J Korean Surg Soc.
2011 Sep;81(3):225-228. 10.4174/jkss.2011.81.3.225.
Tacrolimus related neurologic complication after pediatric kidney transplantation
- Affiliations
-
- 1Department of Surgery, Yeungnam University College of Medicine, Daegu, Korea. whkwun@med.yu.ac.kr
- KMID: 2212202
- DOI: http://doi.org/10.4174/jkss.2011.81.3.225
Abstract
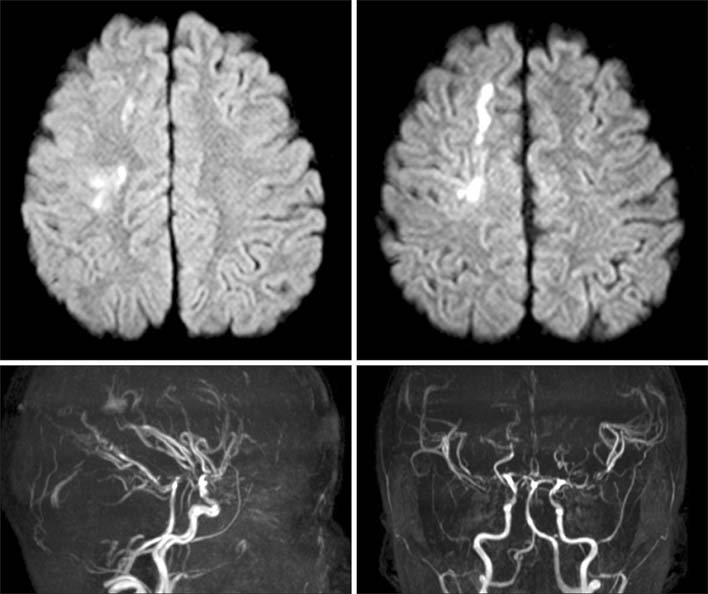
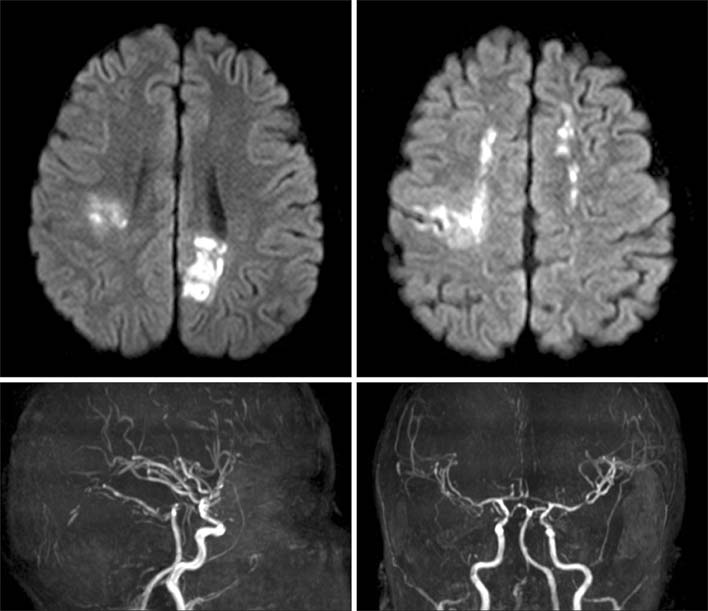
- Recently significant neurotoxicity has been reported with the use of carcineurin inhibitors. An 11-year-old-girl had undergone a transplantation of kidney from her mother. On post-operative day 12, hypertension, headache, and left motor weakness (grade I) suddenly occurred. The brain-magnetic resonance imaging and magnetic resonance angiography showed acute cerebral infarction at subcortical white matter of the right hemisphere and multiple stenoses of both anterior cerebral artery and middle cerebral artery. While stopping tacrolimus treatment, we experienced clinical and radiological improvement. So, the neurological complications of this patient seem to have been caused by the use of tacrolimus.
Keyword
MeSH Terms
Figure
Reference
-
1. Hinchey J, Chaves C, Appignani B, Breen J, Pao L, Wang A, et al. A reversible posterior leukoencephalopathy syndrome. N Engl J Med. 1996. 334:494–500.2. Casey SO, Sampaio RC, Michel E, Truwit CL. Posterior reversible encephalopathy syndrome: utility of fluid-attenuated inversion recovery MR imaging in the detection of cortical and subcortical lesions. AJNR Am J Neuroradiol. 2000. 21:1199–1206.3. Singh N, Bonham A, Fukui M. Immunosuppressive-associated leukoencephalopathy in organ transplant recipients. Transplantation. 2000. 69:467–472.4. Shin RK, Stern JW, Janss AJ, Hunter JV, Liu GT. Reversible posterior leukoencephalopathy during the treatment of acute lymphoblastic leukemia. Neurology. 2001. 56:388–391.5. Bartynski WS, Boardman JF. Catheter angiography, MR angiography, and MR perfusion in posterior reversible encephalopathy syndrome. AJNR Am J Neuroradiol. 2008. 29:447–455.6. McKinney AM, Short J, Truwit CL, McKinney ZJ, Kozak OS, SantaCruz KS, et al. Posterior reversible encephalopathy syndrome: incidence of atypical regions of involvement and imaging findings. AJR Am J Roentgenol. 2007. 189:904–912.7. Lee VH, Wijdicks EF, Manno EM, Rabinstein AA. Clinical spectrum of reversible posterior leukoencephalopathy syndrome. Arch Neurol. 2008. 65:205–210.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Risk of graft loss on once-daily versus twice-daily tacrolimus in kidney transplant patients: a meta-analysis
- Posterior Reversible Encephalopathy Syndrome Improved by Changing Immunosuppressant from Calcineurin Inhibitor to Sirolimus in a Kidney Transplantation Recipient
- Determination of tacrolimus dosage using machine learning in kidney transplantation
- The comparison of coefficient of variation among once-daily and twice-daily tacrolimus in kidney transplant patients: a meta-analysis
- Modified Release Tacrolimus