J Korean Soc Spine Surg.
2002 Dec;9(4):356-363. 10.4184/jkss.2002.9.4.356.
Functional Outcome of the Surgical Correction of Neuromuscular Scoliosis
- Affiliations
-
- 1Department of Orthopaedic Surgery, College of Medicine, St. Vincent's Hospital, Korea.
- 2Department of Orthopaedic Surgery, College of Medicine, Kang-Nam St. Mary's Hospital, Korea. kyh@cmc.cuk.ac.kr
- KMID: 2209718
- DOI: http://doi.org/10.4184/jkss.2002.9.4.356
Abstract
-
STUDY DESIGN: A retrospective study of functional outcome after surgical correction of neuromuscular scoliosis.
OBJECTIVES
To assess functional outcomes and their significances after the surgical correction of neuromuscular scoliosis. SUMMARY OF LITERATURE REVIEW: The surgical correction of neuromuscular scoliosis has been used to stabilize the trunk for balanced sitting, to improve cardiopulmonary function, and the function of the upper extremities. Many authors have reported favorable surgical results, but few studies have been undertaken on functional assessment after surgery.
MATERIALS AND METHODS
Eighteen adult patients with neuromuscular scoliosis underwent surgical correction. Functional assessments were performed in terms of impairments, disabilities, and handicaps. The impairments included sitting ability, coronal Cobb's angle, pain after surgery, and cosmesis after surgery. The disabilities included dressing, feeding, toilet/bathing, locomotion, and the use of both hands, and the handicaps included the effort and time to care for patients. Each parameter was checked preoperatively, 6 months after surgery, and at the last follow-up.
