J Korean Ophthalmol Soc.
2007 Oct;48(10):1323-1328. 10.3341/jkos.2007.48.10.1323.
Comparison of Hydrogel and Silicone Hydrogel Bandage Contact Lens after LASEK
- Affiliations
-
- 1Department of Ophthalmology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. tychung@smc.samsung.co.kr
- KMID: 2210984
- DOI: http://doi.org/10.3341/jkos.2007.48.10.1323
Abstract
-
PURPOSE: To compare the effectiveness between wearing a conventional hydrogel vifilcon A bandage contact lens (BCL) and a silicone hydrogel lotrafilcon A BCL after laser-assisted subepithelial keratomileusis (LASEK).
METHODS
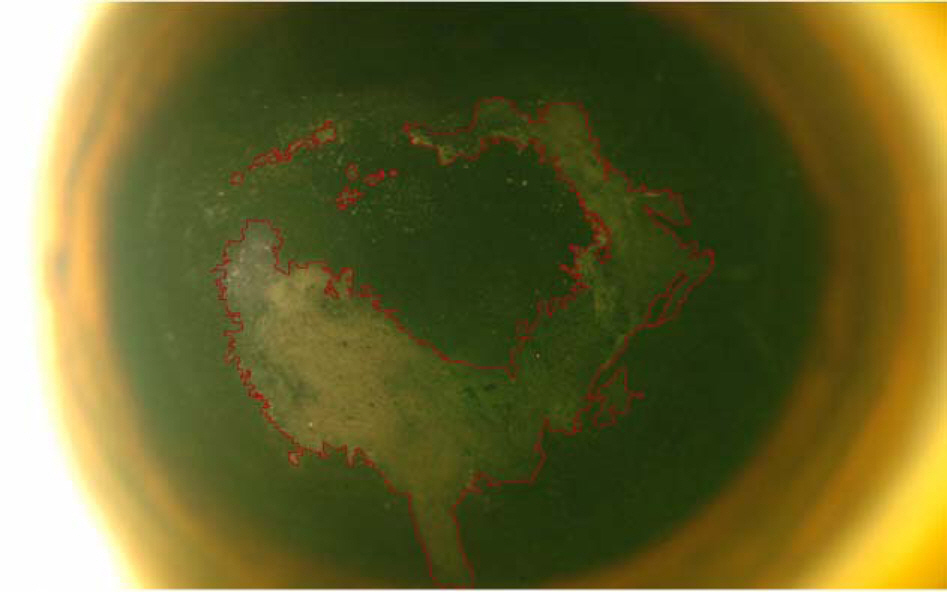
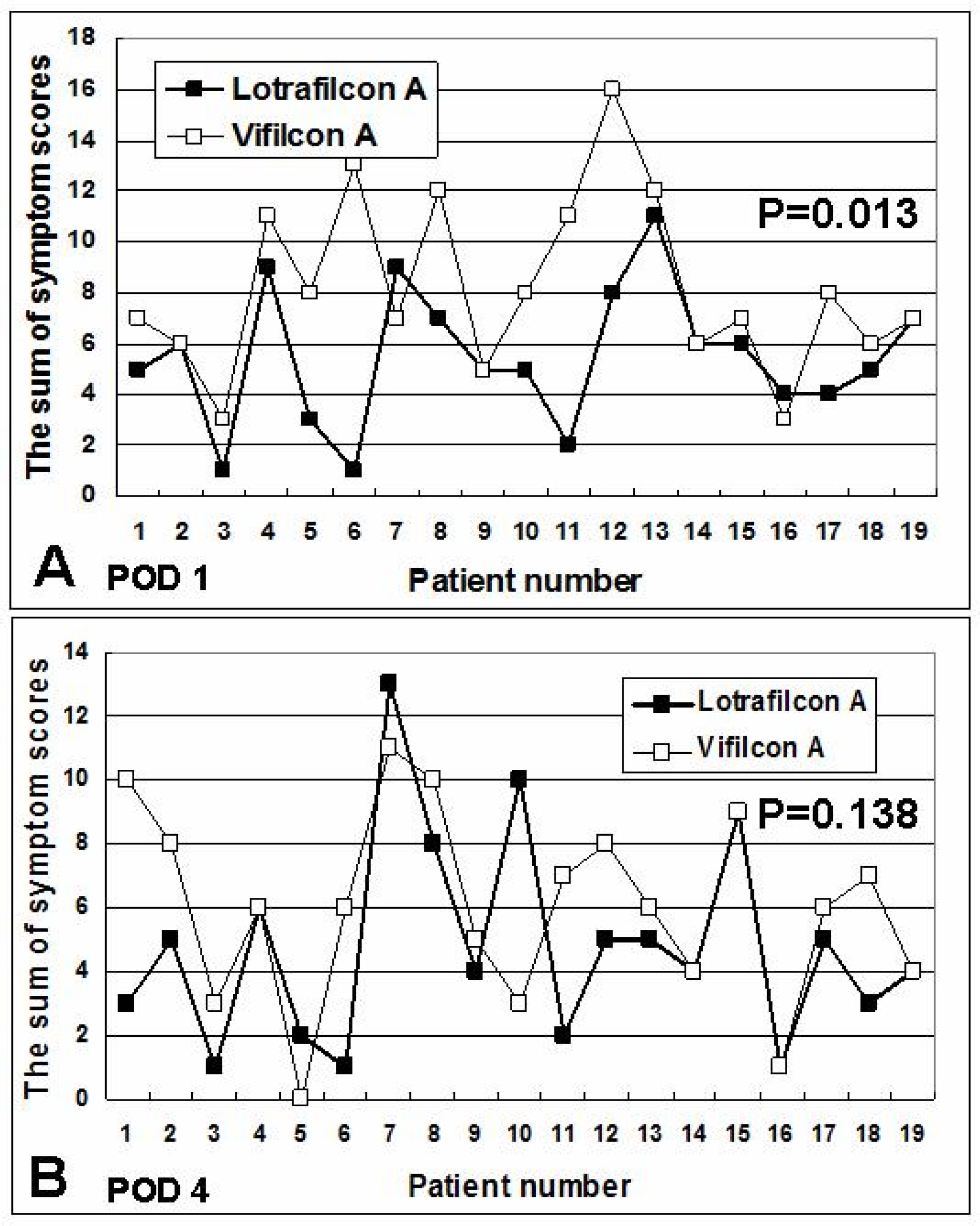
LASEK was performed on 38 eyes of 19 patients. Each patient was fitted with a silicone hydrogel lotrafilcon A lens in one eye and a conventional hydrogel vifilcon A lens in the other eye. The patient was masked on the type of lens in each eye. General preference between the two types of lenses, subjective symptoms (pain, photophobia, tearing, dryness, and foreign body sensation; graded as 0 to 4), and the area of non-viable corneal epithelium were assessed in each eye at one and four days after surgery.
