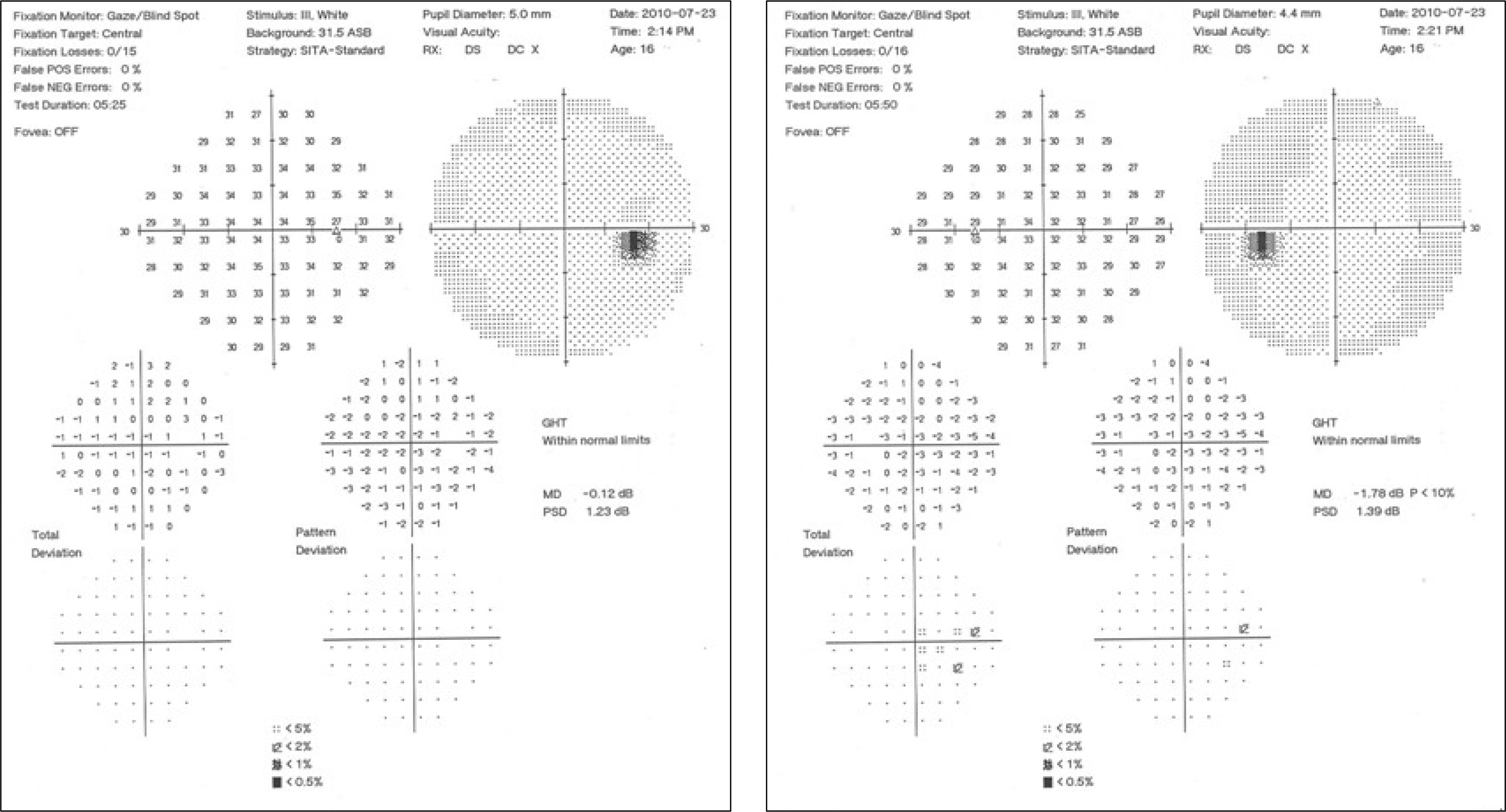
A 15-year-old girl, who had no ophthalmologic disease, complained of bilateral visual loss immediately after ECT. At the first ophthalmologic examination, best corrected visual acuity was 0.03 in both eyes. Findings of anterior segment and fundus, movement of external ocular muscles, and pupillary light reflex were normal. Visual field examination showed generalized reduction of sensitivity and increased fixation loss in both eyes. Optical coherence tomography revealed no abnormalities. Electroretinography was normal, and a slightly prolonged latency of P100 was noted in the right and left flash visual evoked potentials. Without any specific treatment, the patient's vision improved gradually after 18 hours of ECT and was recovered completely, with vision of 1.0 in both eyes the next day. There were no abnormalities in visual evoked potentials or the visual field.
