J Korean Ophthalmol Soc.
2016 May;57(5):815-822. 10.3341/jkos.2016.57.5.815.
Long-Term Intraocular Pressure Outcome in Fellow Eyes with Angle-Closure Glaucoma after Laser Iridotomy and Phacoemulsification
- Affiliations
-
- 1Department of Ophthalmology, Hallym University Sacred Heart Hospital, Hallym University College of Medicine, Anyang, Korea. kyungwlee@hanmail.net
- 2Department of Ophthalmology, Armed Forces DaeGu Hospital, Gyeongsan, Korea.
- KMID: 2212726
- DOI: http://doi.org/10.3341/jkos.2016.57.5.815
Abstract
- PURPOSE
To evaluate long-term change in intraocular pressure (IOP) in the fellow eyes after laser iridotomy and early phacoemusification with laser iridotomy in patients with acute angle-closure glaucoma.
METHODS
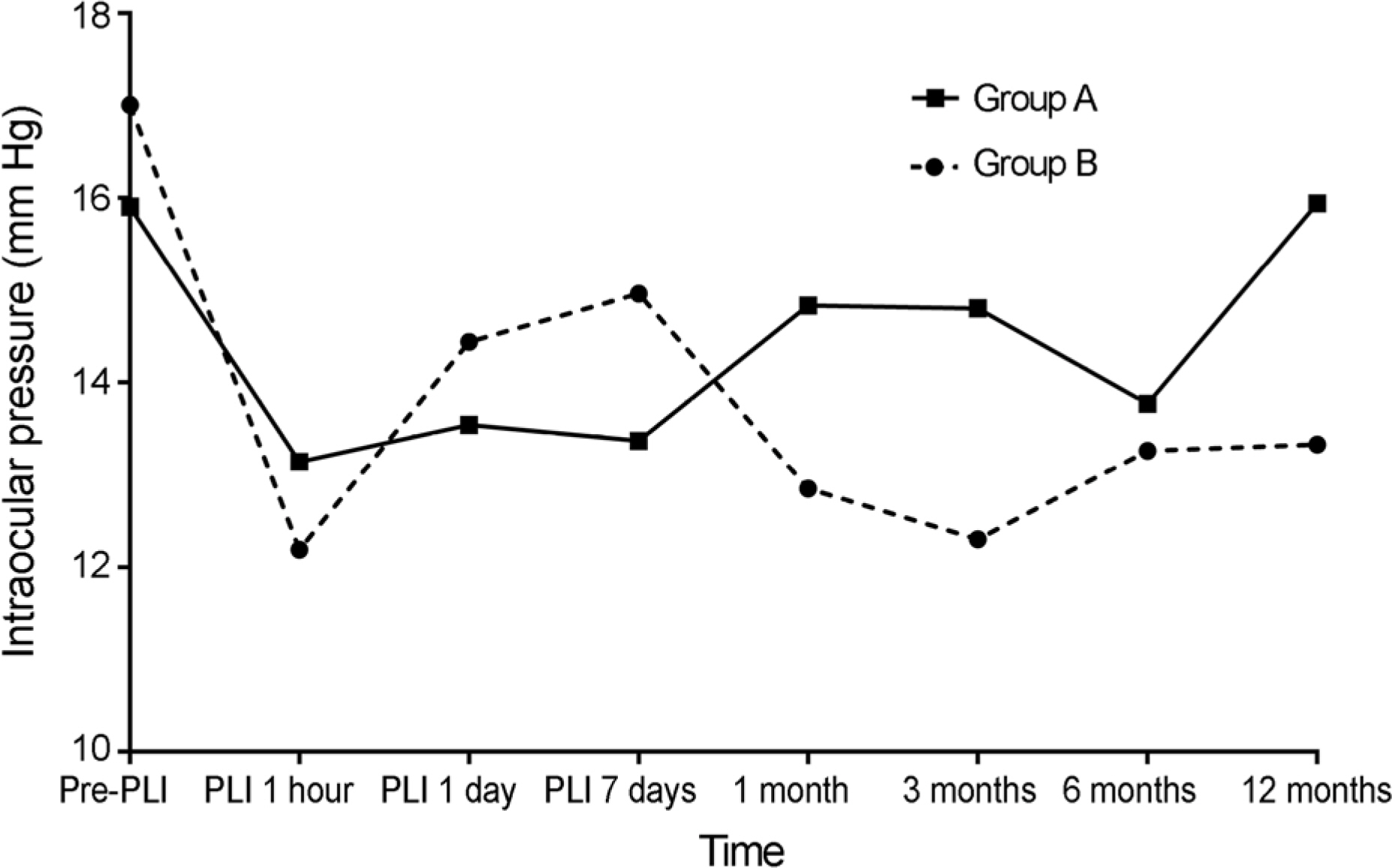
We performed a retrospective, comparative chart review of 62 patients with acute angle-closure glaucoma; 35 patients (Group A) who underwent only prophylactic laser iridotomy on fellow eyes and 27 patients (Group B) who underwent prophylactic laser iridotomy and early phacoemusification on fellow eyes. Patients were followed up at 1 day, 1 week and 1, 3, 6 and 12 months. IOP change was analyzed after laser iridotomy 1 hour and at every follow-up. In addition, visual acuity and complications of laser iridotomy and phacoemusification were determined.
