J Korean Ophthalmol Soc.
2010 Apr;51(4):626-630. 10.3341/jkos.2010.51.4.626.
A Case of Bilateral Retinal Hemorrhages Caused by Plasmodium Vivax Malaria
- Affiliations
-
- 1Department of Ophthalmology, Eulji University School of Medicine, Seoul, Korea. pjs4106@eulji.ac.kr
- KMID: 2213410
- DOI: http://doi.org/10.3341/jkos.2010.51.4.626
Abstract
- PURPOSE
To report a case of bilateral retinal hemorrhages caused by Plasmodium vivax malaria.
CASE SUMMARY
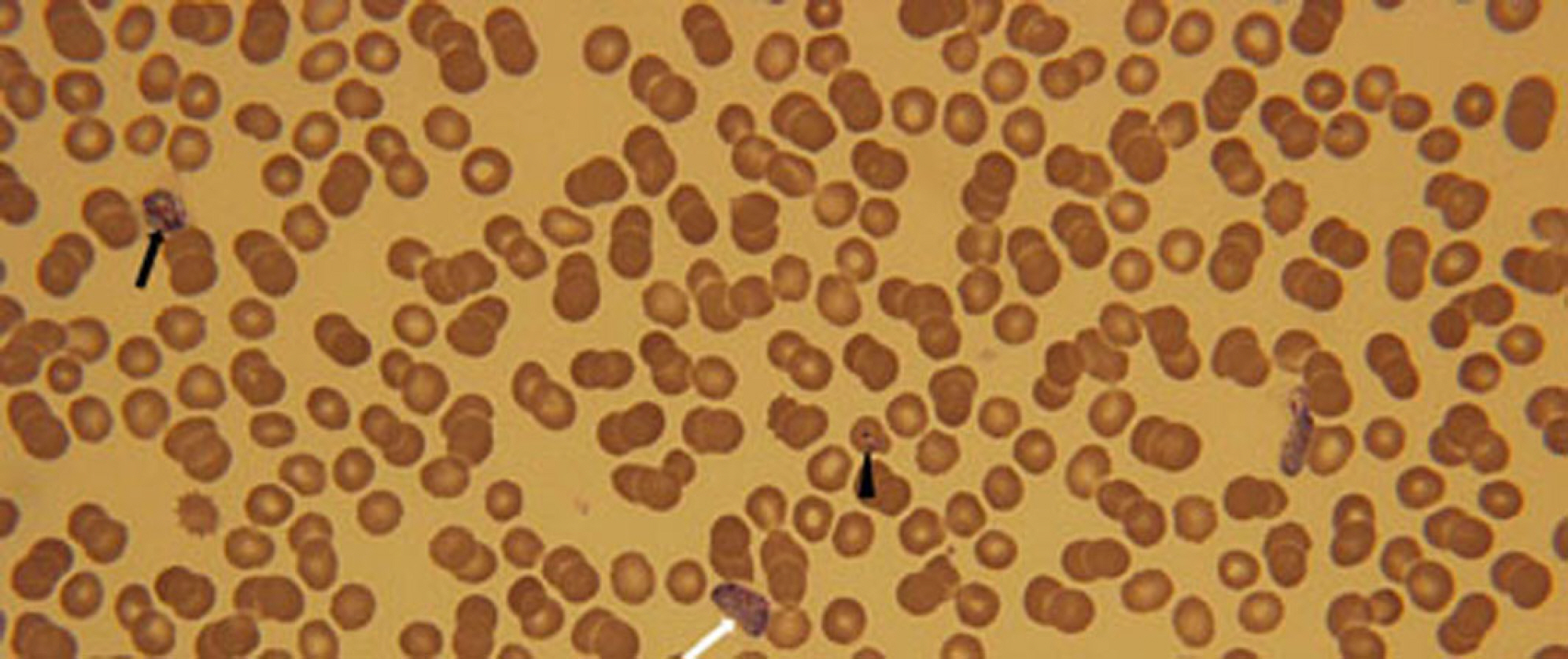
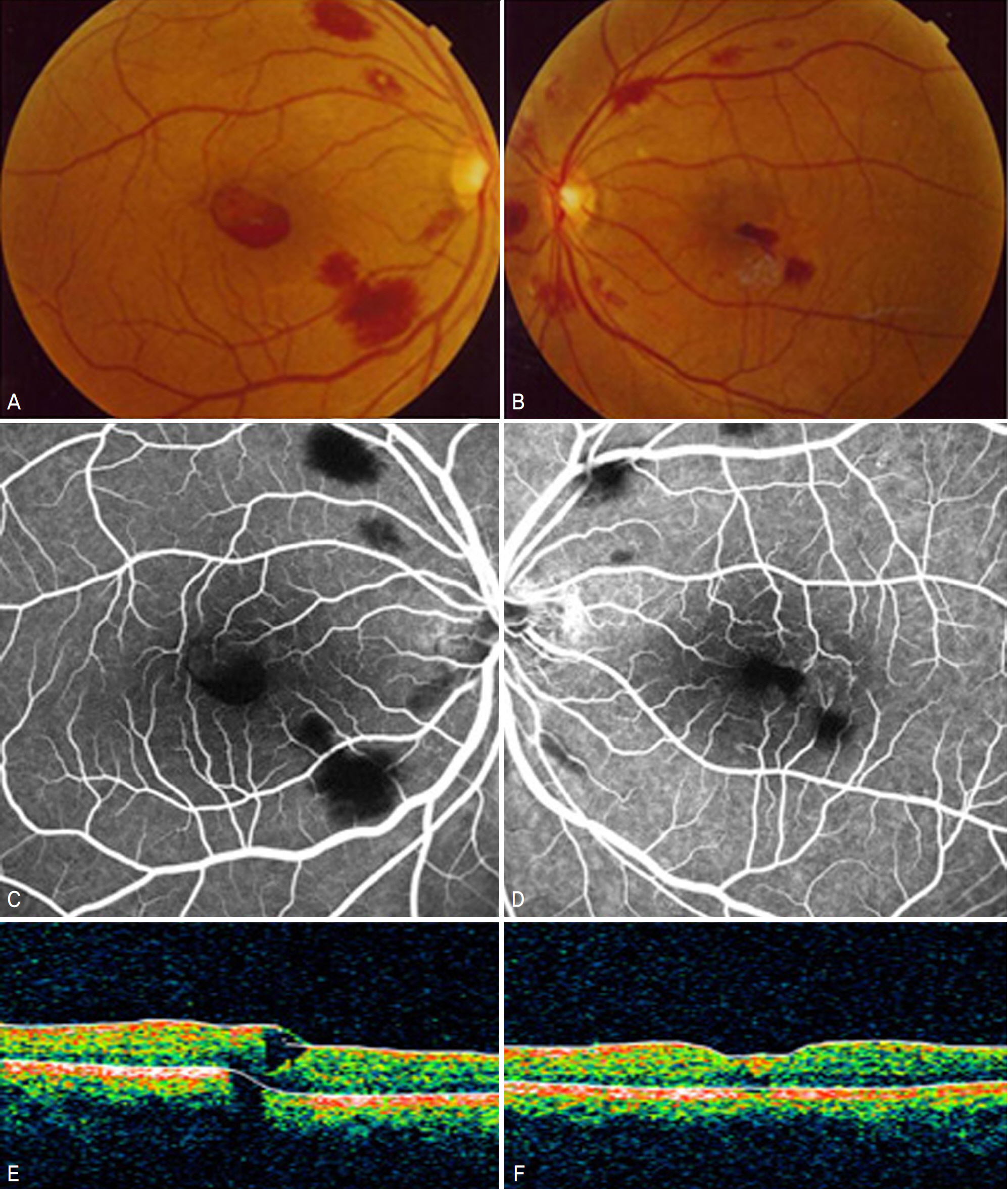
The 38-year-old male patient with cyclic high fever for 48 hours was admitted to the department of internal medicine in our hospital. He complained of decreased visual acuity of the left eye. The best corrected visual acuity was 1.0 in right eye and 0.3 in left eye. His blood hemoglobin concentration was 7.5 g/dl. Fundus examination revealed retinal hemorrhages in the posterior pole and preretinal hemorrhage in the macular area in his left eye. The peripheral blood smear confirmed Plasmodium vivax malaria. Hydroxychloroquine and Premaquine were given orally. Forty-nine days after the initial visit, retinal hemorrhages in the posterior pole and preretinal hemorrhage in the macula area occurred in his right eye. Although retinal hemorrhages in both eyes were reduced 100 days after the initial visit, the best corrected visual acuity was 0.2 in right eye and 0.4 in left eye and visual acuity did not improve.