RESULTS
In terms of impairments, sitting ability, coronal Cobb's angle, pain, and cosmesis were improved by surgery. In terms of disabilities, dressing, toilet/bathing, and locomotion were not improved after surgical correction. However, the feeding and use of both hands were significantly improved. And, in terms of handicaps, both the effort and the time required for care were reduced post-surgically.
CONCLUSIONS
We conclude that impairments, handicaps, and the functions of the upper extremities were improved after surgical intervention to stabilize the trunk and spine in cases of neuromuscular scoliosis, but that overall disabilities were unaffected. This latter apparent shortcoming is attributed to the inability of surgery to treat previous systemic disease affecting physical disabilities of lower extremities. However, surgical correction of neuromuscular scoliosis was found to be clinically significant in terms of improving the functions of the trunk and of the upper extremities.
MeSH Terms
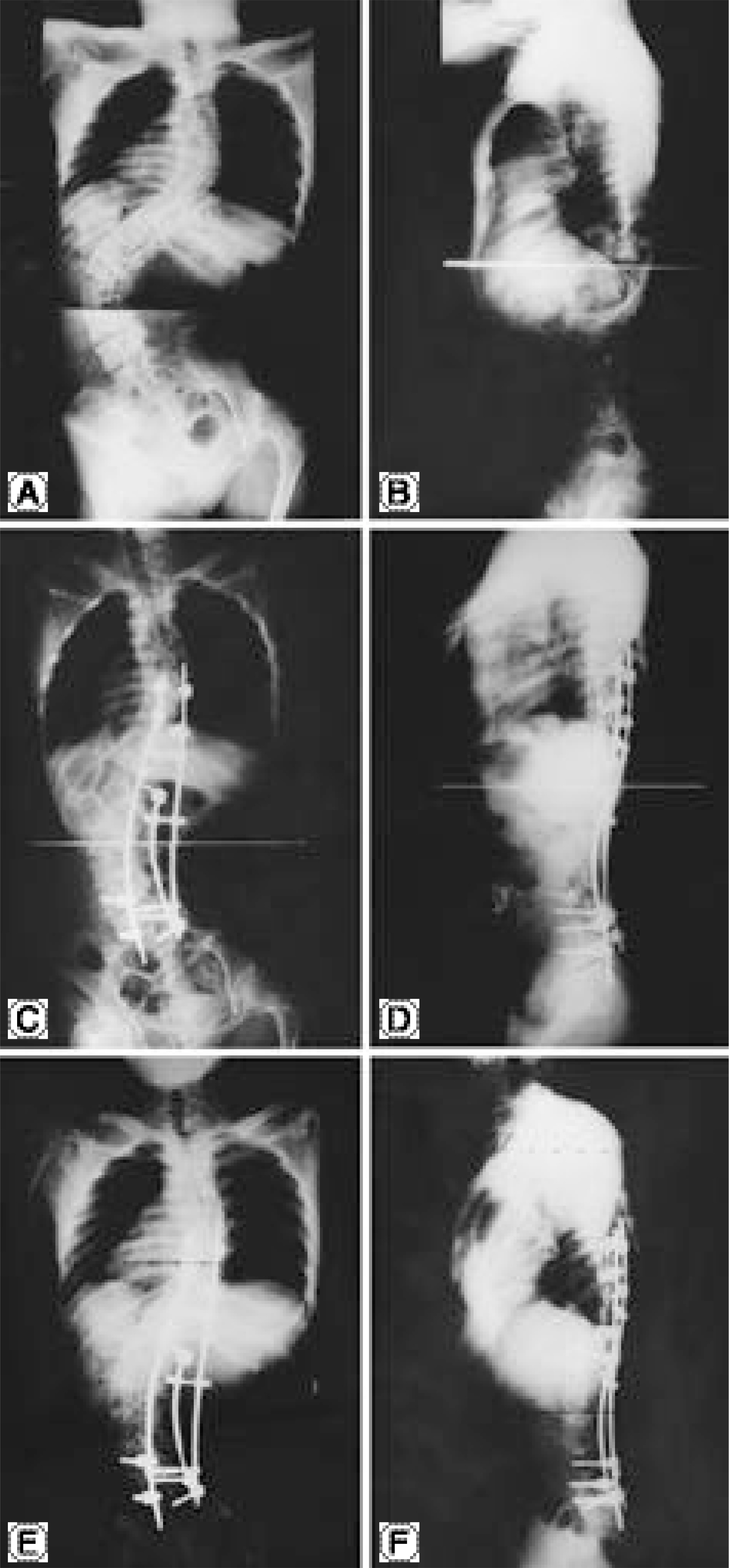
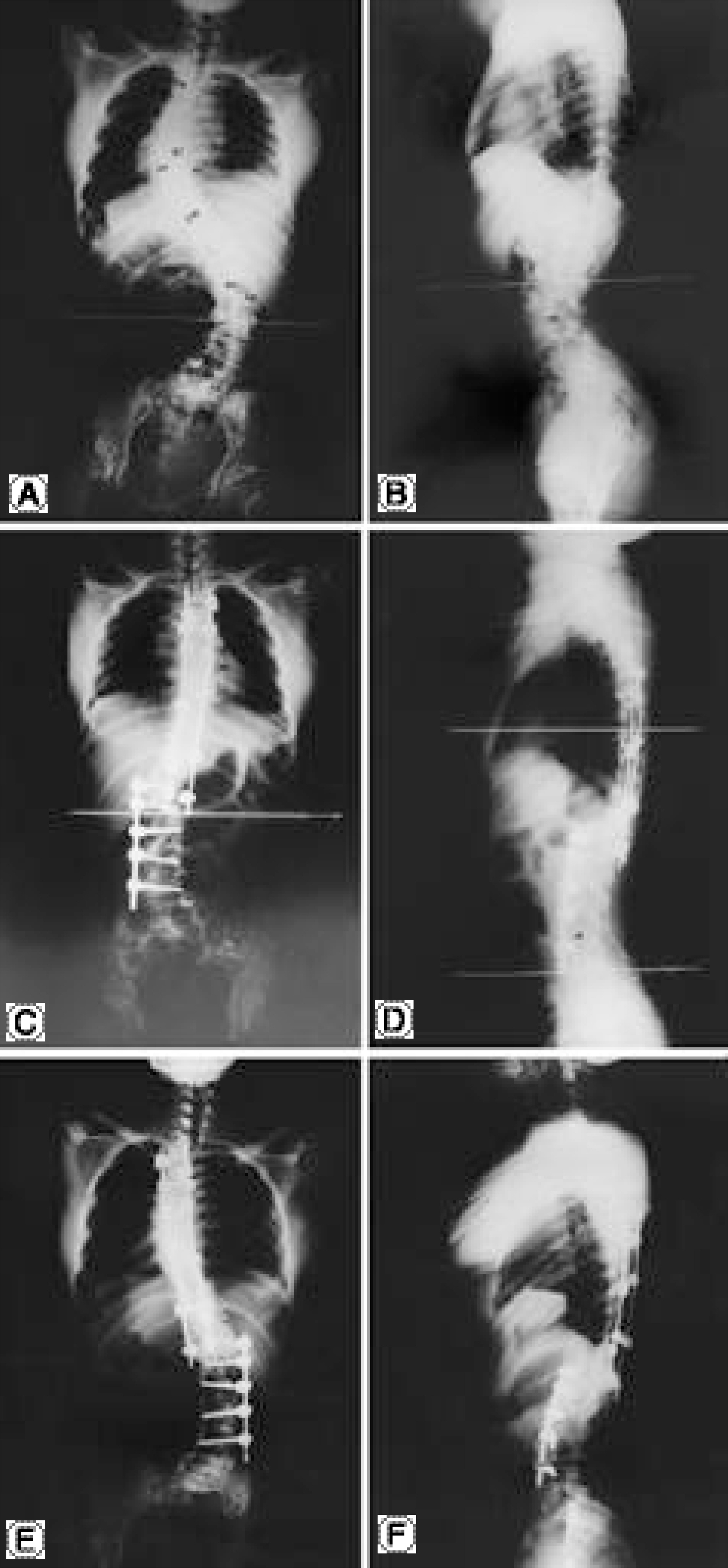
Figure
Reference
-
1). Askin GN, Hallett R, Hare N and Webb JK. The outcome of scoliosis surgery in the severely physically handicapped child. Spine. 22:44–50. 1997.