RESULTS
In Group A, the mean IOP increase in fellow eyes occurred within 1 month after laser iridotomy (initial, 15.9 ± 5.0 mm Hg; final, 15.9 ± 2.6 mm Hg), However, in Group B, the mean IOP of fellow eyes was maintained up to 12 months without an increase in IOP (initial, 17.0 ± 3.3 mm Hg; final, 13.3 ± 2.8 mm Hg) Among the fellow eyes, 13 patients in Group A (37.14%) and 4 patients in Group B (14.81%, p = 0.032) underwent further medical therapy. The initial visual acuity of fellow eyes in Group A was 0.78 ± 0.21 and 0.71 ± 0.22 in Group B, and at the final visit, 0.73 ± 0.31 in Group A and 0.93 ± 0.27 in Group B (p = 0.003).
CONCLUSIONS
We found that most fellow eyes treated with laser iridotomy and phacoemulsification maintained satisfactory IOP and good vision. These results support that laser iridotomy and phacoemulsification in the fellow eye with acute angle-closure glaucoma is a reasonable prophylactic treatment.
MeSH Terms
Figure
Reference
-
References
1. Shin SG. Ahn JH. Rho SH. Aclinical analysis on 456 cases of glaucoma among outpatients during 5 years. J Korean Ophthalmol Soc. 1987; 28:1021–6.2. Song MS. Kim DG. Kim HJ. Clinical study on glaucomatous patients. J Korean Ophthalmol Soc. 1989; 30:755–9.3. Robin AL. Pollack IP. Argon laser peripheral iridotomies in the treatment of primary angle closure glaucoma. Long-term follow-up. Arch Ophthalmol. 1982; 100:919–23.4. Salmon JF. Long-term intraocular pressure control after Nd-YAG laser iridotomy in chronic angle-closure glaucoma. J Glaucoma. 1993; 2:291–6.
Article5. Lam DS. Lai JS. Tham CC, et al. Argon laser peripheral iridoplasty versus conventional systemic medical therapy in treatment of acute primary angle-closure glaucoma: a prospective, randomized, controlled trial. Ophthalmology. 2002; 109:1591–6.
Article6. Aung T. Ang LP. Chan SP. Chew PT. Acute primary angle-closure: long-term intraocular pressure outcome in Asian eyes. Am J Ophthalmol. 2001; 131:7–12.
Article7. Alsagoff Z. Aung T. Ang LP. Chew PT. Long-term clinical course of primary angle-closure glaucoma in an Asian population. Ophthalmology. 2000; 107:2300–4.
Article8. Lee HJ. Kim JH. Sohn YH. Long-term intraocular pressure change in attacked and fellow eyes with acute angle-closure glaucoma after laser iridotomy. J Korean Ophthalmol Soc. 2004; 45:1298–303.9. Lim LS. Husain R. Gazzard G, et al. Cataract progression after prophylactic laser peripheral iridotomy: potential implications for the prevention of glaucoma blindness. Ophthalmology. 2005; 112:1355–9.10. Ming Zhi Z. Lim AS. Yin Wong T. A pilot study of lens extraction in the management of acute primary angle-closure glaucoma. Am J Ophthalmol. 2003; 135:534–6.
Article11. Tarongoy P. Ho CL. Walton DS. Angle-closure glaucoma: the role of the lens in the pathogenesis, prevention, and treatment. Surv Ophthalmol. 2009; 54:211–25.
Article12. Hayashi K. Hayashi H. Nakao F. Hayashi F. Effect of cataract surgery on intraocular pressure control in glaucoma patients. J Cataract Refract Surg. 2001; 27:1779–86.
