J Korean Ophthalmol Soc.
2009 Oct;50(10):1447-1454. 10.3341/jkos.2009.50.10.1447.
The Size of Extraocular Muscles Estimated by Computed Tomography in Patients Undergoing Orbital Wall Fracture Repair
- Affiliations
-
- 1Department of Ophthalmology, CHA University, CHA Bundang medical center, Seongnam, Korea. eye@cha.ac.kr
- KMID: 2212759
- DOI: http://doi.org/10.3341/jkos.2009.50.10.1447
Abstract
- PURPOSE
To determine the cross sections of extraocular muscles in patients with orbital fracture and to demonstrate a relationship among the cross sections, the size of orbital fracture, the soft tissue, and fat herniation and limitation of ocular movement.
METHODS
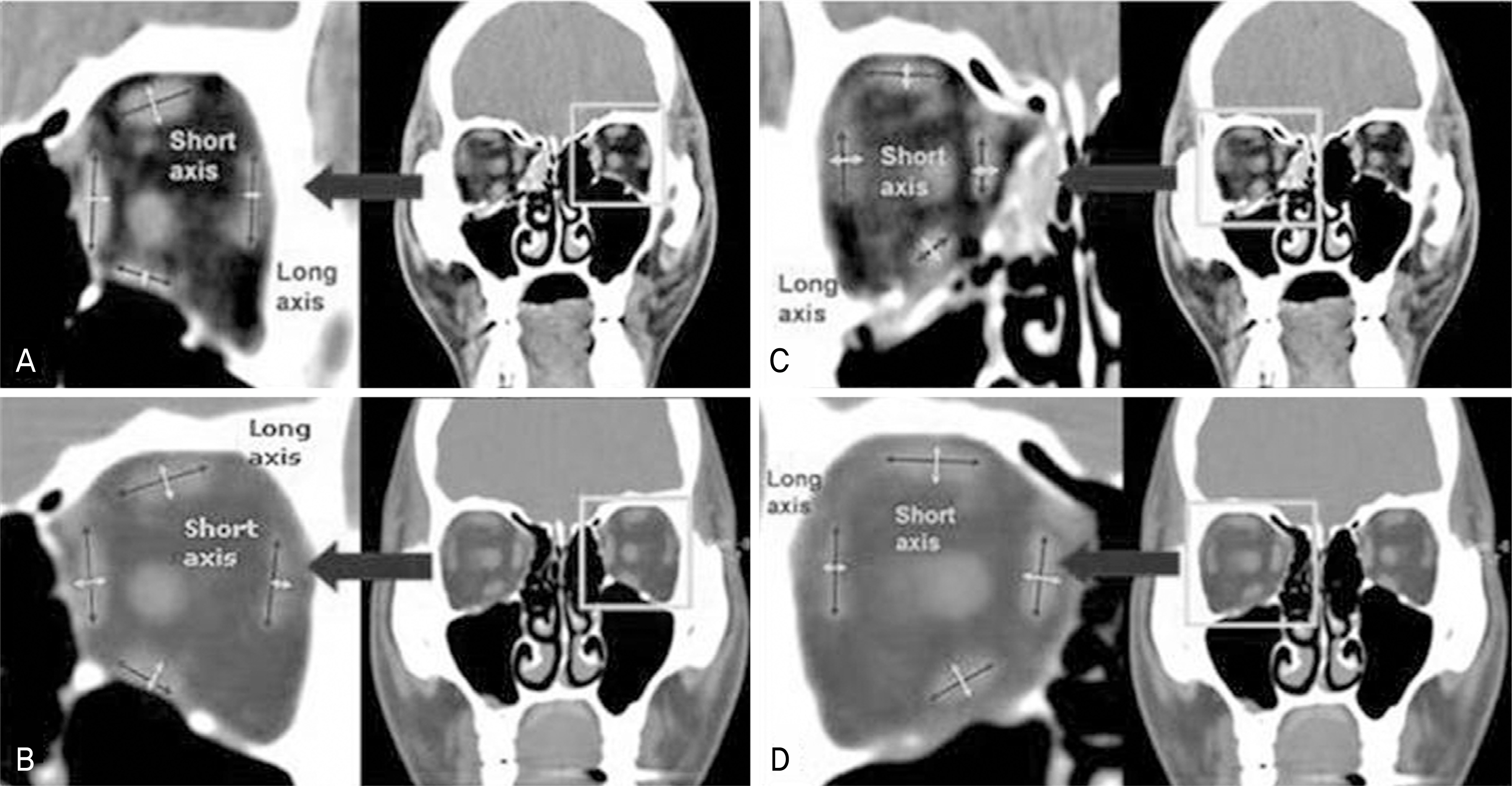