Article2). De Giorgi G, Stella G, Becchetti S, Martucci G and Miscioscia D. Cotrel-Dubousset instrumentation for the treatment of severe scoliosis. Eur Spine. 8:8–15. 1999.
Article3). Garrett AL, Perry J and Nickel V. Stabilization of the collapsing spine. J Bone J Surg. 43-A:474–484. 1961.
Article4). Hallett R, Hare N and Milner AD. Description and evaluation of an assessment form. Physiotherapy. 73:220–225. 1987.5). Hensinger RN and MacEween GD. Spinal deformity associated with heritable neurological conditions: Spinal muscular atrophy. Friedreich's ataxia, familial dysau -tonomia and Charcot-Marie-Tooth disease. J Bone Joint Surg. 58-A:13–24. 1976.6). Hibbs RA. A report of fifty-nine cases of scoliosis treated by the fusion operation. J Bone Joint Surg. 6-A:15. 1924.7). Larsson E-L, Aaro S and Oberg B. Activities and functional assessment 1 year after spinal fusion for paralytic scoliosis. Eur Spine J. 8:100–109. 1999.
Article8). Lonstein JE and Akbarnia RA. Operative treatment of spinal deformities in patients with cerebral palsy or men -tal retardation. J Bone Joint Surg. 65-A:43–55. 1983.9). Mazur J, Menelaus M, Dickens DRV and Doig WG. Efficacy of surgical management for scoliosis in myelomeningocele: Correction of deformity and alteration of functional status. J Pediatr Orthop. 6:568–75. 1986.
Article10). McMaster MJ. Anterior and posterior instrumentation and fusion of thoracolumbar scoliosis due to myelomeningocele. J Bone Joint Surg. 69-B:20–5. 1987.
Article11). Mulcahy CM, Pountney TE, Nelham RL, Green EM and Billington GD. Adapting seating for motor handicap: problems, a solution, assessment and prescription. Br J Occup Ther. 51:347–352. 1988.12). Rhyu K and Ha K. Clinical outcome after surgical correction of severe scoliosis. J Korean Orthop Assoc. 36(1):39–44. 2001.
Article13). Samuelsson K, Larsson E-L, Normelli H, Oberg B, Aaro S and Tropp H. Development of an instrument for clinical evaluation after surgery for neuromuscular scoliosis. Eur Spine J. 5:400–406. 1996.
Article14). Stanitsky CL, Micheli LJ, Hall JE and Rosenthal RK. Surgical correction of spinal deformity in cerebral palsy. Spine. 7:563–9. 1982.
Article15). Sussman MD, Little D, Alley RM and McCoig JA. Posterior instrumentation and fusion of the thoracolumbar spine for treatment of neuromuscular scoliosis. J Pediatr Orthop. 16:304–313. 1996.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Outcome After Surgical Correction of Severe Scoliosis
- Clinical Issues in Indication, Correction, and Outcomes of the Surgery for Neuromuscular Scoliosis: Narrative Review in Pedicle Screw Era
- Correction of the Dorsal Contour Deformity Caused by Scoliosis with Silicone Implant
- Segmental Spinal Instrumentation in the Treatment of Scoliosis
- A Clinical Study of Scoliosis