J Korean Ophthalmol Soc.
2009 Aug;50(8):1275-1281. 10.3341/jkos.2009.50.8.1275.
Best Disease With Old-age Onset Misdiagnosed as Chronic Central Serous Chorioretinopathy: A Case Report
- Affiliations
-
- 1Department of Ophthalmology, Konkuk University Medical Center, Konkuk University School of Medicine, Seoul, Korea. eyekim@kuh.ac.kr
- KMID: 2212554
- DOI: http://doi.org/10.3341/jkos.2009.50.8.1275
Abstract
- PURPOSE
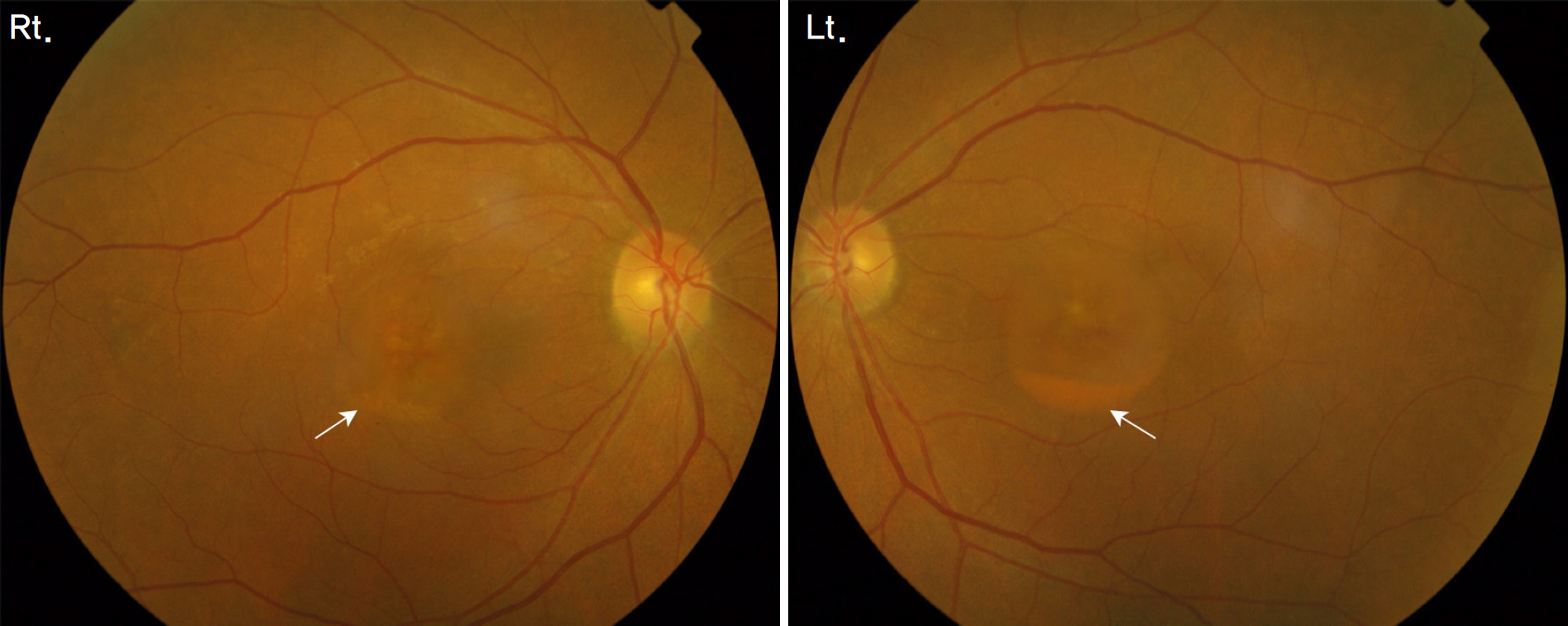
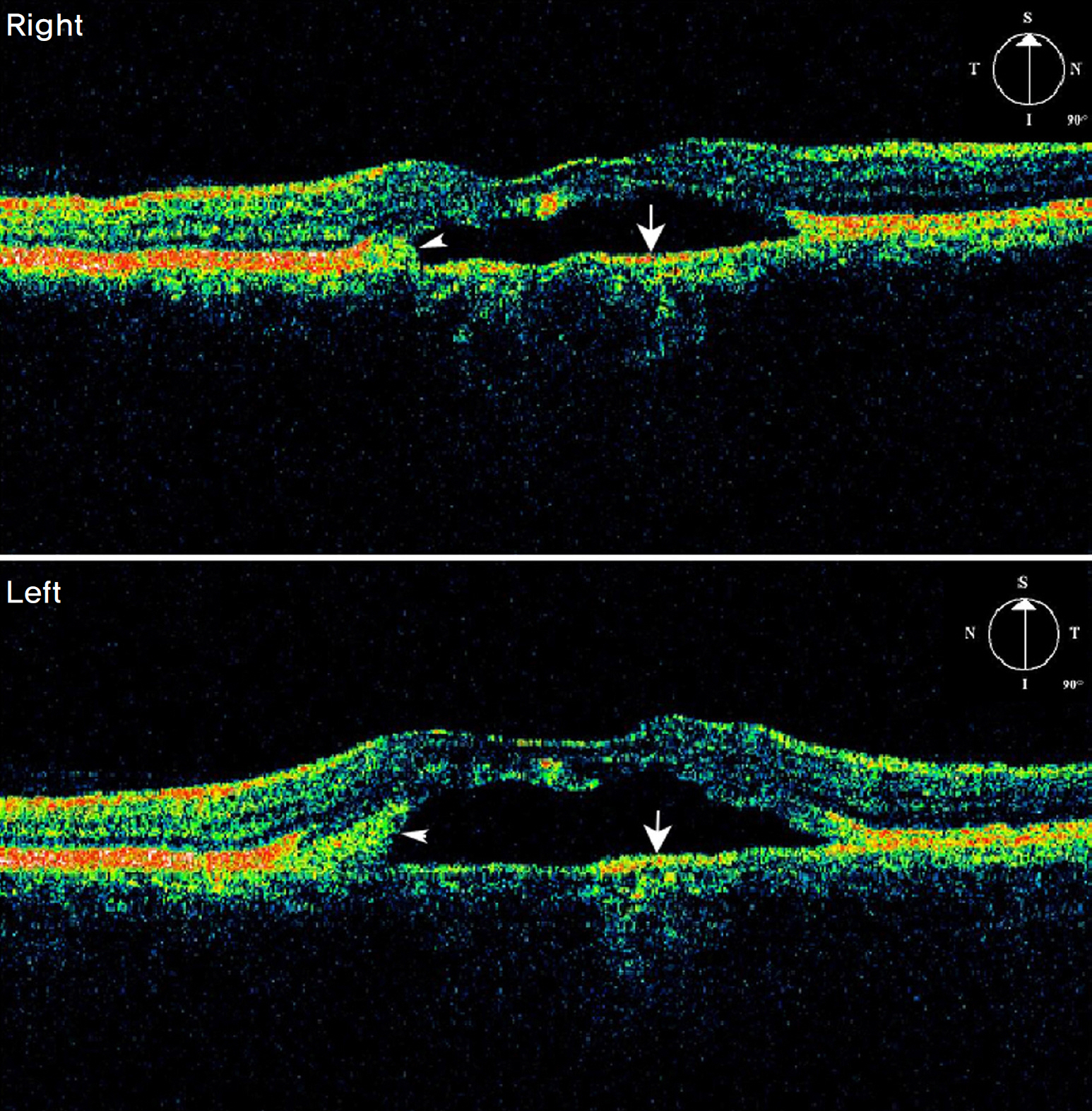