Article13. Jacobi PC. Dietlein TS. Lüke C, et al. Primary phacoemulsification and intraocular lens implantation for acute angle-closure glaucoma. Ophthalmology. 2002; 109:1597–603.14. Pereira FA. Cronemberger S. Ultrasound biomicroscopic study of anterior segment changes after phacoemulsification and foldable intraocular lens implantation. Ophthalmology. 2003; 110:1799–806.
Article15. Mei L. Zhonghao W. Zhen M, et al. Lens thickness and position of primary angle closure measured by anterior segment optical coherence tomography. J Clin Exp Ophthalmol. 2013; 4:281.
Article16. Shams PN. Foster PJ. Clinical outcomes after lens extraction for visually significant cataract in eyes with primary angle closure. J Glaucoma. 2012; 21:545–50.
Article17. Musch DC. Gillespie BW. Niziol LM, et al. Cataract extraction in the collaborative initial glaucoma treatment study; incidence, risk factors, and the effect of cataract progression and extraction on clinical and quality-of-life outcomes. Arch Ophthalmol. 2006; 124:1694–700.18. Lowe RF. Aetiology of the anatomical basis for primary angle-closure glaucoma. Biometrical comparisons between normal eyes and eyes with primary angle-closure glaucoma. Br J Ophthalmol. 1970; 54:161–9.
Article19. Krupin T. Mitchell MB. Johnson MF. Becker B. The long-term effects of iridectomy for primary acute angle-closure glaucoma. Am J Ophthalmol. 1978; 86:506–9.
Article20. Lee HB. Hwang US. Yoo JM. Song JK. Sequential agon and Nd: YAG laser iridotomies in angle closure glaucoma. J Korean Ophthalmol Soc. 1999; 40:2245–51.21. Choi DK. Hyung S. Re-elevation of intraocular pressure after peripheral laser iridotomy in patients with closed angle. J Korean Ophthalmol Soc. 2011; 52:716–20.
Article22. Friedman DS. Chew PT. Gazzard G, et al. Long-term outcomes in fellow eyes after acute primary angle closure in the contralateral eye. Ophthalmology. 2006; 113:1087–91.
Article23. Kim YY. Jung HR. Clarifying the nomenclature for primary angle-closure glaucoma. Surv Ophthalmol. 1997; 42:125–36.
Article24. Chandler PA. Trotter RR. Angle-closure glaucoma; subacute types. AMA Arch Ophthalmol. 1955; 53:305–17.25. Lowe RF. Angle-closure, pupil dilatation, and pupil block. Br J Ophthalmol. 1966; 50:385–9.
Article26. Wishart PK. Atkinson PL. Extracapsular cataract extraction and posterior chamber lens implantation in patients with primary chronic angle-closure glaucoma: effect on intraocular pressure control. Eye (Lond). 1989; 3:6. 706–12.
Article27. Koo BS. Chung J. Baek NH. The effect of extracapsular cataract extraction in patients with chronic angle-closure glaucoma combined with cataract. J Korean Ophthalmol Soc. 1996; 37:1045–53.28. Lam DS. Leung DY. Tham CC, et al. Randomized trial of early phacoemulsification versus peripheral iridotomy to prevent intraocular pressure rise after acute primary angle closure. Ophthalmology. 2008; 115:1134–40.
Article29. Ang LP. Aung T. Chew PT. Acute primary angle closure in an Asian population: long-term outcome of the fellow eye after prophylactic laser peripheral iridotomy. Ophthalmology. 2000; 107:2092–6.30. Nonaka A. Kondo T. Kikuchi M, et al. Cataract surgery for residual angle closure after peripheral laser iridotomy. Ophthalmology. 2005; 112:974–9.
Article31. Schwartz AL. Martin NF. Weber PA. Corneal decompensation after argon laser iridectomy. Arch Ophthalmol. 1988; 106:1572–4.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Long-term Intraocular Pressure Outcome after Successful Laser Iridotomy for the Acute Primary Angle-closure Glaucoma
- Clinical Results of the Q-Switched Nd-YAG Laser Iridotomy
- Long-term Intraocular Pressure Change in Attacked and Fellow eyes with Acute Angle-closure Glaucoma after Laser Iridotomy
- Effect of YAG Laser Iridotomy on IOP in Chronic Angle-closure Glaucoma
- Clinical Experience of Q-switched Nd:YAG Laser Iridotomy 50 cases for Angle Glosure Glaucoma