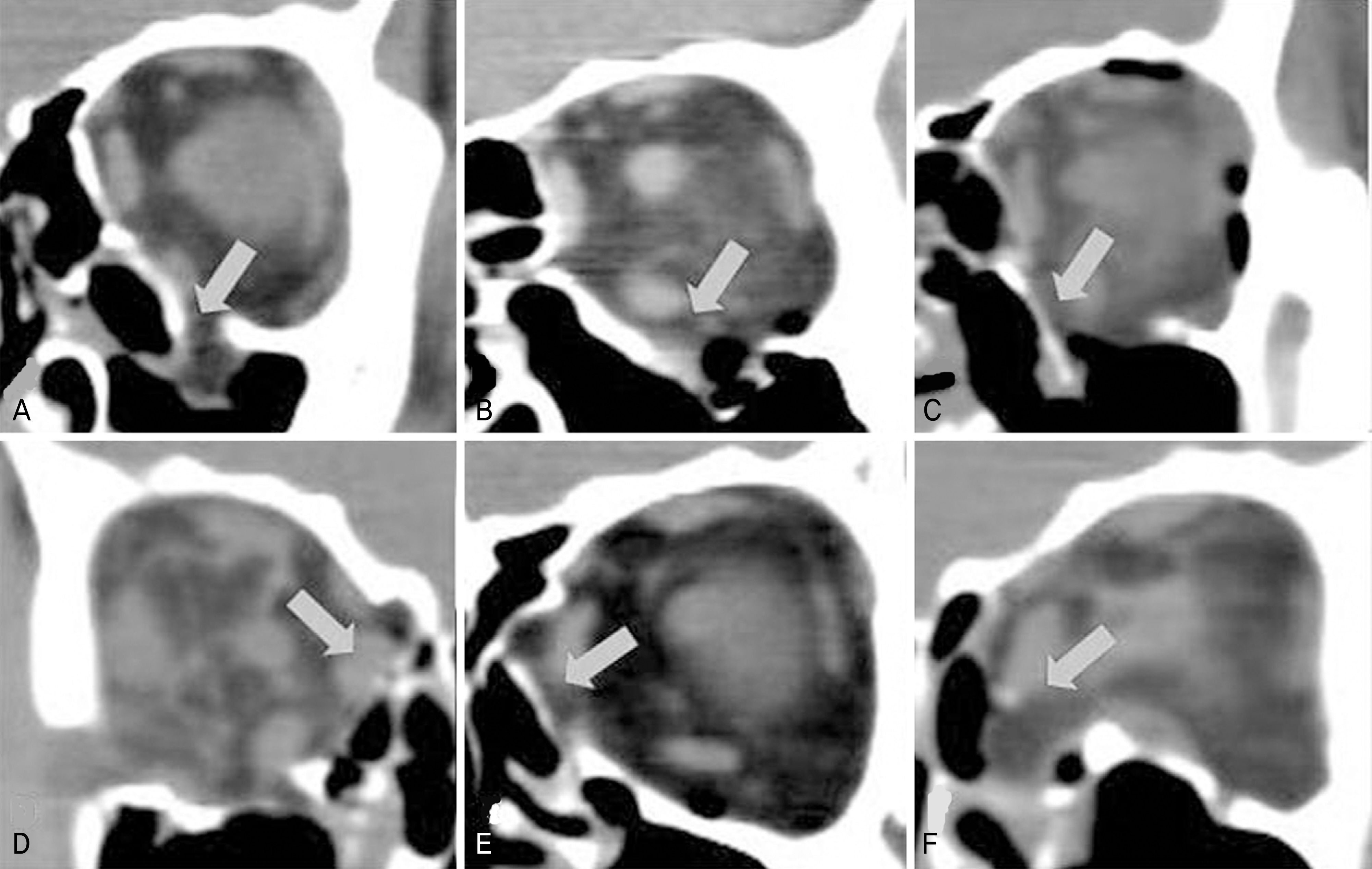
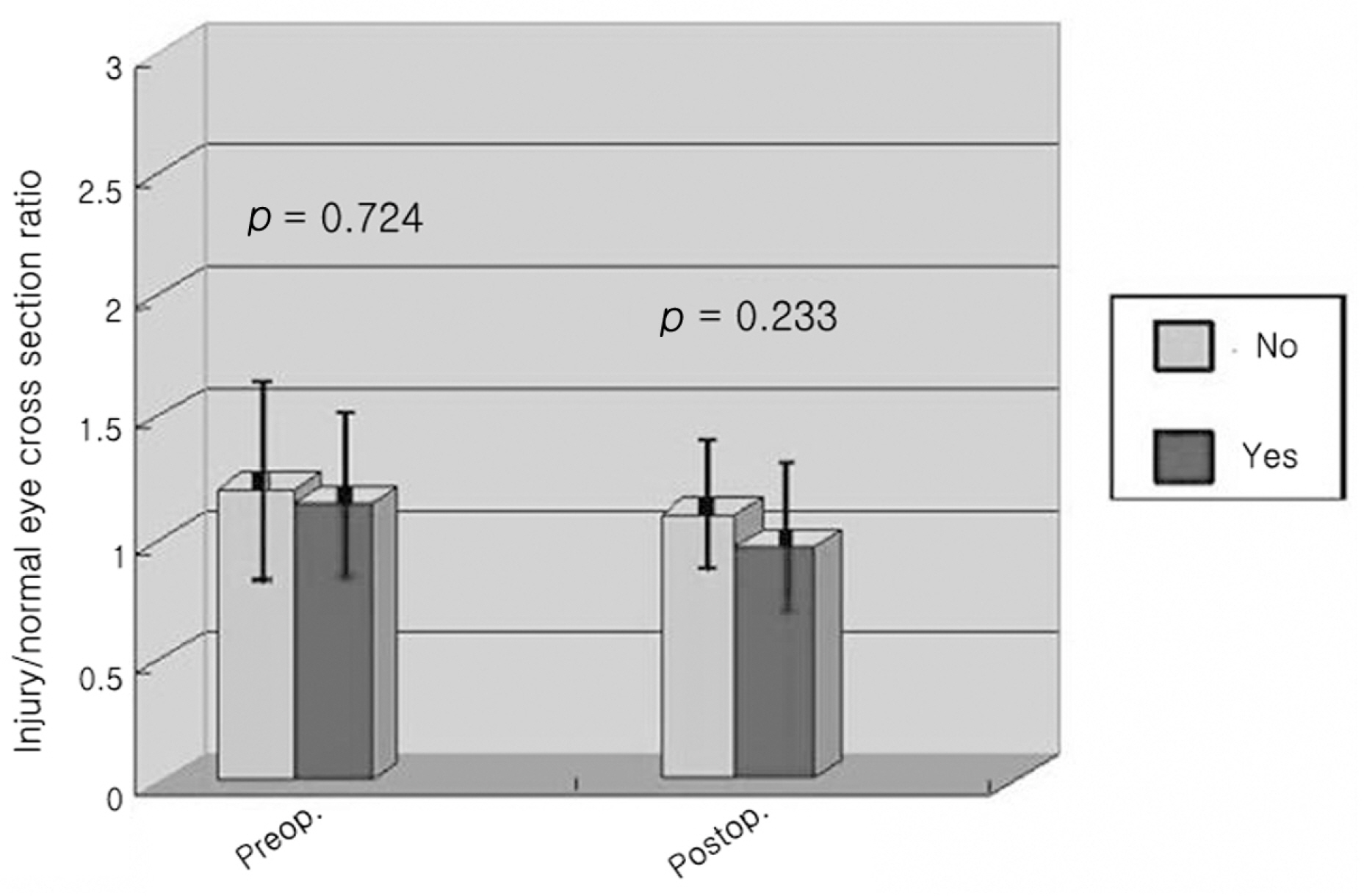
The study included 87 patients (87 eyes) with orbital fracture. The cross section was defined as multiplication of the long axis and short axis. The ratio of the cross section in normal and injured eyes was calculated at preoperative and postoperative periods.