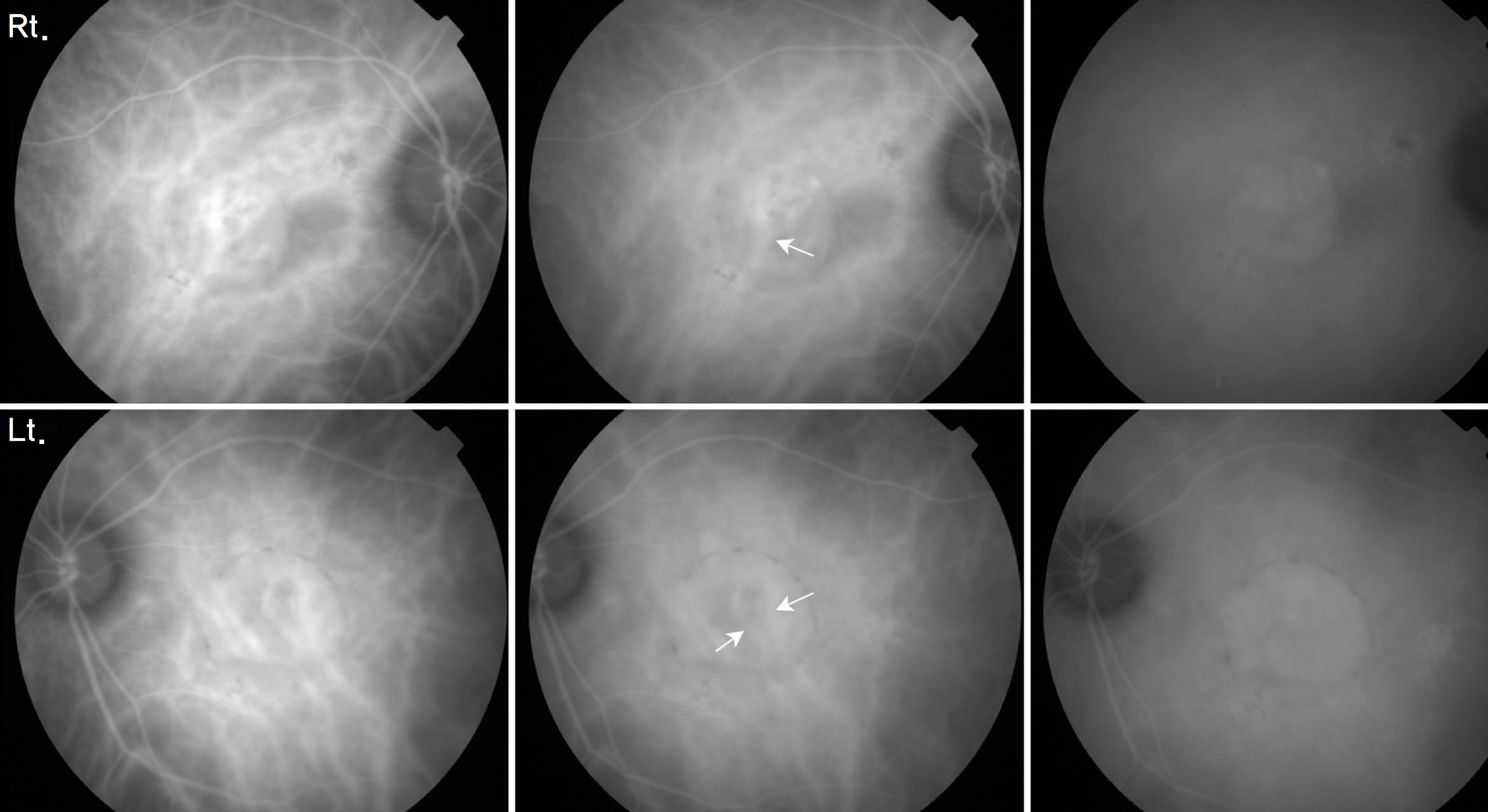
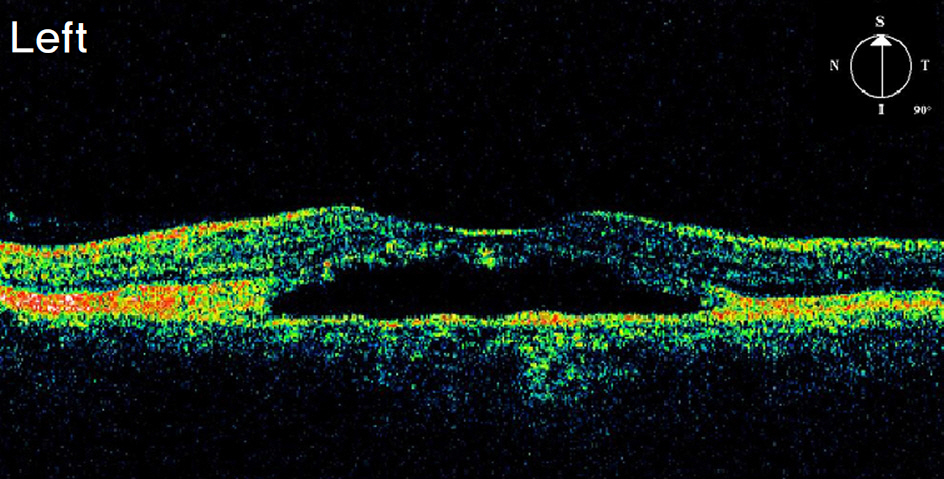
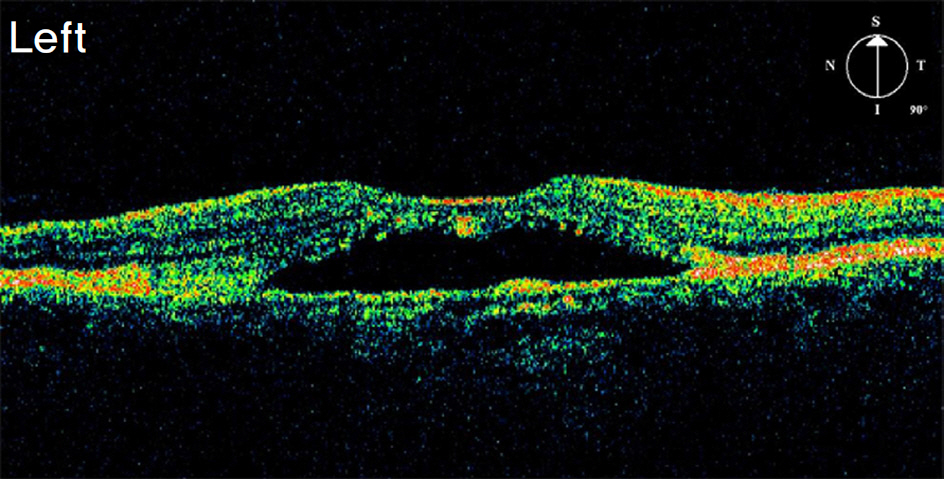
To report a case of Best's disease with old-age-onset with unusual clinical features. CASE SUMMARY: A 68-year-old woman with a six-month history of using oral steroids complained of decreased vision in both eyes. Fundus examination revealed a circular area of macular elevation measuring approximately 1.5 disc diameter size in both eyes. Optical coherence tomography (OCT) showed serous retinal detachment, but pigment epithelial detachment was seen only on fluorescein angiography and indocyanine green angiography. The patient received a diagnosis of chronic central chorioretinopathy with choroidal neovascularization. Photodynamic therapy (PDT) and intravitreal bevacizumab (IVB) injections were prescribed as treatment, but were ineffective. For a definitive diagnosis, we performed an electro-oculogram (EOG) and the result was abnormal with an Arden ratio below 1.5 in both eyes. A final diagnosis of Best's disease was established. Spectral domain OCT findings at the last visit showed a clearly visible RPE split and a low reflective space between the split RPE layers, as well as a high reflectivity corresponding to the subretinal material. CONCLUSIONS: We report a case of Best's disease with old-age onset with unusual clinical features and abnormal EOG findings. Spectral domain OCT was helpful in evaluating the disease. Treatment with PDT and IVB was not effective.
