J Korean Ophthalmol Soc.
2009 Jan;50(1):172-175. 10.3341/jkos.2009.50.1.172.
A Case of Parinaud Syndrome After Intracranial Hemorrhage
- Affiliations
-
- 1Department of Ophthalmology, Inha University College of Medicine, Incheon, Korea. ksm0724@medimail.co.kr
- KMID: 2211914
- DOI: http://doi.org/10.3341/jkos.2009.50.1.172
Abstract
- PURPOSE
To report one case of Parinaud syndrome after intracranial hemorrhage.
CASE SUMMARY
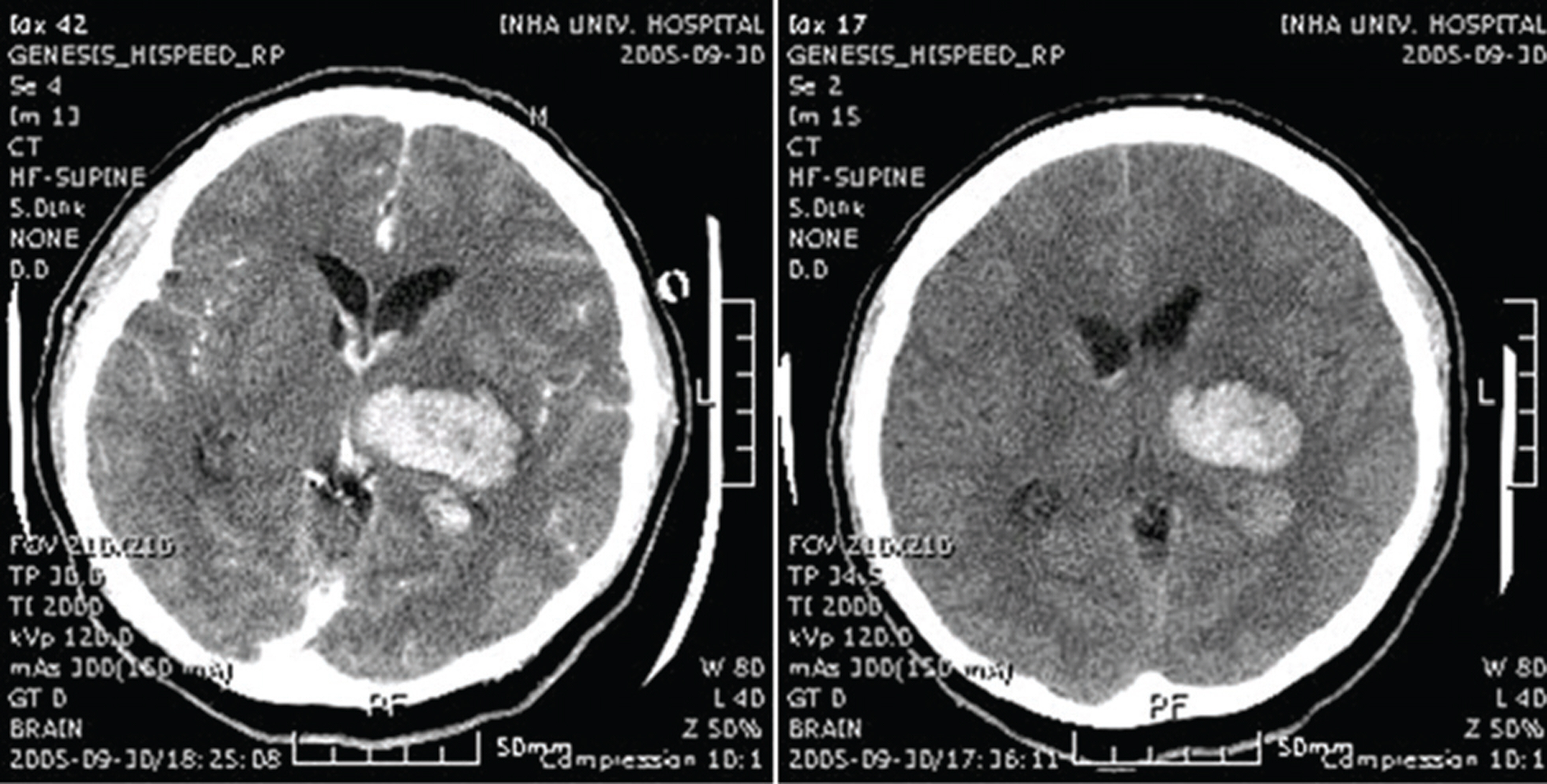
A 45-year-old man visited our emergency department complaining of right-sided weakness and right-sided hypoesthesia. Intracranial hemorrhage in the left thalamus and intraventricular hemorrhage were noted upon brain computed tomography, and the patient was admitted to the department of neurosurgery. He complained of diplopia and upgaze palsy, and he was referred to the department of ophthalmology. The patient exhibited convergence-retraction nystagmus, light-near dissociation and vertical gaze limitation within 15 degrees. The best-corrected visual acuity of both eyes was 20/20, but convergence-retraction nystagmus and light-near dissociation still remained. Upgaze palsy was also not improved.
CONCLUSIONS
Once symptoms manifest, Parinaud syndrome does not resolve except in patients with hydrocephalus. If the findings persist for more than 6 months, the likelihood of complete resolution is very small. We reported a case of typical Parinaud syndrome with upgaze palsy, convergence-retraction nystagmus and light-near dissociation after thalamic and intraventricular hemorrhage.
MeSH Terms
Figure
Reference
-
References
1. Pearce JM. Parinaud’s syndrome. J Neurol Neurosurg Psychiatry. 2005; 76:99.