RESULTS
Patients reported preferring the lotrafilcon A lens to vifilcon A at 1 (79%) and 4 (74%) days after LASEK. The mean symptom scores of tearing and foreign body sensation at 1 day after surgery (P=0.012 and P=0.034, respectively) and foreign body sensation at 4 days after surgery (P=0.027) were significantly lower in the lotrafilcon A group. The mean area of the non-viable corneal epithelium was smaller in the lotrafilcon A lens group at 1 day and 4 days after surgery, although not statistically significant.
CONCLUSIONS
Patients better tolerated the silicone hydrogel lotrafilcon A BCL compared with the conventional hydrogel vifilcon A BCL. The mean symptom scores were significantly lower in the lotrafilcon A group at both 1 and 4 days after LASEK.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Dastjerdi MH, Soong MK. LASEK (laser subepithelial keratomileusis). Curr Opin Ophthalmol. 2002; 13:261–3.
Article2. Anderson NJ, Beran RF, Sohneider TL. Epi-LASEK for the correction of myopia and myopic astigmatism. J. Cataract Refract Surg. 2002; 28:1343–7.
Article3. Litwak S, Zadok D, Garcia-de Quevedo V, et al. Laser-assisted subepithelial keratectomy versus photorefractive keratectomy for the correction of myopia. A prospective comparative study. J Cataract Refract Surg. 2002; 28:1330–3.4. Bergenske P, Caroline P, Smithe J. Contact lenses as an adjunct in refractive surgery practice. CL Spectrum. 2002; 17:30–7.5. Duane TD. Therapeutic hydrogel lenses. In : Duane TD, editor. Clinical Ophthalmology. New York: Harper & Row;1978. v. 4. chap. 10.6. Gould HL. Therapeutic experiences with soft contact lenses. Trans Am Acad Ophthalmol Otolaryngol. 1974; 78:391.7. Duke-Elder S. System of Ophthalmology. 5. Philadelphia: C.V. Mosby;1970. p. 786.8. Sampson WG. Symposium; Soft contact lenses. Trans Am Acad Ophthalmol Otolaryngol. 1974; 78:383.9. Szaflik JP, Ambroziak AM, Szaflik J. Therapeutic use of a lotrafilcon A silicone hydrogel soft contact lens as a bandage after LASEK surgery. Eye Contact Lens. 2004; 30:59–62.
Article10. Lim L, Tan DT, Chan WK. Therapeutic use of Bausch & Lomb PureVision contact lenses. CLAO J. 2001; 27:179–85.11. Engle AT, Laurent JM, Schallhorn SC, et al. Masked comparison of silicone hydrogel lotrafilcon A and etafilcon A extended-wear bandage contact lenses after photorefractive keratectomy. J Cataract Refract Surg. 2005; 31:681–6.
Article12. Lee JH, Do SJ. Therapeutic uses of T-lens (Soflens) in corneal diseases. J Korean Ophthalmol Soc. 1983; 24:269–72.13. Leibowitz HM. Hydrophilic contact lenses in corneal disease, IV. Penetrating corneal wounds. Arch Ophthalmol. 1972; 88:602.14. Dohlman C, Boruchoff S, Mobilia E. Complications in use of soft contact lenses in corneal disease. Arch Ophthalmol. 1973; 90:367–71.
Article15. Tighe B. Silicone hydrogels-what are they and how should they be used in everyday practice? Optician. 1999; 218:31–2.16. Montero J, Sparholt J, Mely R. Retrospective case series of therapeutic applications of a lotrafilcon A silicone hydrogel soft contact lens. Eye Contact Lens. 2003; 29:S54–6.
Article17. Dumbleton K, Chalmers R, Richter D. Vascular response to extended wear of hydrogel lenses with high and low oxygen permeability. Optom Vis Sci. 2001; 78:147–51.
Article18. Ren D, Yamamoto K, Ladage PM, et al. Adaptive effects of 30-night wear of hyper-02 transmissible contact lenses on bacterial binding and corneal epithelium. Ophthalmology. 2002; 109:127–39.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Characteristics of Silicone Hydrogel Contact Lenses Commercially Available in Korea
- The Effects of Cheap Tinted Contact Lenses on Corneal Swelling and Ocular Surface Inflammation
- The Effect of Corneal Edema on Corneal Topography
- Corneal Edema Induced by Balafilcon A Contact Lens in Rabbits
- Clinical Features after Rupture of Hydrogel Breast Implants - MDbP206