Keyword
MeSH Terms
-
Aged
Angiography
Antibodies, Monoclonal, Humanized
Choroidal Neovascularization
Electrooculography
Eye
Female
Fluorescein Angiography
Humans
Indocyanine Green
Photochemotherapy
Retinal Detachment
Steroids
Tomography, Optical Coherence
Triazenes
Vision, Ocular
Vitelliform Macular Dystrophy
Bevacizumab
Antibodies, Monoclonal, Humanized
Indocyanine Green
Steroids
Triazenes
Figure
Reference
-
References
1. Best F. Uber eine hereditaere makulaaffection; Beitraege zurverer-bungslehre. Zschr Augenheilk. 1905; 13:199–212.2. Marmorstein AD, Marmorstein LY, Rayborn M, et al. Bestrophin, the product of the Best vitelliform macular dystrophy gene (VMD2), localizes to the basolateral plasma membrane of the retinal pigment epithelium. Proc Natl Acad Sci U S A. 2000; 97:12758–63.
Article3. Deutman AF. Electro-oculography in families with vitelliform dystrophy of the fovea. Detection of the carrier state. Arch Ophthalmol. 1969; 81:305–16.4. Deutman AF, Hoyng CB, van Lith-Verhoeven. Macular dys-trophies / vitelliform dystrophy. Ryan SJ, Schachat AP, editors. Retina. 4th ed.Baltimore: Elsevier Mosby;2006. 2:chap. 64.5. Andrade RE, Farah ME, Costa RA. Photodynamic therapy with verteporfin for subfoveal choroidal neovascularization in best disease. Am J Ophthalmol. 2003; 136:1179–81.
Article6. Leu J, Schrage NF, Degenring RF. Choroidal neovascularisation secondary to Best's disease in a 13-year-old boy treated by intravitreal bevacizumab. Graefes Arch Clin Exp Ophthalmol. 2007; 245:1723–5.
Article7. Miyake Y, Shiroyama N, Horiguchi M, et al. Bull's-eye maculo-pathy and negative electroretinogram. Retina. 1989; 9:210–5.
Article8. Yannuzzi LA, Flower RW, Slakter JS. Central serous Chorio-retinopathy. Craven L, editor. Indocyanine green angiography. 1st ed.St. Louise: Mosby Co;1997. 1:chap. 22.9. Chan WM, Lam DS, Lai TY, et al. Treatment of choroidal neovas-cularization in central serous chorioretinopathy by photodynamic therapy with verteporfin. Am J Ophthalmol. 2003; 136:836–45.
Article10. Chan WM, Lai TY, Liu DT, Lam DS. Intravitreal bevacizumab (avastin) for choroidal neovascularization secondary to central serous chorioretinopathy, secondary to punctate inner choroido-pathy, or of idiopathic origin. Am J Ophthalmol. 2007; 143:977–83.
Article11. Spaide RF, Noble K, Morgan A, Freund KB. Vitelliform macular dystrophy. Ophthalmology. 2006; 113:1392–1400.
Article12. O'Gorman S, Flaherty WA, Fishman GA, Berson EL. Histo-pathologic findings in Best's vitelliform macular dystrophy. Arch Ophthalmol. 1988; 106:1261–8.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A case of Atypical Central Serous Chorioretinopathy with Bullous Retinal Detachment
- A Case of Central Serous Chorioretinopathy Following Systemic Corticosteroid Therapy
- A Seasonal Variation of Central Serous Chorioretinopathy
- A Case of Atypical Idiopathic Central Serous Chorioretinopathy
- A Case of Chronic Central Serous Chorioretinopathy Associated with Pituitary Adenoma