J Korean Surg Soc.
2012 Feb;82(2):87-93. 10.4174/jkss.2012.82.2.87.
Multivisceral resection for locally advanced rectal cancer: adequate length of distal resection margin
- Affiliations
-
- 1Department of Surgery, Chonnam National University Hospital, Gwangju, Korea. kyumyydaddy@naver.com
- KMID: 2212206
- DOI: http://doi.org/10.4174/jkss.2012.82.2.87
Abstract
- PURPOSE
Locally advanced rectal cancer may require an intraoperative decision regarding curative multivisceral resection (MVR) of adjacent organs. In bulky tumor cases, ensuring sufficient distal resection margin (DRM) for achievement of oncologic safety is very difficult. This study is designed to evaluate the adequate length of DRM in multiviscerally resected rectal cancer.
METHODS
A total of 324 patients who underwent curative low anterior resection for primary pT3-4 rectal cancer between 1995 and 2004 were identified from a prospectively collected colorectal database.
RESULTS
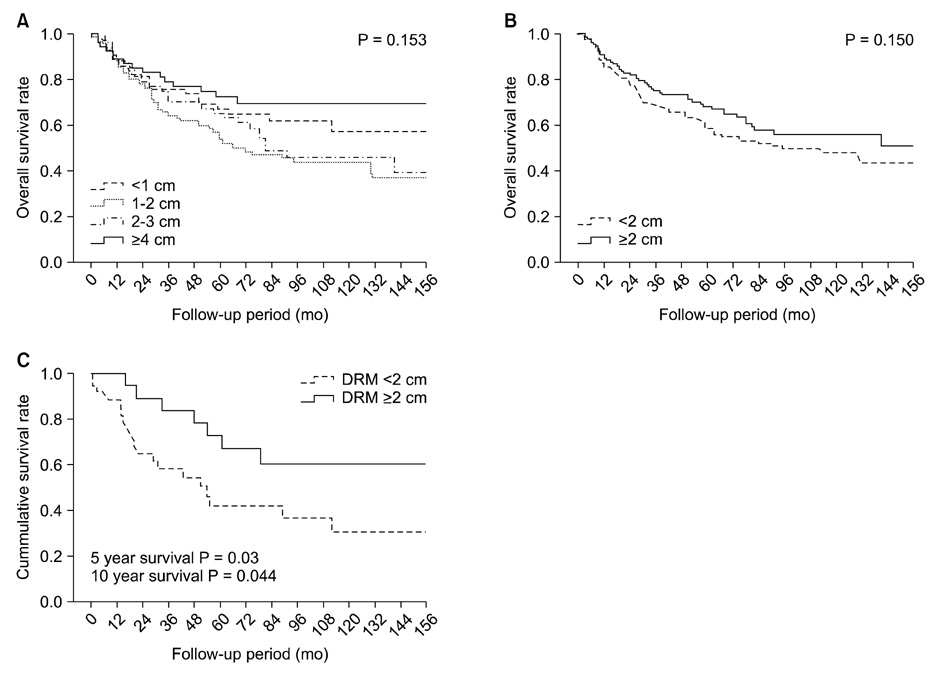
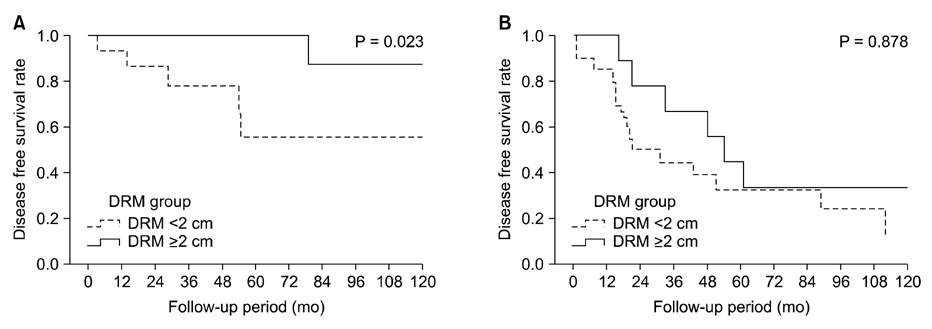
Short lengths of DRM (< or =1 cm) did not compromise essentially poor oncologic outcomes in locally advanced rectal cancer (P = 0.736). However, especially in rectal cancers invading adjacent organs, DRM of less than 2 cm showed poor survival outcome. In 5-year and 10-year survival analysis of MVR, a shorter DRM (<2 cm) showed 41.9% and 30.5%, although a longer DRM (> or =2 cm) showed 72.4% and 60.2% (P = 0.03, 0.044). In multivariate analysis of MVR, poorly differentiated histology, ulceroinfiltrative growth of tumor, and short DRM (<2 cm) were significant factors for prediction of poor survival outcome, although short DRM was not significantly related to local and systemic recurrence.
