J Korean Soc Radiol.
2013 Sep;69(3):181-185. 10.3348/jksr.2013.69.3.181.
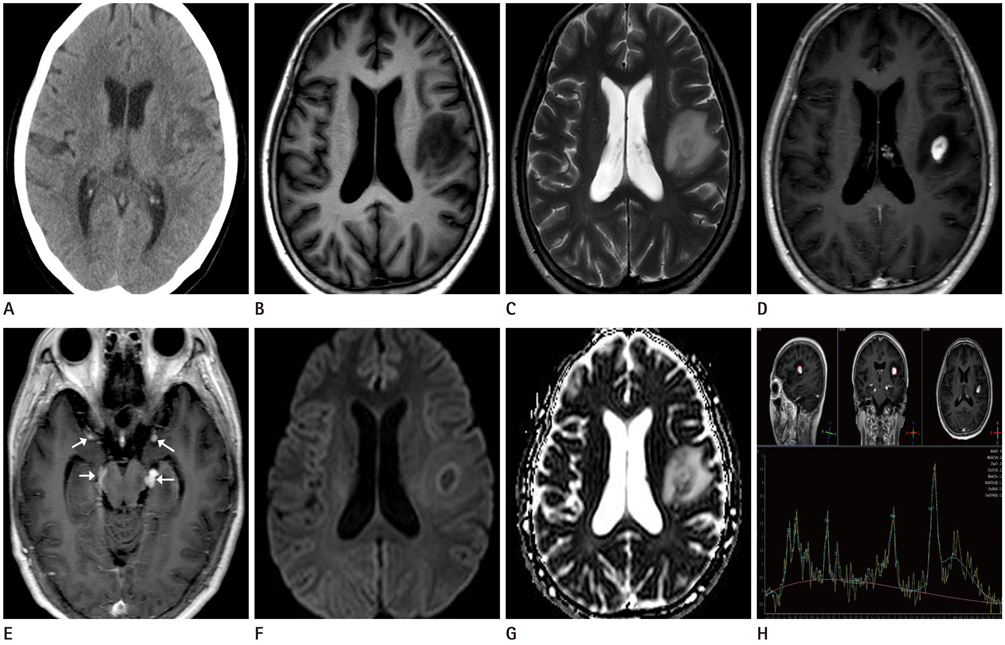
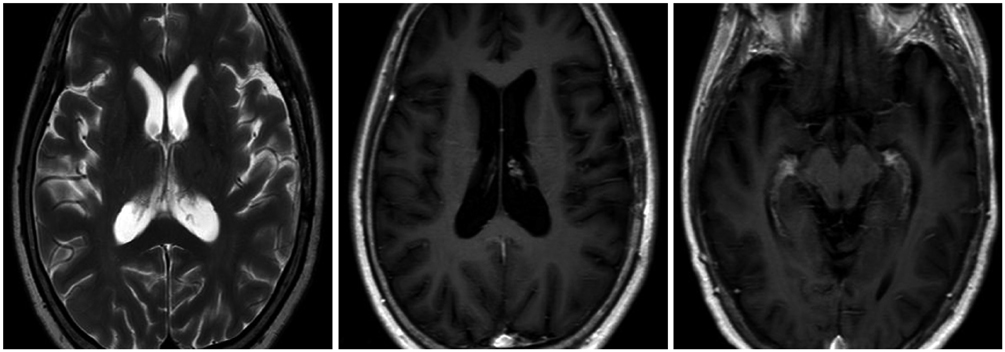
Cerebral Gumma Mimicking a Brain Tumor in a Human Immunodeficiency Virus-Negative Patient: A Case Report
- Affiliations
-
- 1Department of Radiology, Haeundae Paik Hospital, Inje University College of Medicine, Busan, Korea. sartre81@gmail.com
- 2Department of Physical Medicine and Rehabilitation, Haeundae Paik Hospital, Inje University College of Medicine, Busan, Korea.