CONCLUSIONS
Retinal hemorrhages infrequently can occur by Plasmodium viviax malaria and can result in permanent visual loss.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Three Various Cases of Retinal Hemorrhages Caused by Plasmodium vivax Malaria
Kyoung Jin Kim, Haeng Ku Kang, Kang Hoon Lee, Seok Jae Yang, Yeon Sung Moon
J Korean Ophthalmol Soc. 2011;52(7):863-870. doi: 10.3341/jkos.2011.52.7.863.
Reference
-
References
1. Kho WG. Reemergence of malaria in Korea. J Korean Med Assoc. 2007; 50:959–66.
Article2. Lewallen S, Taylor TE, Molyneux ME, et al. Association between measures of vitamin A and the ocular fundus findings in cerebral malaria. Arch Ophthalmol. 1998; 116:293–6.
Article3. Biswas J, Fogla R, Srinivasan P, et al. Ocular malaria. A clinical and histopathologic study. Ophthalmology. 1996; 103:1471–5.4. Kim SM, Kim KB, Jung HJ, et al. Retinal hemorrhage in an adult with Plasmodium vivax malaria. Korean J Infect Dis. 1997; 29:323–6.5. Chai IH, Lim GI, Yoon SN, et al. Occurrence of tertian malaria in a male patient who has never been abroad. Korean J Parasitol. 1994; 32:195–200.
Article6. Cho SY, Kong Y, Park SM, et al. Two vivax malaria cases detected in Korea. Korean J Parasitol. 1994; 32:281–4.
Article7. Lee JS, Kho WG, Lee HW, et al. Current status of vivax malaria among civilians in Korea. Korean J Parasitol. 1998; 36:241–8.
Article8. Yi KJ, Chung MH, Kim HS, et al. A relapsed case of imported abdominal malaria after a standard course of hydroxychloroquine and primaquine therapy. Korean J Parasitol. 1998; 36:143–6.9. Lee SH, Che JI, Hong ST, et al. Synopsis of medical parasitology. 1st ed.Seoul: Korea medical publishing co;1996. p. 400–12.10. Oh J, Kim HS, Huh K. Cerebral Malaria Associated with Retinal Hemorrhage on Macular Area. J Korean Ophthalmol Soc. 2003; 44:2699–704.11. Hidayat AA, Nalbandian RM, Sammons DW, et al. The abdominal histopathologic features of ocular malaria. Ophthalmology. 1993; 100:1183–6.12. Choi HJ, Lee SY, Yang H, et al. Retinal haemorrhage in vivax malaria. Trans R Soc Trop Med Hyg. 2004; 98:387–9.
Article13. Grant W. Ocular complications of malaria. Arch Ophthalmol. 1946; 35:48.
Article14. Olumese P, Adeyemo A, Gbadegesin R, Walker O. Retinal haemorrhage in cerebral malaria. East Afr Med J. 1997; 74:285–7.15. Carraro M, Rossetti L, Gerli G. Prevalence of retinopathy in abdominals with anemia or thrombocytopenia. Eur J Haematol. 2001; 67:238–44.16. Montero JA, Ruiz-Moreno JM, Sanchis E. Intraretinal abdominal associated with leishmaniasis. Ophthalmic Surg Lasers Imaging. 2003; 34:212–4.17. Kezuka T, Usui N, Suzuki E, et al. Ocular complications in mye-lodysplastic syndromes as preleukemic disorders. Jpn J Ophthalmol. 2005; 49:377–83.
Article18. Baker TR, Spencer WH. Ocular findings in multiple myeloma. A report of two cases. Arch Ophthalmol. 1974; 91:110–3.19. Nagpal KC, Goldberg MF, Rabb MF. Ocular manifestations of sickle hemoglobinopathies. Surv Ophthalmol. 1977; 21:391–411.
Article20. Looareesuwan S, Warrell D, White N, et al. Retinal hemorrhage, a common sign of prognostic significance in cerebral malaria. Am J Trop Med Hyg. 1983; 32:911–5.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Three Various Cases of Retinal Hemorrhages Caused by Plasmodium vivax Malaria
- Retinal Hemorrhage in an Adult with P. vivax Malaria
- A case of Plasmodium vivax malaria occurring during a school excursion to Pocheon-gun
- A Case of Plasmodium Vivax Malaria with Cerebral Complications
- A Case of Plasmodium vivax Malaria Associated with Autoimmune Hemolytic Anemia