CONCLUSION
In locally advanced rectal cancer of pT3-4, a short length of DRM (< or =1 cm) did not compromise essentially poor oncologic outcome. In rectal cancers invading adjacent organs and requiring MVR, a shorter DRM (<2 cm) was found to be related to poor survival outcome.
Figure
Reference
-
1. Lehnert T, Methner M, Pollok A, Schaible A, Hinz U, Herfarth C. Multivisceral resection for locally advanced primary colon and rectal cancer: an analysis of prognostic factors in 201 patients. Ann Surg. 2002. 235:217–225.2. Lopez MJ. Multivisceral resections for colorectal cancer. J Surg Oncol. 2001. 76:1–5.3. National Comprehensive Cancer Network (NCCN). Colon cancer and rectal cancer guidelines, ver. 1. 2007. Washington: National Comprehensive Cancer Network (NCCN).4. Moore HG, Riedel E, Minsky BD, Saltz L, Paty P, Wong D, et al. Adequacy of 1-cm distal margin after restorative rectal cancer resection with sharp mesorectal excision and preoperative combined-modality therapy. Ann Surg Oncol. 2003. 10:80–85.5. Kwok SP, Lau WY, Leung KL, Liew CT, Li AK. Prospective analysis of the distal margin of clearance in anterior resection for rectal carcinoma. Br J Surg. 1996. 83:969–972.6. Guillem JG, Chessin DB, Shia J, Suriawinata A, Riedel E, Moore HG, et al. A prospective pathologic analysis using whole-mount sections of rectal cancer following preoperative combined modality therapy: implications for sphincter preservation. Ann Surg. 2007. 245:88–93.7. Birbeck KF, Macklin CP, Tiffin NJ, Parsons W, Dixon MF, Mapstone NP, et al. Rates of circumferential resection margin involvement vary between surgeons and predict outcomes in rectal cancer surgery. Ann Surg. 2002. 235:449–457.8. Lopez MJ, Monafo WW. Role of extended resection in the initial treatment of locally advanced colorectal carcinoma. Surgery. 1993. 113:365–372.9. Eisenberg SB, Kraybill WG, Lopez MJ. Long-term results of surgical resection of locally advanced colorectal carcinoma. Surgery. 1990. 108:779–785.10. Gall FP, Tonak J, Altendorf A. Multivisceral resections in colorectal cancer. Dis Colon Rectum. 1987. 30:337–341.11. Heslov SF, Frost DB. Extended resection for primary colorectal carcinoma involving adjacent organs or structures. Cancer. 1988. 62:1637–1640.12. Montesani C, Ribotta G, De Milito R, Pronio A, D'Amato A, Narilli P, et al. Extended resection in the treatment of colorectal cancer. Int J Colorectal Dis. 1991. 6:161–164.13. Pollett WG, Nicholls RJ. The relationship between the extent of distal clearance and survival and local recurrence rates after curative anterior resection for carcinoma of the rectum. Ann Surg. 1983. 198:159–163.14. Kim SJ, Choi YJ, Kang JG. Clinicopathologic analysis of mesorectal spread of rectal cancer with whole mount section. J Korean Surg Soc. 2010. 78:298–304.15. Kuvshinoff B, Maghfoor I, Miedema B, Bryer M, Westgate S, Wilkes J, et al. Distal margin requirements after preoperative chemoradiotherapy for distal rectal carcinomas: are < or = 1 cm distal margins sufficient? Ann Surg Oncol. 2001. 8:163–169.16. Kinoshita H, Watanabe T, Yanagisawa A, Nagawa H, Kato Y, Muto T. Pathological changes of advanced lower-rectal cancer by preoperative radiotherapy. Hepatogastroenterology. 2004. 51:1362–1366.17. Shirouzu K, Isomoto H, Kakegawa T. Distal spread of rectal cancer and optimal distal margin of resection for sphincter-preserving surgery. Cancer. 1995. 76:388–392.18. Williams NS, Dixon MF, Johnston D. Reappraisal of the 5 centimetre rule of distal excision for carcinoma of the rectum: a study of distal intramural spread and of patients' survival. Br J Surg. 1983. 70:150–154.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Analysis of the Prognostic Effectiveness of a Multivisceral Resection for Locally Advanced Colorectal Cancer
- Surgical issues in locally advanced rectal cancer treated by preoperative chemoradiotherapy
- Feasibility and Outcomes of Multivisceral Resection in Locally Advanced Colorectal Cancer: Experience of a Tertiary Cancer Center in North-East India
- Concomitant Adjacent Organ Resection in Locally Advanced Colon Cancer
- Robotic Partial Excision of Levator-Ani Muscle for Locally Advanced Low Rectal Cancer Invading Ipsilateral Pelvic Floor