- KMID: 2208798
- DOI: http://doi.org/10.3348/jksr.2013.69.3.181
Abstract
- Syphilis has a broad spectrum of clinical manifestations, and the cerebral gumma is a kind of neurosyphilis which is rare and can be cured by appropriate antibiotic treatments. However, in clinical practices, diagnosis of cerebral syphilitic gumma is often difficult because imaging and laboratory findings revealed elusive results. Herein, we present a rare case of neurosyphilis presenting as cerebral gumma confirmed by histopathological examination, and positive serologic and cerebrospinal fluid analyses. This case report suggests that cerebral gumma should be considered as possible diagnosis for human immunodeficiency virus-negative patients with space-occupying lesion of the brain. And this case also provides importance of clinical suspicions in diagnosing neurosyphilis because syphilis serology is not routinely tested on patients with neurologic symptoms.
MeSH Terms
Figure
Reference
-
1. Lee CW, Lim MJ, Son D, Lee JS, Cheong MH, Park IS, et al. A case of cerebral gumma presenting as brain tumor in a human immunodeficiency virus (HIV)-negative patient. Yonsei Med J. 2009; 50:284–288.2. Yoon YK, Kim MJ, Chae YS, Kang SH. Cerebral syphilitic gumma mimicking a brain tumor in the relapse of secondary syphilis in a human immunodeficiency virus-negative patient. J Korean Neurosurg Soc. 2013; 53:197–200.3. Jeong YM, Hwang HY, Kim HS. MRI of neurosyphilis presenting as mesiotemporal abnormalities: a case report. Korean J Radiol. 2009; 10:310–312.4. Lee MA, Aynalem G, Kerndt P, Tabidze I, Gunn R, Olea L, et al. Symptomatic Early Neurosyphilis Among HIV-Positive Men Who Have Sex With Men-Four Cities, United States, January 2002-June 2004S. JAMA. 2007; 298:732–734.5. Fargen KM, Alvernia JE, Lin CS, Melgar M. Cerebral syphilitic gummata: a case presentation and analysis of 156 reported cases. Neurosurgery. 2009; 64:568–575. discussion 575-576.6. Simon RP. Neurosyphilis. Arch Neurol. 1985; 42:606–613.7. Berger JR, Waskin H, Pall L, Hensley G, Ihmedian I, Post MJ. Syphilitic cerebral gumma with HIV infection. Neurology. 1992; 42:1282–1287.8. Agrons GA, Han SS, Husson MA, Simeone F. MR imaging of cerebral gumma. AJNR Am J Neuroradiol. 1991; 12:80–81.9. Vogl T, Dresel S, Lochmüller H, Bergman C, Reimers C, Lissner J. Third cranial nerve palsy caused by gummatous neurosyphilis: MR findings. AJNR Am J Neuroradiol. 1993; 14:1329–1331.10. Al-Okaili RN, Krejza J, Wang S, Woo JH, Melhem ER. Advanced MR imaging techniques in the diagnosis of intraaxial brain tumors in adults. Radiographics. 2006; 26 Suppl 1:S173–S189.11. Soares-Fernandes JP, Ribeiro M, Maré R, Magalhães Z, Lourenço E, Rocha JF. Diffusion-weighted magnetic resonance imaging findings in a patient with cerebral syphilitic gumma. J Comput Assist Tomogr. 2007; 31:592–594.12. Suarez JI, Mlakar D, Snodgrass SM. Cerebral syphilitic gumma in an HIV-negative patient presenting as prolonged focal motor status epilepticus. N Engl J Med. 1996; 335:1159–1160.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Cerebral Gumma Presenting as Brain Tumor in a Human Immunodeficiency Virus (HIV)-Negative Patient
- Cerebral Syphilitic Gumma Mimicking a Brain Tumor in the Relapse of Secondary Syphilis in a Human Immunodeficiency Virus-Negative Patient
- A Case of Ankylosing Spondylitis in a Patient with Human Immunodeficiency Virus
- Human Immunodeficiency Virus-Associated Multiple Cerebral Aneurysmal Vasculopathy in a Young Adult: A Case Report
- Cerebral Syphilitic Gummata Mimicking Metastatic Brain Tumors