RESULTS
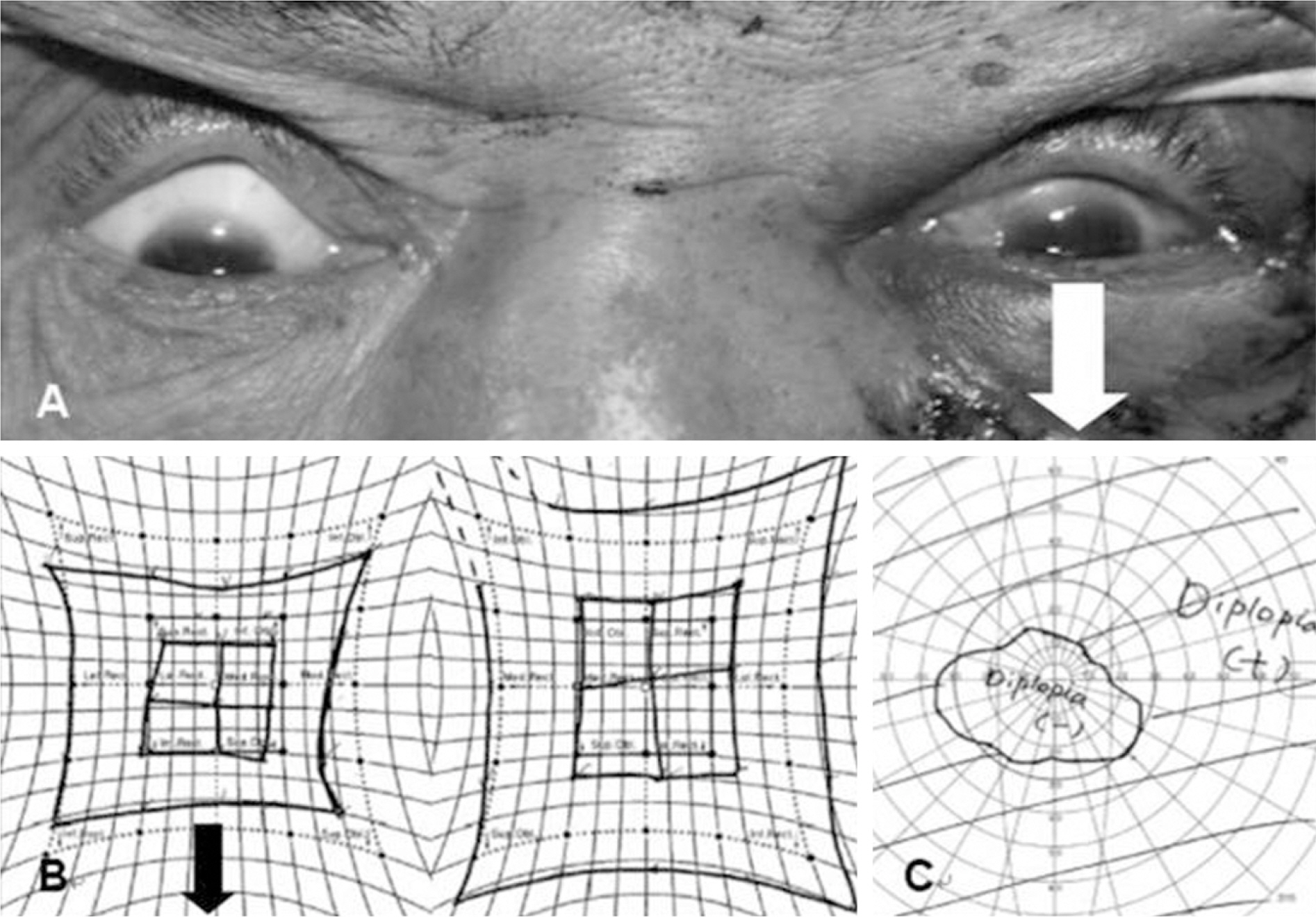
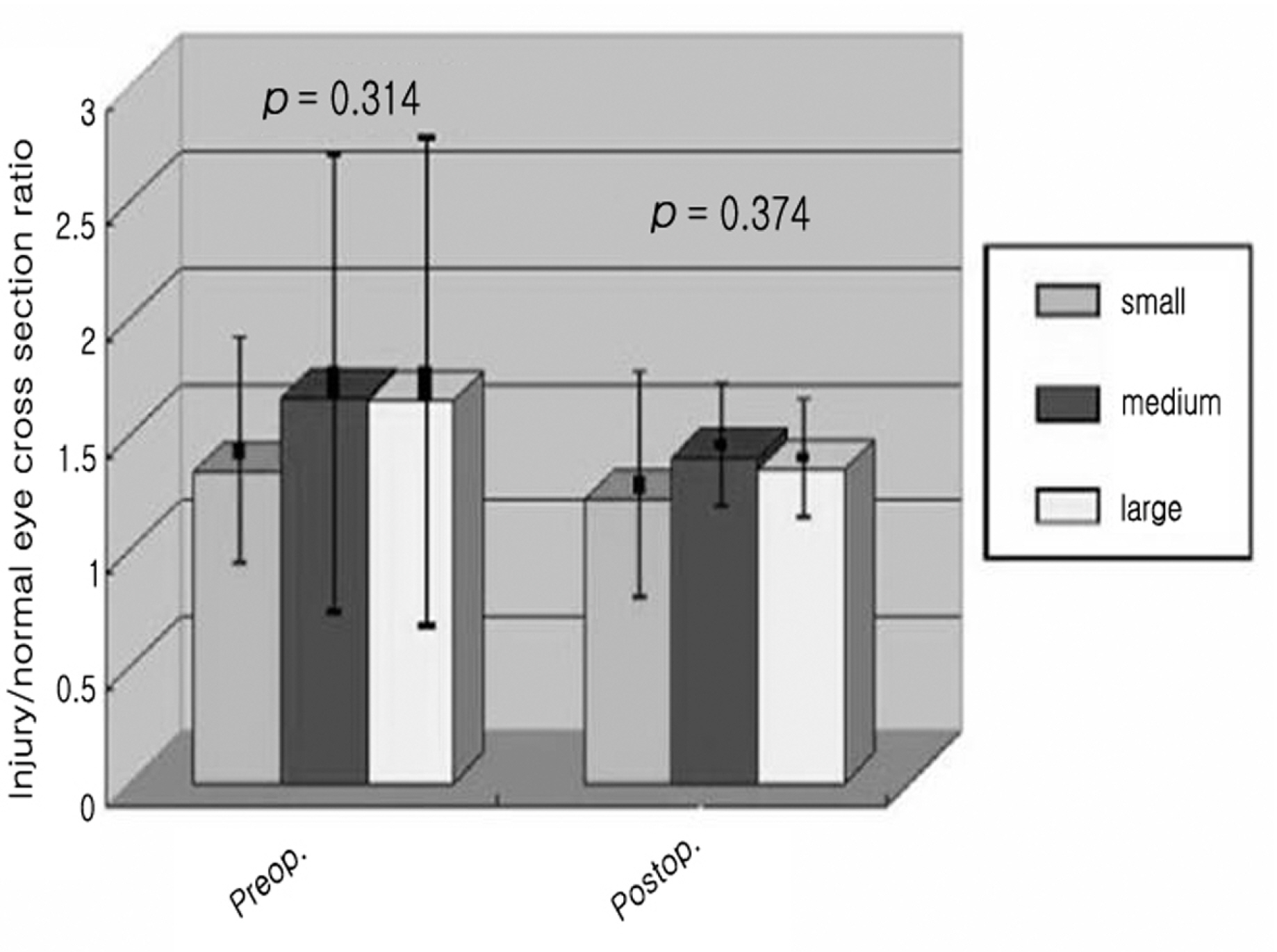
The cross sections of all rectus muscles, except for the superior, increased in injured eyes and subsequently decreased postoperatively. After surgery, the cross sections of lateral and medial rectus muscles recovered to near normal but the inferior remained enlarged. The increased ratio of the short and long axis was significant but not the difference of the cross sections related to the short and long axis ratio. There was a preoperative difference between injured/normal cross section ratio in relation to the size of inferior fracture. There was postoperative normalization for the cross sections of inferior rectus muscles with the restrictive limitation due to inferior fracture.
CONCLUSIONS
The cross sections increased mostly after orbital fracture and subsequently decreased postoperatively. There was a change in the cross section ratio with the size of inferior fracture at preoperative period but there was no change in the cross sections related to the restrictive or paralytic limitation, except for eyes with the restriction secondary to inferior fracture. These were significantly normalized postoperatively in cross section.