CONCLUSIONS
Transient visual loss can occur after ECT, because of cortical blindness by transient cerebral ischemia, and can be recovered completely without specific treatment.
MeSH Terms
Figure
Cited by 1 articles
-
Recent Trends for Optimization of Electroconvulsive Therapy
Tak Youn, Ung Gu Kang, Yong Sik Kim, In Won Chung
J Korean Neuropsychiatr Assoc. 2016;55(1):12-24. doi: 10.4306/jknpa.2016.55.1.12.
Reference
-
References
1. Aldrich MS, Alessi AG, Beck RW, Gilman S. Cortical blindness: etiology, diagnosis, and prognosis. Ann Neurol. 1987; 21:149–58.
Article2. Parry R, Rees JR, Wilde P. Transient cortical blindness after coronary angiograhpy. Br Heart J. 1993; 70:563–4.3. Rodriguez A, Lozano JA, del Pozo D, Homar Paez J. Post-traumatic transient cortical blindness. Int Ophthalmol. 1993; 17:277–83.
Article4. Quattrocolo G, Leotta D, Appendino L, et al. A case of cortical blindness due to carbon monoxide poisoning. Ital J Neurol Sci. 1987; 8:57–8.
Article5. Gijtenbeek JM, van den Bent MJ, Vecht CJ. Cyclosporine neurotoxicity: a review. J Neurol. 1999; 246:339–46.
Article6. Huo R, Burden SK, Hoyt CS, Good WV. Chronic cortical visual impairment in children: etiology, prognosis, and associated neurological deficits. Br J Ophthalmol. 1999; 83:670–5.7. Cunningham FG, Fernandez CO, Hernandez C. Blindness associated with preeclampsia and eclampsia. Am J Obstet Gynecol. 1995; 172:1291–8.
Article8. Joseph JM, Louis S. Transient ictal cortical blindness during middle age. A case report and review of the the literature. J aberrations. 1995; 15:39–42.9. Cha IS, Kim HJ. Clinical study of cortical blindness after open-heart surgery. J Korean Ophthalmol. 1983; 24:865–8.10. Kwon IT, Nam KR, Kim BC. Cortical blindness after cerebral angiography. J Korean Ophthalmol Soc. 1992; 33:1238–42.11. Baek CE, Kim DS, Kim SH, Shin JC. Two cases of cortical blindness after gas exposure. J Korean Ophthalmol Soc. 1996; 37:1576–81.12. Cho HJ, Park JW, Seo MS. Transient cortical blindness related to general anesthesia. J Korean Ophthalmol Soc. 2001; 42:650–3.13. Miller NR. Walsh and Hoyt's Clinical Neuro-Ophthalmology. 4th ed.Baltimore: Williams & Wilkins;1991. p. 138–49.14. Yoon DH, Lee SW, Choi Y. Ophthalmology. 6th ed.Ilchokak;2002. p. 321–2.15. Belden JR, Caplan LR, Pessin MS, Kwan E. Mechanisms and clinical features of posterior border-zone infarcts. Neurology. 1999; 53:1312–8.
Article16. Kurani AP, Kellner CH, Turbin RE, et al. Transient visual loss after right unilateral ECT. J ECT. 2005; 21:186–7.
Article17. Sonavane S, Borade S, Gajbhiye S, et al. Cortical blindness associated with electroconvulsive therapy. J ECT. 2006; 22:155–7.
Article18. Subash M, Sheth HG, Saihan Z, Plant GT. Transient visual loss after seizures. Clin Experiment Ophthalmol. 2010 Apr 28. [Epub ahead of print].
Article19. Meyer JS, Gotoh F, Favale E. Cerebral metabolism during epileptic seizures in man. Electroencephalogr Clin Neurophysiol. 1966; 21:10–22.
Article20. Kahana A, Rowley HA, Weinstein JM. Cortical blindness: clinical and radiologic findings in reversible posterior leukoencephalop-athy syndrome. Ophthalmology. 2005; 112:e7–11.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Anesthetic Management during Electroconvulsive Therapy
- Anesthetic care for electroconvulsive therapy during pregnancy: A case report
- Electroconvulsive Treatment in Dementia With Lewy Bodies: A Case Report
- Comparision of Propofol and Thiopental Sodium as Anesthetic Agents for Electroconvulsive Therapy: Effects on Seizure Duration, Hemodynamic Responses and Recovery
- Combined Clozapine and Electroconvulsive Therapy in a Japanese Schizophrenia Patient: A Case Report