Article2. Menon A, Sreedhar A, Anilkumar D, Ittyerah TP. Parinaud's syndrome in a patient with thalamic infarction due to cerebral venous thrombosis. Indian J Ophthalmol. 2007; 55:237–8.
Article3. Bhola R, Olson RJ. Dorsal midbrain syndrome with bilateral superior oblique palsy following brainstem hemorrhage. Arch Ophthalmology. 2006; 124:1786–8.
Article4. Schmidtke K, Buttner-Ennever JA. Nervous control of eyelid function. A review of clinical, experimental and pathological data. Brain. 1992; 115:227–47.5. Jouvent E, Benity S, Fenelon G. . Convergence nystagmus and vertical gaze palsy of vascular origin. Rev Neurol (Paris). 2005; 161:593–5.6. Buuttner U, buuttner-Ennever JA, Rambold H, Helmchen C. The Contribution of midbrain circuits in the control of gaze. Ann N Y Acad Sci. 2002; 956:99–110.7. Miller NR. Late improvement in upward gaze in a patient with hydrocephalus related Parinaud dorsal midbrain syndrome. Br J Ophthalmol. 2006; 90:123.
Article8. Moon SY, Park SH, Hwang JM. . Multiple Germ Cell Tumors Manifesting as Anterior Hypothalamic and Pretectal Syndromes. J Korean Neurol Assoc. 2005; 23:264–7.9. Wilhelm BJ, Wilhelm H, Moro S, Barbur JL. Pupil response components: studies in patients with Parinaud’s syndrome. Brain. 2002; 125:2296–307.
Article10. Buckley EG, Holgado S. Surgical Treatment of Upgaze Palsy in Parinaud’s Syndrome. J AAPOS. 2004; 8:249–53.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A case of fetal intracranial hemorrhage diagnosed by antenatal ultrasonographic examination
- A Case Report of Osler-Rendu-Weber Syndrome
- Oculo-Cerebral Syndrome after Spontaneous Subarachnoid Hemorrhage
- A Case of Takayasu's Arteritis Associated with Subarachnoid Hemorrhage and Intracranial Aneurysm: Case Report
- Delayed Vasospasm after Aneurysmal Subarachnoid Hemorrhage in Behcet Syndrome