Keyword
MeSH Terms
Figure
Cited by 3 articles
-
Clinical Manifestations and Computed Tomography Findings of Trapdoor Type Medial Orbital Wall Blowout Fracture
Sung Ha Hwang, Su jin Park, Mijung Chi
J Korean Ophthalmol Soc. 2020;61(2):117-124. doi: 10.3341/jkos.2020.61.2.117.A Study of Different Aspects of Blowout Fracture Between Preoperative CT and Intraoperative Images
Dong Sik Ham, Chung Hyun Lee, Jae Wook Yang
J Korean Ophthalmol Soc. 2011;52(8):902-909. doi: 10.3341/jkos.2011.52.8.902.Comparison of Diplopia and Ocular Torsion Rate in Blow-Out Fracture Patients
Kyoung Lae Kim, Sung Pyo Park, Hyoung Kyun Kim
J Korean Ophthalmol Soc. 2015;56(2):162-167. doi: 10.3341/jkos.2015.56.2.162.
Reference
-
References
1. Paek SH, Kim YS, Lee TS. A clinical study of blowout fracture. J Korean Ophthalmol Soc. 1993; 34:1194–8.2. Lee SY, Kim SY, Kim HB. Orbital fractures evaluated by computed tomography. J Korean Ophthalmol Soc. 1990; 31:249–53.3. Ahn SK, Jung SW. The clinical aspects of orbital fractures proven by computed tomography. J Korean Ophthalmol Soc. 1997; 38:2077–83.4. Lee MS, Ahn JH, Kim HY, Lee SY. Clinical study of orbital wall fracture. J Korean Ophthalmol Soc. 1997; 38:1687–93.5. Kwon YH, Park DW, Chung JY, Ahn HB. A clinical study of pediatric orbital wall fracture. J Korean Ophthalmol Soc. 2006; 47:7–12.6. Park SH, Rah SH, Kim YH. Clinical evaluation of the associated ocular injuries of orbital wall fracture patients. J Korean Ophthalmol Soc. 2002; 43:1474–81.7. Gilbard SM, Mafee MF, Lagouros PA, Langer BG. The prognostic significance of computed tomography. Ophthalmology. 1985; 92:1523–8.8. Harris GJ, Garcia GH, Logani SC, Murphy ML. Correlation of preoperative computed tomography and postoperative ocular motility in orbital blowout fractures. Ophthalmic Plast Reconstr Surg. 2000; 16:179–87.
Article9. Lee SH, Lew H, Yun YS. Ocular motility disturbances in orbital wall fracture patients. Yonsei Med J. 2005; 46:359–67.
Article10. Raskin EM, Millman AL, Lubkin V, et al. Prediction of late enophthalmos by volumetric analysis of orbital fractures. Ophthalmic Plast Reconstr Surg. 1998; 14:19–26.
Article11. Schuknecht B, Carls F, Valavanis A, Sailer HF. CT assessment of orbital volume in late post-traumatic enophthalmos. Neuroradiology. 1996; 38:470–5.
Article12. Levine LM, Sires BS, Gentry LR, Dortzbach RK. Rounding of the inferior rectus muscle: A helpful radiologic finding in the manage –ment of orbital floor fractures. Ophthalmic Plast Reconstr Surg. 1998; 14:141–3.13. Matic DB, Tse R, Banerjee A, Moore CC. Rounding of the inferior rectus muscle as a predictor of enophthalmos in orbital floor fractures. J Craniofac Surg. 2007; 18:127–32.
Article14. Smith B, Lisman RD, Simonton J, Della Rocca R. Volkmann's contracture of the extraocular muscles following blowout fracture. Ophthalmic Plast Reconstr Surg. 1984; 74:200–16.
Article15. Baldeschi L, Lupetti A, Vu P, et al. Reactivation of Graves'– orbitopathy after rebabilitative orbital decompression. Ophthal– mology. 2007; 114:1395–402.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Superior Orbital Fissure Syndrome after Repair of Blow Out Fracture
- Ocular Motility Disturbances in Orbital Wall Fracture Patients
- Factors Affecting Persistent Diplopia after Surgical Repair of Isolated Inferior Orbital Wall Fracture
- A Case of Idiopathic Orbital Myositis Involving All Extraocular Muscles of Both Eyes
- Transcaruncular Approach to Blowout Fractures of the Medial Orbital Wall